This article has been verified for CPD. Click the button below to answer a few
short questions and download a form to be included in your CPD folder.
Rejuvenation of the eyes has a very high impact on the overall appearance of the face. The shadow pattern of the inferior orbital rim is one of the most important shadows of the ageing midface [1]. Although every patient has individual needs, blending of the lid-cheek junction is of particular importance to achieve a youthful appearance.
Ageing process of the face
Facial ageing is a multifactorial process. Physiological and morphological changes occur in bones, ligaments, muscles, fascia, fat and skin [2,3].
Facial soft tissues tend to descend with age. Repositioning the soft tissues toward their original position is a common goal which one tries to achieve when performing certain procedures, ranging from surgical facelifts to thread lifts and the use of soft tissue injection techniques [4].
The infraorbital region
The anatomy of the lower eyelid and the lid-cheek junction has to be understood as a unit. This is because the structures are continuous from the eyelid to the cheek, and they influence each other during ageing. The lower eyelid and tear trough deformities can occur depending on the underlying structures. These vary from lower eyelid hollowness, dark circles, tear trough depression with or without fat herniation, and skin excess [5].
Patients usually present with dark circles in the medial infraorbital area, more commonly known as the tear troughs. However, this is not the only problematic area. A great challenge is faced when dealing with the lateral infraorbital area, particularly the lateral depressions between the lower eyelid and the cheek eminence, which is called the lid-cheek junction. These are also known as the palpebromalar grooves [6].
Surface anatomy
The skin of the face has consistent attachment points to the underlying structures through the facial retaining ligaments. As the volume of the face deflates, these attachment points will define most of the shadows that develop with age [7].
This was shown by Yang et al. [8], who reported that the orbicularis retaining ligament (ORL) and the malar fat pad play important roles in the formation of the tear trough deformity and palpebromalar groove. The groove in the lateral portion of the lid-cheek junction is formed mainly due to the ORL, which arises from the inferior orbital rim and ends at the junction of the palpebral and orbital portions of the orbicularis oculi muscle. The histology and structure of the ORL changes in the mid-pupillary line when it continues into the tear trough. Yang et al. also showed that the sub-orbicularis oculi fat pad (SOOF) was located mainly at the inferior lateral orbit underneath the orbicularis oculi muscle, while there was no obvious oculi fat pad in sagittal sections of the tear trough. Therefore, the orbicularis retaining ligament limits the age-induced descent of the orbicularis oculi muscle, and the subcutaneous tissue volume reduction caused by malar fat pad atrophy and descent enhances the tear trough deformity.
The nomenclature
Different authors refer to the surface markings of this area with different nomenclature. The author recommends the following as the most straightforward nomenclature to be used when making reference to the relevant anatomical regions of the face.The depression in the medial infraorbital area is called the tear trough.
The depression immediately inferior to the tear trough is called the nasojugal groove. The nasojugal groove extends inferolaterally from the medial canthus to a point inferior to the medial limbus. It becomes progressively more prominent with ageing.
The nasojugal groove is continuous with the mid-cheek groove, which can also be referred to as a mediojugal fold or malar groove [2,6].
The palpebromalar groove is the lateral depression between the lower eyelid and the cheek eminence, and is also referred to as the lid-cheek groove or lid-cheek junction.
The nasojugal groove (the tear trough) and the palpebromalar groove (lid-cheek groove) form a ‘V’ shaped deformity with increasing age. These two grooves connect to become a continuous groove that sharply demarcates the bulging orbital fat above, from the retruded midcheek below. The resulting demarcation of these grooves is determined by the attachment of the underlying ligaments.
The layers in the infraorbital region of the face
The infraorbital region can be divided into lateral and medial parts. The boundary between the lateral and medial parts lies about 4-6mm medial to the midpupillary line [2,5,9-11].
In the lateral part, seven different layers can be identified, while in the medial part, only three layers can be identified.
Layer one is the skin, layer two is the orbicularis oculi muscle, and layer three, is the periosteum [2]. The skin in the infraorbital region is described as being the thinnest in the human body. In the medial part, the orbicularis oculi muscle can sometimes be seen through the thin skin, and gives a blueish appearance to the tear trough area.
In the lateral infraorbital area, there’s a layer of superficial fat above the muscle. This is part of the malar mound. This is practically absent in the medial area. The skin over the malar fat pad is thicker than over the lower eyelid and this further accentuates the lid-cheek junction.
Layer three of the lateral part is the orbicularis oculi muscle. This muscle is attached to the anterior portion of the orbital aperture by fascia on its undersurface, which intermingle with the periosteum of this area. This is called the ORL. The ORL is very important to consider when treating this area. It loops around the anterior aspect of the orbit and it connects the muscle to the orbit. It inserts 2-3mm below the orbital rim. The subdivision of the orbicularis oculi muscle into its palpebral and orbital parts corresponds to the course of the ORL. Laterally it forms the lateral orbital thickening [2,5,10-12].
The ORL is the boundary between the extraorbital fat such as SOOF and the intraorbital fat. This means it forms the deep boundary which separates the cheek from the lower eyelid and intraorbital fat. In the tear trough area, the ORL changes its name to become the tear trough ligament.
Layer four is the sub-orbicularis oculi fat, known as SOOF. This is located underneath the orbicularis oculi muscle and is divided into the medial and lateral portions. The SOOF is one of the deep fat compartments of the face. It is bound superiorly by the orbicularis retaining ligament and inferiorly by the zygomatico-cutaneous ligament (ZCL). It corresponds to the malar mound above, which is the superficial infraorbital fat. This is the reason why it is important to inject into the deep layer, as injection into the superficial layer leads to prolonged oedema [3,9].
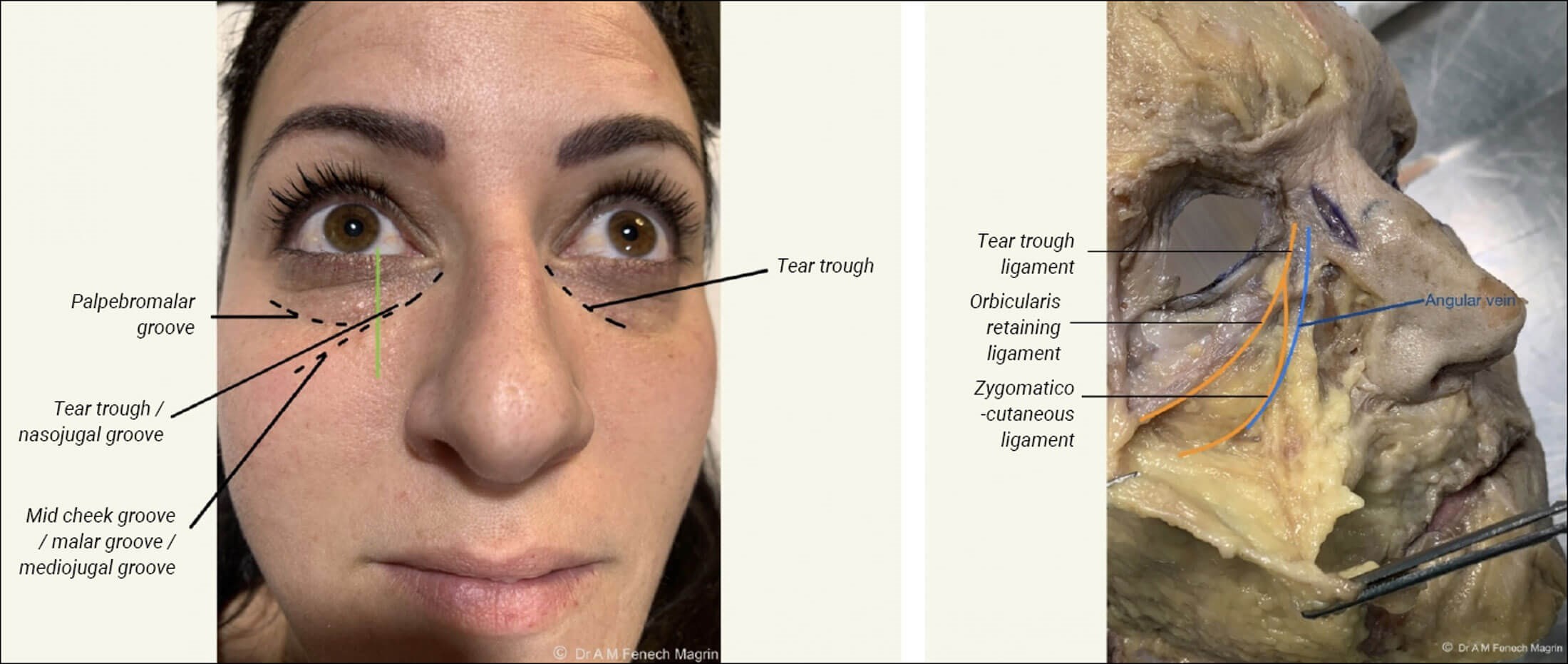
Figure 1: Nomenclature of surface anatomy, folds and grooves shown on model
with corresponding ligaments shown on a cadaveric dissection.
The point where the ZCL and ORL fuse medially can be seen as a vertical landmark on the surface approximately 2-4mm medial to the mid-pupillary line, which corresponds to the medial limbus (Figure 1). When the zygomatico-cutaneous ligament connects with the ORL, it encloses the space where the SOOF is located. Therefore, the medial limbus is the most medial extent of the SOOF, and is the point where the tear trough begins. The orbicularis retaining ligament changes its name once it fuses with the zygomatico-cutaneous ligament. This is now known as the tear trough ligament [2,10].
Layer five is the fascia, which is the continuation of the superficial lamina of the deep temporal fascia. Layer six is the fat in the pre-zygomatic space. Many authors don’t make a distinction between the pre-zygomatic space and the SOOF.
Layer seven is the periosteum. The inferior orbital rim changes in shape, position and also projection during the ageing process. It becomes lower, especially in the lateral portion. A decrease in the projection can also be observed in CT scan images, which were utilised in the studies carried out by Khan and Shaw [13]. This causes a loss of bony support to the already atrophic tissues.
Injection technique / algorithm
Patient examination is very important. The type of the lower eyelid and tear trough deformity needs to be established. The presence of palpebral fat pads or inferior eyelid oedema can be an absolute or relative contraindication to the treatment. When there is the presence of relatively moderate oedema, it is recommended to inject half the indicated volume, or even less [4,6,9].
The infraorbital area can be treated in different ways. The following is a description of an injection technique used by the author.
First, the tear trough should only be treated if and when indicated. A 25G, 50mm blunt-tipped cannula is used. The same entry point is used for both the tear trough deformity correction and for the rest of the infraorbital area, as the whole infraorbital area is treated as a unit. Therefore, the entry point is through an inferior approach, on an imaginary vertical line dropped down from the lateral limbus, around 1.5 to 2cm below the lid-cheek crease. This is done so the cannula slides lateral to the major vessels. The entry point is performed using a 23G needle.
The cannula is advanced cranially towards the medial infra-orbital tear trough region. One will encounter some resistance as the orbicularis oculi is reached and some gentle tugging is usually needed to go deep to the muscle. The cannula has to glide easily, once the deep plane is reached. If one comes across obstacles, the cannula should not be advanced further; it needs to be retracted for a few millimetres. The depth and the angle of entry has to be slightly changed until the penetration is easier. When the cannula reaches the tear trough depression, this can be felt and controlled with the non-dominant hand. Generally, no more than 0.2-0.3ml of hyaluronic acid (HA) are injected, in four to six passages on each side, using a slow, retrograde, fanning technique [4,11]. It’s always preferable to under correct, as we know this area, being devoid of fat is unforgiving, and overcorrection can lead to lumpiness and unsatisfactory results. From this same entry point, the middle and lateral portion of the lid-cheek groove can also be treated.
One of the aims is to readjust the alignment of the ORL. With ageing, this ligament changes orientation from 90 degrees between the maxilla and the ORL, to 45 degrees. Therefore, by injecting a filler below the ligament, it repositions it to its original angle, and also repositions the mid-face, improving the appearance of the lid-cheek junction. Recontouring of the inferior orbital rim is also an integral part of this treatment protocol.
As one glides superiorly with the cannula to treat the middle part of the infraorbital area, a resistance or a pop is felt, and this would be the ZCL. One should stop before feeling the second pop or when further resistance is felt, as there’s a risk of going into the orbit. Therefore, with the finger of the non-dominant hand, the inferior orbital rim should be secured, to prevent the cannula from passing cranial to the ORL or into the retro-septal space. The same is repeated in the lateral infraorbital regions, while about five to six passes are done from caudal to cranial. In the lateral region, the lateral SOOF is reached in layer four.
Once the cannula is palpable at the inferior orbital rim, the product is administered in small boluses and retrograde threading technique, of 0.02-0.2ml at a time. One should always keep in mind that the superior anatomical boundary for the cannula is the ORL. Perforation of this and injection of the intraorbital fat leads to worsening of the eyelid bags.
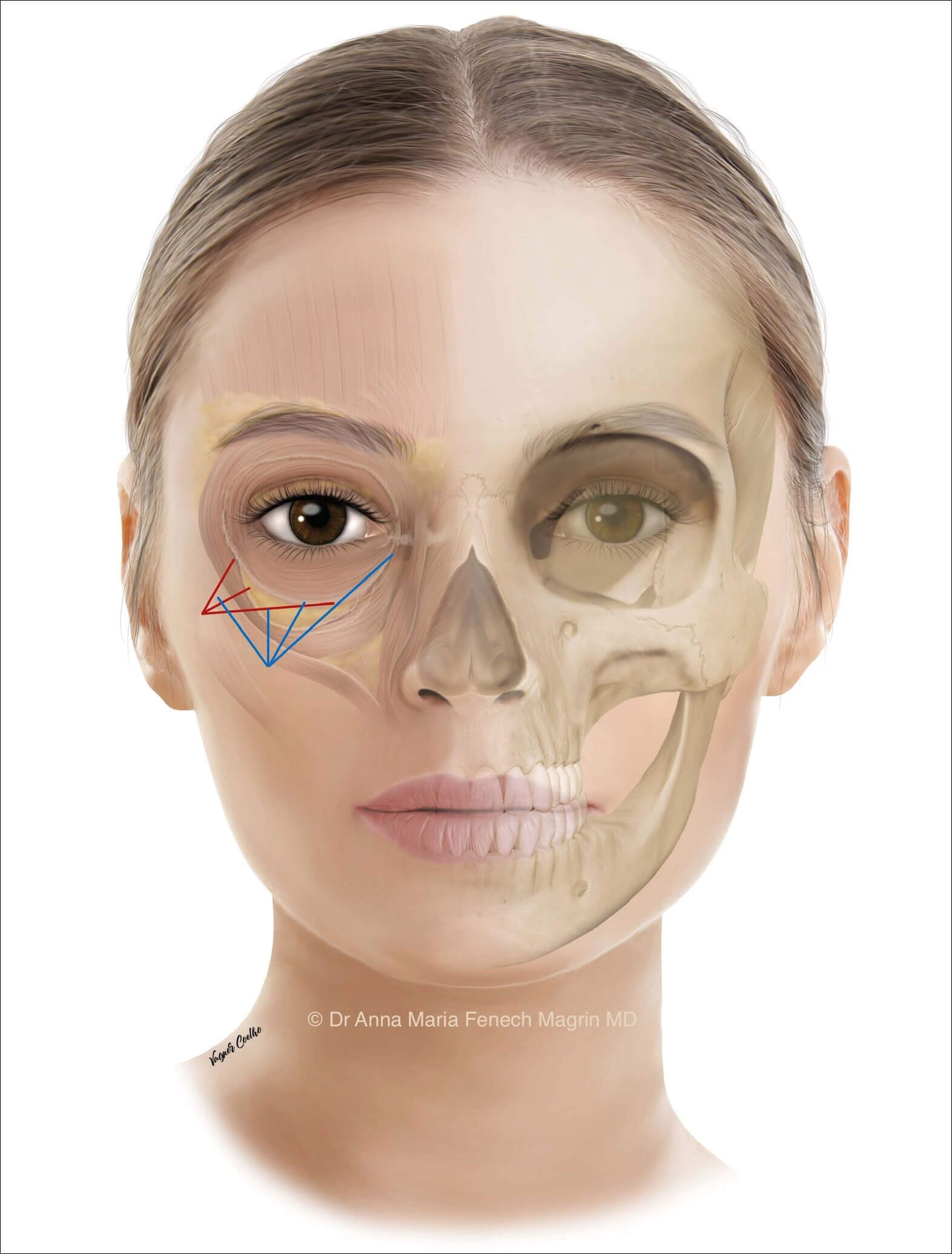
Figure 1: Nomenclature of surface anatomy, folds and grooves shown on model
with corresponding ligaments shown on a cadaveric dissection.
After volumisation of the deep fat compartment, the SOOF, the second step is the contouring phase. Recontouring of the inferior orbital rim is performed. Another dermal access can be done for this. This would be located 1-1.5cm lateral and 1.5cm caudal to the lateral canthal ligament (Figure 2). A 25G 50mm blunt-tipped cannula is used. The cannula is advanced from lateral to medial, gliding deep to the orbicularis oculi muscle within the supraperiosteal plane.
From here, the tear trough can also be reached. A resistance can be felt when the ZCL is reached. One must push gently through it to reach the tear trough area. The target layer for both injection steps should be the deep to the orbicularis oculi muscle and inferior to the ORL.
Another technique that can be used is the bolus injection technique using a needle. The bolus injections can be performed with the syringe supplied by the filler material manufacturer.
The needle is inserted perpendicular to the skin until it reaches the bone. The entry points are marked 2-3mm below the lid-cheek junction, which corresponds to the wider and deeper part of the crease. The position of the superficial vessels should be noted to try and avoid haematomas. The HA is deposited in bolus injections of 0.1-0.15ml in contact with the periosteum, until reaching the level of the medial limbus. Again, it is always important to inject in a deep plane, underneath the orbicularis oculi muscle.
Conclusion
In summary, entering the layer which is deep to the orbicularis oculi muscle is of key importance when depositing the filler agent in the lid-cheek junction. Knowledge of the anatomy is very important when treating the infraorbital area. It is always better to undertreat then to overtreat as too much filler may lead to unfavourable results.
References
1. Glasgold M, Glasgold R, Lam S. Autologous fat grafting for midface rejuvenation. Clinics in Plastic Surgery 2015;42(1):115-21.
2. Cotofana S, Fratila AA, Schenck TL, et al. The anatomy of the aging face: a review. Facial Plastic Surgery 2016;32(03):253-60.
3. Cotofana S, Lachman N. Anatomy of the facial fat compartments and their relevance in aesthetic surgery. JDDG: Journal der Deutschen Dermatologischen Gesellschaft 2019;17(4):399-413.
4. Bernardini FP, Casabona G, Alfertshofer MG, et al. Soft tissue filler augmentation of the orbicularis retaining ligament to improve the lid‐cheek junction. Journal of Cosmetic Dermatology 2021;20(11):3446-53.
5. Mojallal A, Cotofana S. Anatomy of lower eyelid and eyelid–cheek junction. Annales de Chirurgie Plastique Esthétique 2017;62(5):365-74.
6. Lee JH, Hong G. Definitions of groove and hollowness of the infraorbital region and clinical treatment using soft-tissue filler. Archives of Plastic Surgery 2018;45(03):214-21.
7. Glasgold M. Introduction to volumetric facial rejuvenation. Facial Plastic Surgery 2015;31(01):10-4.
8. Yang C, Zhang P, Xing X. Tear trough and palpebromalar groove in young versus elderly adults: a sectional anatomy study. Plastic and reconstructive surgery 2013;132(4):796-808.
9. Sykes JM, Cotofana S, Trevidic P, et al. Upper face: clinical anatomy and regional approaches with injectable fillers. Plastic and reconstructive surgery 2015;136(5):204S-18S.
10. Pessa JE, Rohrich RJ. Facial Topography. Clinical Anatomy of the Face. St. Louis, USA; Thieme Medical Publishers, Inc; 2012.
11. Ingallina FM. Facial Anatomy & Volumizing Injections. Superior & Middle Third. 3Aface Academy.
12. Rohrich RJ, Avashia YJ, Savetsky IL. Prediction of facial aging using the facial fat compartments. Plastic and Reconstructive Surgery 2021;147(1S-2):38S-42S.
13. Kahn DM, Shaw RB. Aging of the Bony Orbit: A Three-Dimensional Computed Tomographic Study. Aesthetic Surgery Journal 2008;28(3):258-64.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME











