The authors provide an expert guide to the use of hyaluronic acid dermal fillers to rejuvenate the periorbital area.
One of the early signs of periorbital ageing are dark circles around the eye, with patients complaining of a fatigued appearance. In 1961, Loeb described the ‘nasojugal groove’; the medial concavity between the eyelid border and cheek. He hypothesised the defect was due to volume loss of the medial and central fat pad, in addition to fixation of the orbital septum at the level of the inferomedial portion of arcus marginalis [1].
In 1969, Flowers came up with the now commonly used term of ‘tear trough’. He identified several other factors which led to its development, including the muscular defect between the orbicularis muscle and angular head of the quadrates labii superioris muscle, cheek descent and loss of facial volume.
Modern day views are that the tear trough is a concave deformity caudal to the orbital fat that results from ageing and inherited anatomical difference [1,2]. The end result and tired appearance has a significant effect on an individual, including lower self-esteem and worse perception of facial appearance.
It presents as a 2cm depression, inferior to the orbital fat of the lower eyelid which can potentially pseudo herniate, casting shadows over the area in question [1-5]. Improvement and rejuvenation can be achieved using fat grafting to supplement volume, fat repositioning via an arcus marginalis release or the use of hyaluronic acid dermal fillers. The endpoint, an aesthetically pleasing tear trough, should show a smooth transition between the preseptal and orbital portions of the orbicularis oculi muscle, with continuation into the upper malar region without a definable transition point.
Anatomy of the tear trough and ageing
It is important to first understand the local anatomy, using it to guide strategies for management, as well as acting as a good differentiator between potential treatment options.
Jiang et al. performed a five-year retrospective clinical study between May 2009 and Sept 2014 [6]. In their paper they included 78 patients (69 women and nine men) with tear trough deformity ranging from 25 to 69-years-old.
Ageing and tear trough anatomy was categorised into three criterial deficits:
- Volume loss
- Orbital fat pad herniation
- Excess lower eyelid skin.
Class 1 (n=10) patients did not have bulging orbital fat or excess skin, mild periorbital volume loss and flatness of the midface. Class 2 (n=18) patients had mild orbital fat bulging without excess skin. Class 3 (n=50) patients had significant volume loss, severe fat bulging and excess skin. All patients had full depression circumferentially along the orbital rim.
Patients who wanted a reversible treatment received hyaluronic acid injections using a 27-gauge needle at 90 degrees. The needle was passed through skin, dermis and orbicularis muscle until the tip reached bone and the filler was injected in retrograde fashion; 0.2ml to 0.5ml was used per side to form a scaffolding, with the aim of filling the orbital hollowness [7,8]. Those with Class 3 deficits were treated with fat repositioning using an arcus marginalis release (release of the orbicularis oculi muscle origin).

Follow-up data on 67 of the 78 patients were collected at three months and five years. All patients reported good results, rating themselves as very satisfied or satisfied.
Anatomical dissections, by Haddock et al., of the lower eyelid and midfacial regions showed two specific tissue layers: the superficial and deep plane, together contributing to the lid-cheek junction and the tear trough [9]. The superficial plane includes the pretarsal and orbital portions of the orbicularis oculi muscle, as well as the underlying fat. In the deep plane they found separation between the lid cheek junction and the tear trough.
Medially, the orbital orbicularis is attached at its origin to the maxilla, while there are also ligamentous attachments laterally. Fibrous structures extend from the periosteum along the inferior orbital rim and eventually become lamellar. These structures pass through orbicularis oculi into skin as the ‘obicularis retaining ligament’, named secondary to its underlying attachment to zygoma, and caudally to the arcus marginalis at the orbital rim.
The formation of the tear trough deformity is multifactorial. Anatomical variations include: volume loss, skin laxity and in certain patients where the position of the tear trough is within the boundary of the orbicularis muscle [10]. Improved anatomical knowledge ultimately leads to improved treatment options [11].
The lambros is the junction of the thick cheek skin and thin lower eyelid skin. With age, the lower eyelid skin losses elasticity and thickness, in addition to potentially gaining a degree of hyperpigmentation. Simultaneous loss of mid facial volume reduces the support at the nasojugal groove, exacerbating prominent tear troughs further. There is also laxity of the supporting ligaments, like the orbicularis retaining ligament, due to gravitational descent of the mid face [12-14]. Other underlying mid face structures also play an important role in the process, such as with maxillary hypoplasia [15].


Assessment and treatment
Assessment of tear trough variations is a subjective entity for both the surgeons and patients typically. There have been attempts at creating an objective assessment, such as Hirmand in 2010 who created a classification system based on clinical evaluation [16]:
- Class I patients have volume loss limited medially to the tear trough. These patients can also have mild flattening extending to the central cheek.
- Class II patients exhibit volume loss in the lateral orbital area in addition to the medial orbit, and they may have moderate volume deficiency in the medial cheek and flattening of the central upper cheek.
- Class III patients present with a full depression circumferentially along the orbital rim, medial to lateral.
An appropriate anatomical understanding and an appreciation of the ageing process allows the treatment to be customised as required. An example would be the necessity for volume enhancement of the infraorbital rim or cheek in older patients to improve overall outcomes.
Unlike other volume deficits in the face, tear trough filler is more technically demanding due to the complex anatomy and interaction with numerous facial structures.
Hyaluronic acid (HA) fillers are the most commonly used worldwide [17]. They are seen as a safe, non-invasive and reversible treatment which has gained increasing popularity recently. HA fillers can be used as a sole treatment option or as an adjunct to surgery. Their primary disadvantage is that they are not permanent, however longer lasting fillers are overcoming this hurdle.
Patient selection is paramount. When assessing the patient, consideration should be taken with regards to skin quality and depth of hollowness. The ideal candidate has good skin tone, minimal laxity and mild to moderate tear trough depth. Care should be taken in patients with large fat pads or pseudo bulging pads as improvements are minimal, with some patients complaining of post-treatment ‘puffyness’.
Care should also be taken with patients who have excess skin in the lower eyelid and skin laxity. The discolouration of the lower eyelid skin can contribute to the appearance of tear trough. This can be improved in some cases with HA fillers, but the results are not guaranteed, with inadequate information often given to patients. Those with excess skin laxity and fat herniation would find greater benefits with surgery rather than injectables.
Injecting technique varies between surgeons. Topical local anaesthetic creams can be used to reduce the pain of injection. Direct injection into the area with a 30-gauge needle deep to the dermis was previously very common, with gentle finger pressure massage of the filler. Care must be taken with massaging so as to not displace the filler into the cheek, which will in fact accentuate the defect rather than resolve it. There is a greater risk of bruising with direct injections and this may take a few days to settle. Post-injection care involves sleeping with an extra pillow to keep the head elevated for a few days and avoidance of massage to the area.
The Kane technique involves injecting into the deepest portion of the medial tear trough first, between the skin and orbicularis oculi. Threads of filler are injected cephalad and caudal to the tear trough. The raised filler is then tapered medially. If the tear trough is deep, a cross hatch injection technique is used to add volume. This involves a lot of injections and is very much dependant on the quality of the patient’s skin. Kane’s post-procedure recommends head elevation, in addition to night-time ice packs for two nights.

Preferred technique
The skin in the lower eye lid is often very delicate. As a result, we prefer avoiding direct injection if possible. Patients are given an ice pack for several minutes pre-procedure, with the aim of reducing swelling and bruising. The lid cheek junction is marked with white eyeliner with the patient sitting upright and maintaining an upward gaze (accentuating the defect medially). An upward, outward gaze outlines the deficit laterally on the contralateral side. Topical local anaesthetic cream is used on the zygoma before 0.3ml lidocaine is injected. An infraorbital block can be used, but we prefer to avoid this as it can distort the anatomy.
A needle (23-25G depending on skin thickness) is used to create a small tunnel before introduction of the cannula (25G 50mm). Using this technique, we have found the treatment to be less traumatic and a noticeable reduction in bruising.
The cannula is passed to the deepest point medially. HA is injected deep to the dermis and muscle at multiple levels as the cannula is gently withdrawn in a retrograde fashion. Discontinuous lines of filler are used to provide a more graded appearance and avoid a noticeable sausage appearance. We avoid injecting large volumes, with the aim of allowing a more graded appearance from medial to lateral. Overcorrection is not recommended. Gentle massage is done to spread the filler and avoid irregularities.
Afterwards, patients have an ice pack for 10 minutes in clinic and are advised to avoid alcohol for 48 hours, as well as sleeping with an extra pillow at night for a few nights.
Complications
Several complications must be discussed pre-treatment to ensure appropriate consent is obtained. Ecchymosis is discolouration of the skin secondary to bleeding beneath. This is reduced with a cannula technique, but also with ice packs [18]. Pain and erythema are often self-limiting, but with a single insertion point the degree of these is significantly reduced. Irregularities can occur, which can be massaged at the time of injection or a few weeks later at follow-up. If they do not resolve, they can be dissolved with 10 units of hyaluronidase in the specific area. Subtle oedema may occur due to the hydrophilic nature of the filler and often resolves in two to three weeks. Finally, pre and post-procedure photos need to be taken as some patients after a few weeks perceive a lack of change as they get used to their new appearance.
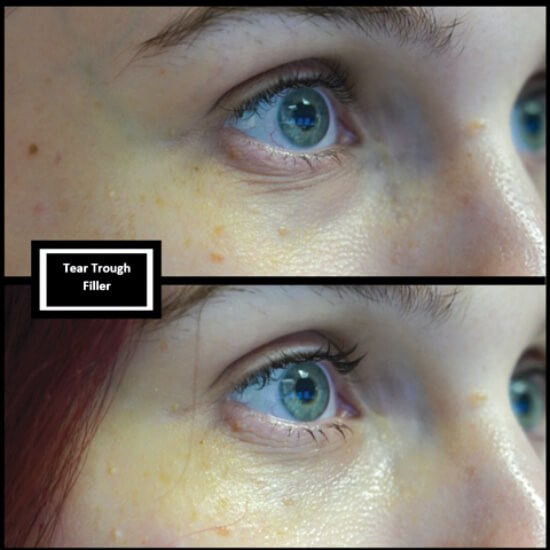
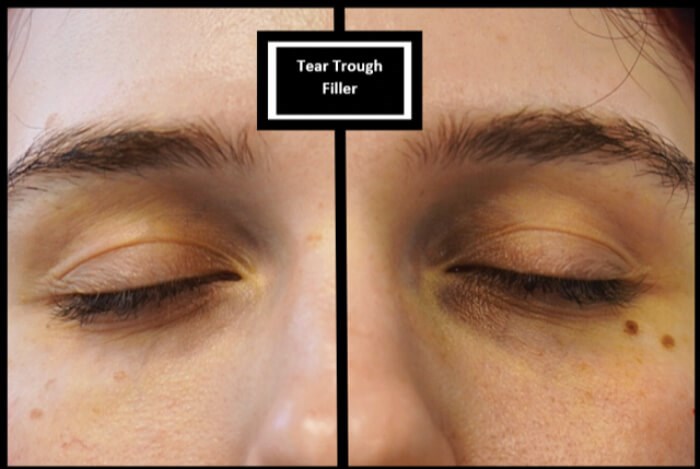
Results
Duration of results varies depending on the HA filler and brand, but often can last longer in this area due to the lack of soft tissue movement, when compared to the rest of the face [19]. The key to good results is patient selection and appropriate pre-injection consultation, with studies typically highlighting an 85-88% aesthetic improvement [20].
Conclusion
Periorbital rejuvenation can have a dramatic impact on patients’ lives. Patient selection is the key to achieving optimal results. Understanding the local anatomy and the dynamic ageing process allows the correct choice of treatment, as well as the placement of filler.
References
1. Loeb R. Fat pad sliding and fat grafting for leveling lid depressions. Clin Plast Surg 1981;8:757-76.
2. Flowers RS. Tear trough implants for correction of tear trough deformity. Clin Plast Surg 1993;20(2):403-15.
3. Espinoza GM, Holds JB. Evaluation and treatment of the tear trough deformity in lower blepharoplasty. Semin Plast Surg 2007;21:57-64.
4. Hirsch RJ, Carruthers JD, Carruthers A. Infraorbital hollow treatment by dermal fillers. Dermatol Surg 2007;33:1116-9.
5. Hirmand H. Anatomy and nonsurgical correction of the tear trough deformity. Plast Reconstr Surg 2010;125:699‑708.
6. Jiang J, Wang X, Chen R, et al. Tear through deformity: different types of anatomy and treatment options. Post Dermatol Alegrol 2016;33(4):303-8.
7. De Pasquale A, Russa G, Pulvirenti M, Di Rosa L. Hyaluronic acid filler injections for tear-trough deformity: injection technique and high-frequency ultrasound follow-up evaluation. Aesthetic Plast Surg 2013;37:587-91.
8. Berros P, Lax L, Bétis F. Hyalurostructure treatment: superior clinical outcome through a new protocol – a 4-year comparative study of two methods for tear trough treatment. Plast Reconstr Surg 2013;132:924e-31e.
9. Haddock NT, Saadeh PB, Boutros S, Thorne CH. The tear trough and lid/cheek junction: anatomy and implications for surgical correction. Plast Reconstr Surg 2009;123(4):1332-40.
10. Codner MA, Wolfli JN, Anzarut A. Primary transcutaneous lower blepharoplasty with routine lateral canthal support: a comprehensive 10-year review. Plast Reconstr Surg 2008;121:241-50.
11. Muzaffar AR, Mendelson BC, Adams WP. Surgical anatomy of the ligamentous attachments of the lower lid and lateral canthus. Plast Reconstr Surg 2002;110:873‑84.
12. La Ferriere KA, Kilpatrick JK. Transblepharoplasty: subperiosteal approach to rejuvenation of the ageing midface. Facial Plast Surg 2003;19:157-70.
13. Shorr N, Hoenig JA, Goldberg RA, et al. Fat preservation to rejuvenate the lower eyelid. Arch Facial Plast Surg 1999;1:38-9.
14. Yang N, Qiu W, Wang Z, et al. Anatomical studying of the tear trough area. Zhonghua Zheng Xing Wai Ke Za Zhi 2014;30:50-3.
15. Goldberg RA, McCann JD, Fiaschetti D, Ben Simon GJ. What causes eyelid bags? Analysis of 114 consecutive patients. Plast Reconstr Surg 2005;115:1395-402.
16. Hirmand H. Anatomy and nonsurgical correction of the tear trough deformity. Plast Reconstr Surg 2010;125(2):699-708.
17. Peckinpaugh JL, Reddy HS, Tower RN. Large particle hyaluronic acid gel for the treatment of lower eyelid retraction associated with radiation-induced lipoatrophy. Ophthal Plast Reconstr Surg 2010;26:377-9.
18. Nestor MS, Ablon GR, Stillman MA. The use of a contact cooling device to reduce pain and ecchymosis associated with dermal filler injections. J Clin Aesthet Dermatol 2010;3(3):29-34.
19. Donath AS, Glasgold RA, Meier J, Glasgold MJ. Quantitative evaluation of volume augmentation in the tear trough with a hyaluronic acid-based filler: a three dimensional analysis. Plast Reconstr Surg 2010;125(5):1515-22.
20. Viana GAP, Osaki MH, Cariello AJ, et al. Treatment of the tear trough deformity with hyaluronic acid. Aesthet Surg J 2011;31(2):225-31.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME











