This article has been verified for CPD. Click the button below to answer a few
short questions and download a form to be included in your CPD folder.
The anatomical understanding of the periorbital ligaments is critical for mastering tear trough treatments, perhaps more important than in any other non-surgical facial treatment.
Knowledge of this region’s anatomy can prevent complications, improve patient outcomes, and build injection confidence. Here is a brief introduction to the key infraorbital ligaments and their significance for under-eye treatments involving hyaluronic acid filler.
Tear trough ligament
The tear trough ligament is the superstar of the region and should be the number one focus when managing infraorbital complaints. Like most ligaments in the region, this ligament is osteocutaneous, meaning it originates from bone and attaches to the skin, which results in the infraorbital region’s characteristic medial groove [1]. Most complaints from patients will involve this ligament, and it will feature prominently in cases of under-eye hollows or often in framing infraorbital bags [2].
The ligament’s main function is to tether the orbicularis oculi muscle and malar fat pads to the maxilla (cheekbone). It is important to clarify that contrary to popular misconception, the ligament is only about 5-7mm in length and extends from the medial canthus to the mid-pupillary line, at which point it becomes the orbital-retaining ligament [1]. Targeting this ligament will normally take one of two forms. In my experience, at a deeper level, a small amount of hyaluronic acid filler can minimise groove appearance caused by the ligament. A more superficial, subcision-like technique, on the other hand, can further improve the medial infraorbital region without the need to add volume. While subcision refers to a slightly different technique used to treat acne scars, the premise here is similar: using a blunt cannula in the subcutaneous layer can reduce the tethering of the skin to the ligament by breaking some of those attachments.
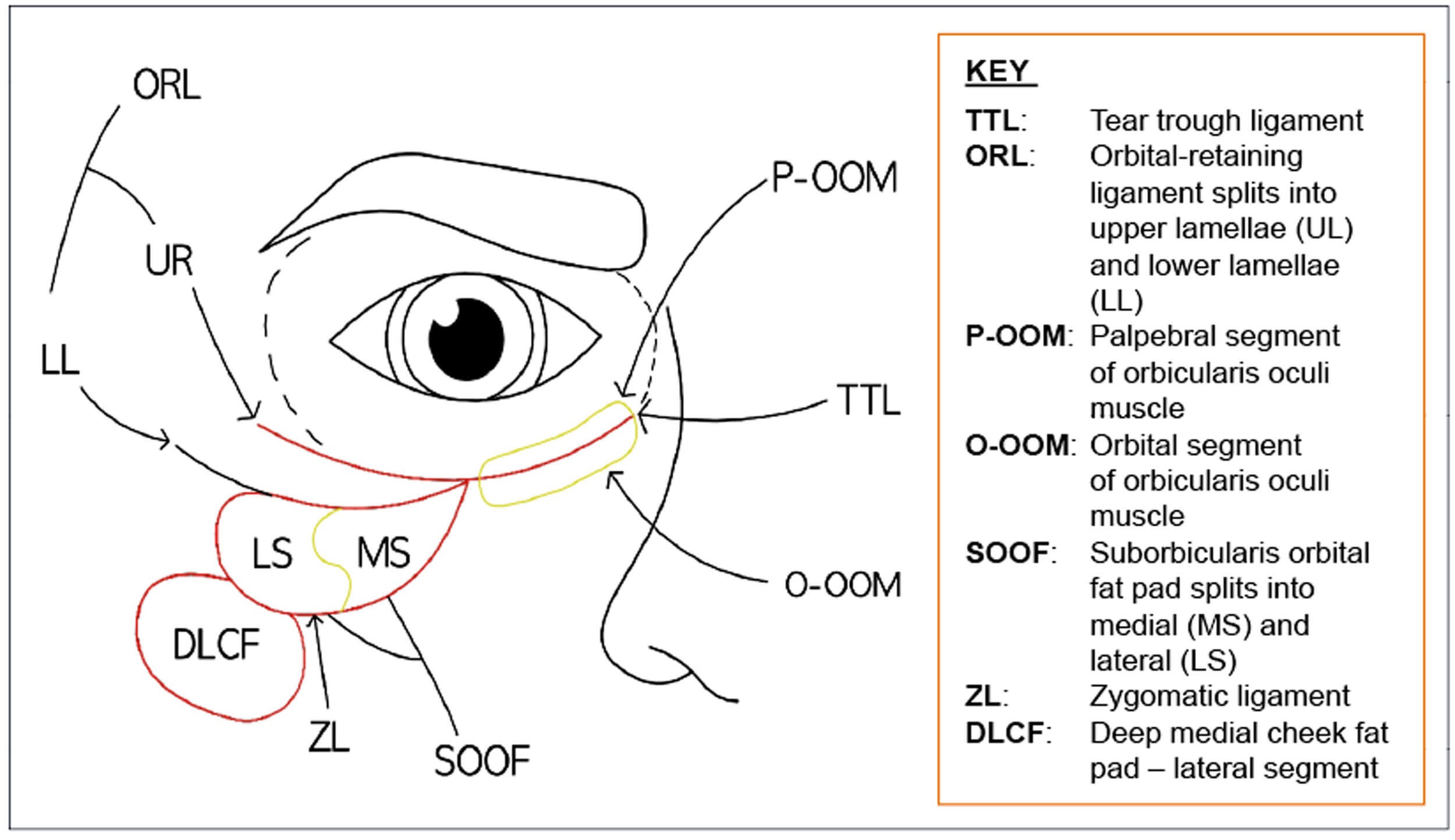
Figure 1: Diagram demonstrating the anatomical features of the tear trough.

Figure 2: Image of patient demonstrating the locations of the nasojugal groove (NJG),
the tear trough (TT) groove, the palpebromalar groove (PMG) and the mid-cheek groove (MCG).
Orbital-retaining ligament
The orbital-retaining ligament is a continuation of the tear trough ligament and splits into two parts. It starts at the mid-pupillary line and extends roughly 15mm laterally [3]. The ligament mainly serves to attach the orbicularis oculi muscle to the orbital rim and also forms the superior border of the suborbicularis orbital fat pad (SOOF) [3].
There is a common misconception that this ligament is the sole anatomical foundation of the palpebromalar groove; however, the origin of this groove is mainly thought to be due to atrophy of subcutaneous fat in the region coupled with fixation by the orbital-retaining ligament [4]. From a clinical perspective, this ligament is of concern to patients exhibiting a prominent palpebromalar groove.
Treatment of this region requires far more caution than the tear trough region for a few reasons. Primarily, the added component of superficial fat loss means that managing the actual problem requires some volume augmentation in the subcutaneous plane, which comes with inherent cosmetic risks of lumps and Tyndall effect when performed in the infraorbital region [2].
Additionally, just beneath this ligament is an area known as the prezygomatic space, which notoriously can lead to malar mounds if mismanaged with dermal fillers [5]. It is for this reason that I stress not filling between the midline and the lateral canthus; in my opinion, all enhancements in this region should come from treating the cheeks, either in the zygoma region or below the zygomatic ligament.
Zygomatic ligament
The zygomatic ligament originates laterally at McGregor’s Patch and forms the inferior border of the prezygomatic space [5]. It appears continuous with the tear trough ligament, though it is not.
This ligament is osteocutaneous and manifests in patients as an apparent mid-cheek groove. Typically, this presentation will appear in conjunction with a pronounced tear trough groove [6]. It is important to recognise that the strength of these ligaments from bone to skin relies heavily on genetics, so these patients may present at any age [6]. The ageing process can certainly exaggerate these attachments, however, a skilled practitioner must be able to manage these concerns when treating young patients, for whom adding volume may be inappropriate as they do not demonstrate any volume loss.
In the case where there is clear volume loss of the cheek accompanied with infraorbital concerns, it would then be sensible to add volume on the bone of this region using a needle and bolus technique. Any decision to inject above the zygomatic ligament should be made with caution, as the pre-zygomatic space is prone to post-treatment complications and often manifests in malar mounds [7]. If your best clinical judgment indicates that you treat the cheeks above the zygomatic ligament, then injections directly onto bone are likely to be the least complication prone.
In patients where cheek augmentation is not indicated, you may want to consider subcision-like techniques using a cannula in the region. Similar to the tear trough region, in my experience, using a cannula in the superficial planes to add some separation between the ligament and skin can improve the results of a mid-cheek groove. For many patients, using very small microdroplets of filler along the line of the ligament (less than 0.1ml total) can also be used in the superficial planes to further enhance any subcision performed.
Enhance your knowledge
Mastering anatomical knowledge of these ligaments and the broader infraorbital region - including fat pads, bone, and skin - is of paramount importance for anyone looking to become an expert under-eye injector. With this knowledge, practitioners can expect to create far more robust and effective treatment plans, provide better results while reducing post-treatment complications, and vastly expand their patient pool. The correct equipment is important too. My current polynucleotide (PDRN) of choice is Plenhyage, which is a high-quality PDRN and therefore provides maximum efficacy for treatment in the tear trough region. It can also effectively be combined with other treatments of the tear trough including, HA fillers, laser, and surgery.
Having said all that, I offer this word of advice: while the anatomy is often similar, each patient’s needs are different. Do not compromise spending time understanding the patient’s needs and collaborating with the patient to form a treatment plan as no two faces are the same.
References
1. Wong CH, Hsieh MK, Mendelson B. The tear trough ligament: anatomical basis for the tear trough deformity. Plast Reconstr Surg 2012;129(6):1392-402.
2. Stutman RL, Codner MA. Tear trough deformity: review of anatomy and treatment options. Aesthet Surg J 2012;32(4):426-40.
3. Haddock NT, Saadeh PB, Boutros S, Thorne CH. The tear trough and lid/cheek junction: anatomy and implications for surgical correction. Plast Reconstr Surg 2009;123(4):1332-40.
4. Doubt G, Garb BB, Rampazzo A, et al. Surgical anatomy relevant to the transpalpebral subperiosteal elevation of the midface. Aesthet Surg J 2015;35(4):353-8.
5. Mendelson BC, Jacobson ST. Surgical anatomy of the midcheek: facial layers, spaces, and the midcheek segments. Clin Plast Surg 2008;35(3):395-404.
6. Huang YL, Chang SL, Ma L, et al. Clinical analysis and classification of the dark eye circle. Int J Dermatol 2014;53(2):164-70.
7. Kpodzo DS, Nahai F, McCord CD. Malar mounds and festoons: review of current management. Aesthet Surg J 2014;34(2):235-48.
Declaration of competing interest: None declared.
COMMENTS ARE WELCOME














