With melanoma rates increasing globally, should there be screening of high-risk groups? Stephen Hayes takes a look at how Australia has reduced its melanoma mortality and asks whether a similar model should be adopted elsewhere.
In Britain, some 16,000 new cases of melanoma skin cancer are reported annually, with some 2300 fatalities. Melanoma is now the fifth most common cancer (excluding BCC and SCC) and the 16th commonest cause of cancer death (source Cancer Research UK). Rates are increasing faster than for any other cancer. Melanoma is one of the few cancers that affects economically better off people more, presumably due to sun exposure on foreign holidays.
There are three ways to reduce melanoma mortality: primary prevention, early detection and treatment of advanced disease. The first way is attractive, ‘prevention is better than cure’, but requires sustained behaviour change in the population over time, which is difficult to achieve. People love sunshine! Treatment of advanced disease has improved with the advent of immunotherapy agents such as ipilimumab and nivolumab, but they are more palliatives than cures, have major side-effects and are extremely expensive.
UK melanoma detection policy – wait until it’s obvious
Early detection is somewhat haphazard in the UK, basically ‘If you are worried about a mole, see your GP’. This policy relies on deadly skin cancers progressing to a stage where untrained persons (patients) notice them. Given the steady fall off in five-year survival as melanomas become thicker, is this a wise or evidence-based policy? British GPs’ skin lesion recognition skills are variable, and full skin checks are not available routinely. All this was brought into stark contrast for me on a two-month skin cancer sabbatical in Australia and New Zealand last December and January, when I sat in and learned from two Australian GP skin cancer experts, Cliff Rosendahl in Brisbane and Jeff Keir of Ballina, New South Wales. Australia has reduced melanoma mortality, mostly by earlier detection.
Most skin cancer screening in Australia is done by GPs
It is usual in Australia for white adults who know their skin is sun damaged to seek out an accredited skin cancer GP for a regular check. Granted, there are several differences. The incidence of melanoma and other skin cancers is higher there, GPs are allowed to treat skin cancer, there is excellent training and certification available, and patients generally pay to be seen. But based on what I observed in three clinics, this seems to work out well. The maximum price for a full skin check by an expert GP specialising in skin cancer was Aus$100 (about £53) some of which could be claimed back on insurance. This is generally affordable. One pub landlady I chatted with told me: “Two of my husbands died from melanoma, so I go for my regular skin check.”
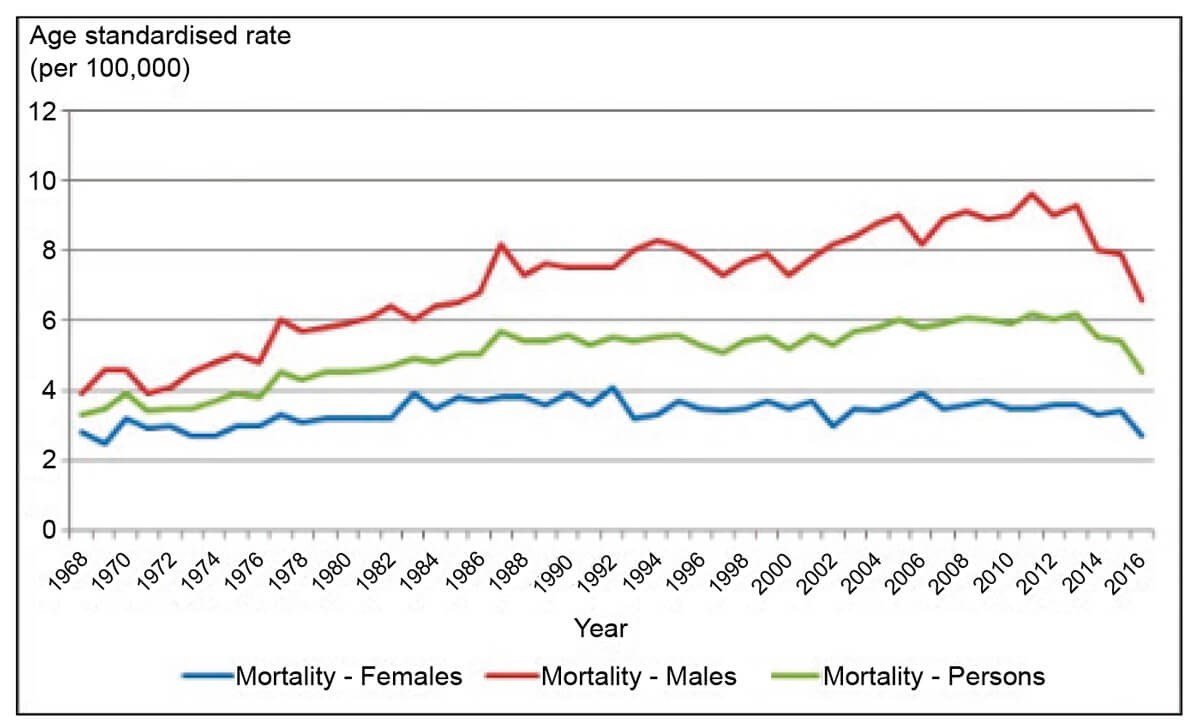
Figure 1: Age-standardised mortality rates for melanoma skin cancer, 1968 to 2016, by sex.
This information is reproduced with permission from Cancer Australia.
Very early melanomas detected by screening
Professor Rosendahl screens patients three days a week. He has rigorously audited his work for 10 years using the Skin Cancer Audit & Research Database (SCARD), and has a ‘hit rate’ (benign to malignant lesions excised ratio) of 3:1, and 80% of the melanomas he detects are at the in-situ stage (100% cure rate). I saw this being achieved by the expedient of meticulous scalp to sole skin examination, using dermoscopy and a digital recording device (FotoFinder), which enabled magnification, detecting pre-invasive melanoma way before the ‘typical’ features of melanoma became visible. In 20 years working with skin cancer I had never seen such early melanomas being caught. His screened patients almost never develop an advanced melanoma – they are caught early by intentional, scientific screening. He was shocked at my melanoma image collection; “You are detecting melanomas very late in Britain” was his observation.
Currently, a patient who wants a skin check could try seeing their GP. Good luck with that! They are worked off their feet, aren’t paid or tasked to provide routine skin checks, haven’t been trained, and lack modern technology. As for the NHS hospital dermatology service, generally only high-risk patients are screened. According to National Institute of Health & Care Excellence (NICE) guidelines, most melanoma patients are monitored for only 12 months, although the increased skin cancer risk is life-long. A recent study showed 8% of melanoma patients will get a second melanoma within five years (Lallas, Apalla, et al. American Journal of Academic Dermatology September 2019).
In short, I believe there is an argument for specialised full skin checks, ideally with full body photography, at an affordable price. If I had had a melanoma, I would like to have total body photography and an annual check for life. The NHS does not offer this. It could be delivered by suitably trained and skilled GPs and nurses, or other medics. You don’t have to be a dermatologist. The greater part of early melanoma detection consists of slow, meticulous inspection of the whole skin, with dermoscopy, ruling out benign lesion after benign lesion until a ‘pattern breaker’ lesion is found which requires action.
As the proverb goes, it isn’t rocket science. Training is available. Excellent online training leading to an international certificate is possible (e.g. https://www.skincancercourses.com/professional-certificate-of-dermoscopy) and many other learning opportunities exist, some are mentioned on my blog at www.dermoscopy.wordpress.com

Subtle pink and brown melanoma picked up on a routine skin check.
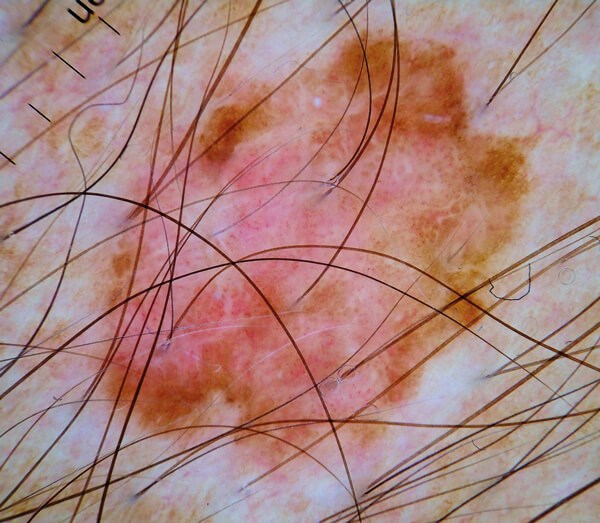
Subtle pink and brown melanoma picked up on a routine skin check.

Thin melanoma picked up on screening.
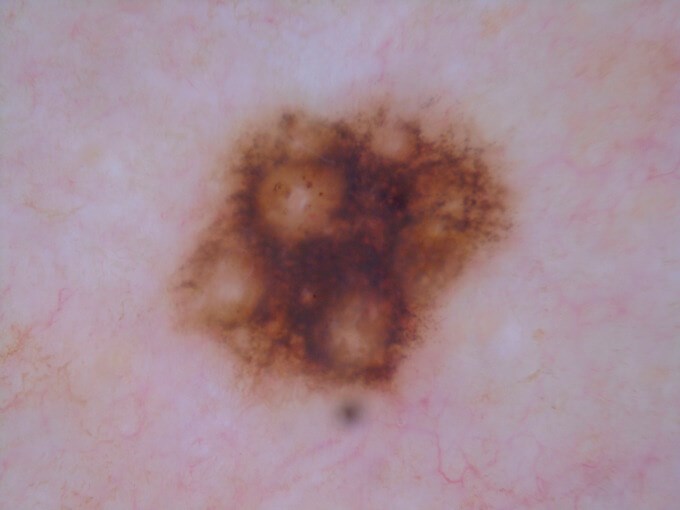
Thin melanoma picked up on screening.
Should we screen for melanoma?
The World Health Organisation (WHO) criteria developed by Wilson and Jungner in 1968 states that, to justify screening, a medical condition must be sufficiently important, have a recognisable early stage, an effective and acceptable test for the early stage, reasonable treatment, and the costs of early case finding and treatment must be “economically balanced”. Until now, melanoma was not thought to satisfy these criteria, but several parameters have changed. The incidence of melanoma has increased significantly. We now know much more about early stage melanoma and how to detect it. We have well validated detection tools our predecessors did not have (dermoscopy and sequential digital monitoring) and the cost of treating metastatic melanoma has shot up with the advent of immunotherapy and other targeted oncology agents.
Taking all these developments together, I am convinced that the case for screening, at least higher risk groups (over 100 naevi, personal history of skin cancer), is now very strong. However, there is no political push for it, and I can’t see the cash-strapped NHS offering screening in the foreseeable future. But I am quite sure that there is a growing need and demand which could be met on a willing seller, willing buyer basis. The Australians have shown the way – and their excellent skin cancer GPs have shown that you don’t need to be a consultant dermatologist to detect skin cancers at a much earlier stage. Training, equipment and affordability are the keys. The opportunity currently exists for a revolutionary step-change in early skin cancer detection.
COMMENTS ARE WELCOME









