The authors share their thoughts on how to achieve the best blepharoplasty results based on their 35 years of experience.
Are you a surgeon wishing to offer the best upper lid surgery to your discerning patients? To help chart the course towards the perfect blepharoplasty it may help to consider the following points. Taken together they should help you to stay clear of at least some of the most obvious dangers.
Know the patient’s expectations and variations of normal
No consultation will go wrong faster than the one where a patient is concerned about their lips or the shape of their nose only for the doctor to point out a problem with their eyelids. “But I like my eyes, they are the best thing about me” is a sure sign that trust and rapport have been irretrievably damaged. An experienced clinician will help a patient with the concern they have, and only after successful resolution will they bring up any extra treatment. Such problems can even occur with eyelids themselves – some adore Asian eyelids, some don’t and want a ‘western’ crease; some want a sleepy or ‘done’ look, others want to look natural. Some patients are bothered by restricted vision from upper lid hooding rather than the cosmetic effect; then there are skin tags and small moles – it is very tempting to remove them for some of us – but unless it has been discussed in the consultation, leave well alone. Beauty is very much in the eye of the beholder.
Diagnose the face as a whole and think ‘less is more’
When a patient is concerned about their droopy upper or lower lids it is important to view the eyes as part of the whole face – surgery to correct one aspect may prevent treatment of others. For example, upper lid hooded skin may be due to descending brows. This can potentially be corrected – at least for a while – with botulinum toxin and therefore avoid surgery, or it may require a combination procedure also treating the brows. Excessive skin removal may fix the brows in a low state and make it impossible to raise them surgically later without pulling on the upper lids to create a staring look. Similarly, lower lid surgery may be avoided for a time with a well-placed filler. Contrary to the name, modern fillers don’t fill but lift, so we sometimes refer to them in our clinic as lifters. A good way of avoiding causing harm is to think “what would I have done?” or “what would I do for my next of kin?”
Understand lid physiology
In order to perform a perfect blepharoplasty, one also needs to understand how lids work. Most obviously, lids close and protect the eye surface. Removing too much skin would prevent this and cause potentially irreversible sight loss from drying and scarring. Lids also lubricate, and so any surgery that affects the innervation of the lid or its movement can hamper the pumping action that moves water across the surface of the eye to the drainage apparatus in the nose. Most body movements are controlled on the left and right by separate halves of the brain; however, opening of the eyelids is an exception, there is only a single brain structure and therefore any surgery on one lid can affect the other side too. And to complicate matters further, eyelid opening is controlled both by a voluntary muscle system and an involuntary one. Surgery that damages either can result in droopier rather than less droopy lids. So, before you embark on surgery make sure you know whether you are dealing with a ptosis (a low sitting lid) or overhanging skin (dermatochalasis). If there is any doubt in your mind do not proceed.
Understand systemic implications of lid pathology
Eyelid problems can signal local or distant disease. Swollen or red eyes or lids can point to thyroid disease, autoimmune disease, allergies or even certain blood cancers. Yellow lesions can signal high cholesterol, or other abnormal cellular processes. Loose droopy lids can be associated with sleep apnoea, Parkinson’s-like or ocular pharyngeal dystrophy disease, metastatic cancer or a swollen blood vessel aneurysm, to mention but a few. The idea that lid surgery is nothing to worry about medically is far from the truth. If there has been any surgery to the eyeball this should also give patient and surgeon pause – some eye operations create very delicate blebs and surgery to the lid can cause these to fail, resulting in blindness. Dry eyes may make someone a poor candidate for lid surgery, or certain scarring disorders like oculo-cicatricial pemphigoid.
Be wary of previous non-surgical approaches that scar or distort
You should also be wary of some of the periocular energy devices sold as an alternative to upper lid surgery. Some treatments can cause the finely sandwiched layers of tissues in the lid to fuse together like a molten panini, making surgery far more destructive and difficult. In general, lid surgery should be done first, not after attempted scarring treatments.
Optimise your patient, not just your surgery
Surgical results are not just about the surgeon – the patient must be in their best possible pre-surgical state. For example, blood pressure and blood sugar should not be too high, any blood thinning medication should be stopped if possible and there should have been time for any treatments, like botulinum toxin, to wear off and for the skin to be optimised for healing. Optimising the patient like this will allow for shorter operations, less bleeding and therefore less inflammation and improved healing. Preoperative management also means that our patients, as a rule, can opt to have their surgery under local anaesthetic.
Customise your surgery
The perfect blepharoplasty will be the blepharoplasty that satisfies the patient and does not adversely affect the functions required of the eyelid. What this means is that there is no one perfect bleph – the trick is to tailor it to the individual and this in turn means figuring out what the patient wants. We have already mentioned a ‘done’ look, or a ‘subtle’ look but there are many other possibilities depending on where the skin crease is placed and the amount of tarsal plate show (Figure 1).
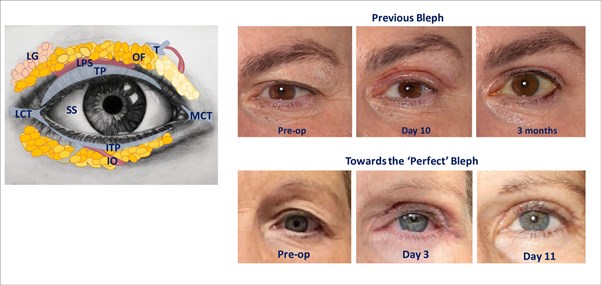
Figure 1: The periocular anatomy is complex even within the orbital rim and behind the septum. Shown are lacrimal gland (LG) levator palpebrae superioris (LPS), orbital fat (OF) of different colours, tarsal plate (TP) and inferior tarsal plate (ITP), medial and lateral canthal tendons (MCT & LCT), trochlear pulley (T) and inferior oblique (IO) and numerous fibrous septae.
The clinical images show the results of a standard FaceRestoration bleph from around 12 months ago (top) and the remarkable improvements possible as we challenge ourselves to perform a perfect blepharplasty (bottom). The lower images show that results at day 11 can now equal the three month follow-up of our prior approach, and swelling at day three can be even less than at day 10 previously.
What the perfect bleph should not do is to remove excessive fat or prolapsed glands. Behind the upper lid and above the eye there are three compartments. The medial and central fat can be adjusted as required, but the lateral contains the tear gland. As we age it can fall forwards and be excised by the unwary, creating a dry eye problem that is permanent and difficult to treat.
Another area requiring care is the lateral canthus where a fibrous band attaches the outer corner of the eye to the bone. Any damage to this area can cause rounding of the eye corner, or a slanting eye. The septum, the thin sheet that keeps the orbital fat separate from the lids, can weaken over time or be damaged, allowing fat to bulge forward. Often strengthening or repairing the septum is better than removing fat – we lose fat in the face with age and removal can create an unhealthy skeletal look as we age. But tightening the septum too much can prevent the lids from closing.
Optimise your postoperative care and expect changes – keep calm
At first not every patient will have a perfect blepharoplasty result, or at least not straight away. But they can still be perfectly reassured and managed. Often the immediate postoperative period can be unusual as the brain learns to adjust to a change in the tissues it controls. Someone who has spent decades continuously lifting their brow will not stop doing that immediately after surgery. And one side may relax before the other. We have seen eyebrows go through the full gamut of positions before settling down. The key to a perfect blepharoplasty is to keep calm and not attempt any corrections or changes early on. Good surgeons need to be patient with their patients – most things will settle, the exception being when not doing something risks further injury such as an inability to close the eyes.
Be confident of non-surgical adjuncts including new developments
The perfect blepharoplasty surgeon will move with the times and be willing to adapt and profit from developments in technology, whether it be laser-assisted surgery, new medications, new injectable products, the best skin products and the leading energy-based devices. We very rarely achieve all we can with a single modality.
Work as a team
A confident and talented surgeon will be happy to work with others. As oculoplastic surgeons we work with plastic surgeons, dermatologists, endocrinologists, aesthetic practitioners, laser specialists, business managers, marketing and PR experts, nurses, optometrists, accountants, receptionists and other oculoplastic surgeons around the world. Teamwork provides opportunities to learn and gain experience safely and builds opportunities for cross-referral.
Tackle difficult cases and revisions
Practice makes perfect, and if one isn’t willing to tackle the challenging or complex cases one will not become an expert at the mundane. For many surgeons it is having dealt with complex complications requiring advanced tissue flaps, handling enormous ocular tumours in Africa, dealing with blinding inflammation in the UK, spending thousands of hours assisting at surgery, or performing revisions, that allows for peak performance during an upper lid blepharoplasty.
Be honest with yourself and stay humble
The perfect blepharoplasty surgeon does not think that they are the perfect blepharoplasty surgeon. For as soon as they think that, they stop learning or reviewing their outcomes critically. This is why we perform standardised Vectra imaging on all our patients before and after surgery. They are there, in colour or black and white, to be compared by computer overlay. This is helpful for patients who may study their faces more and notice asymmetries which were there prior to surgery but not previously noticed. Though we learn from our patients’ experience so we can make things ever better for them this does not mean agreeing to any intervention they suggest. We have had patients request eye removal, or caruncle and plica excision (the fleshy bits in the inner corner that are a vestige of our evolutionary third eyelid). The patient is an expert on their experience, but not on what can be safely achieved. Though most patients are sensible some need strong guidance to know when to stop seeking further interventions.
Finally, is there a perfect blepharoplasty?
Though it seems a bit unfair to reveal to the reader at the end of such a long article, there is of course no such thing as a perfect blepharoplasty. Blepharoplasty surgery is a constant journey of improvement, learning from the previous generation of surgeons’ experience and continuing to strive to perfect it. The most any of us can hope to achieve today is the most perfect blepharoplasty possible right now.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME











