
The provision of safe and effective ophthalmic care to large patient populations has always been challenging. Severe restrictions of outpatient clinical activity due to the COVID-19 crisis has compounded this problem, with 26,800 appointments cancelled in our unit in the first three months of the national lockdown. Inevitably, oculoplastic services across the world have also been affected, with a reduction in admission rates [1].
Units across the UK are rapidly redeveloping their services to encompass newer ways of working, including active clinical referral triage (ACRT) [2], teleophthalmology [3], enhanced discharge and shared care. These service redevelopment projects require baseline data of the number of patients seen in different subspecialties, as well as the distribution and type of referrals within each subspecialty. The latter data is often lacking, and we are anecdotally aware of the scarcity of such data for oculoplastics, even in units with electronic patient record systems.
The Tennent Institute of Ophthalmology in Glasgow provides a tertiary referral service for oculoplastics to 1.2 million people in the West of Scotland. This service is provided by six oculoplastics consultants across five hospitals and includes adnexal, lacrimal and orbital surgery. We retrospectively reviewed referral and clinical records of all patients referred to this service from 1 January 2017 to 31 December 2017, in order to determine the categories of referrals and treatment outcomes at first visit to the service. Referrals vetted to the ‘Minor Operations Clinic’ were excluded from this study.
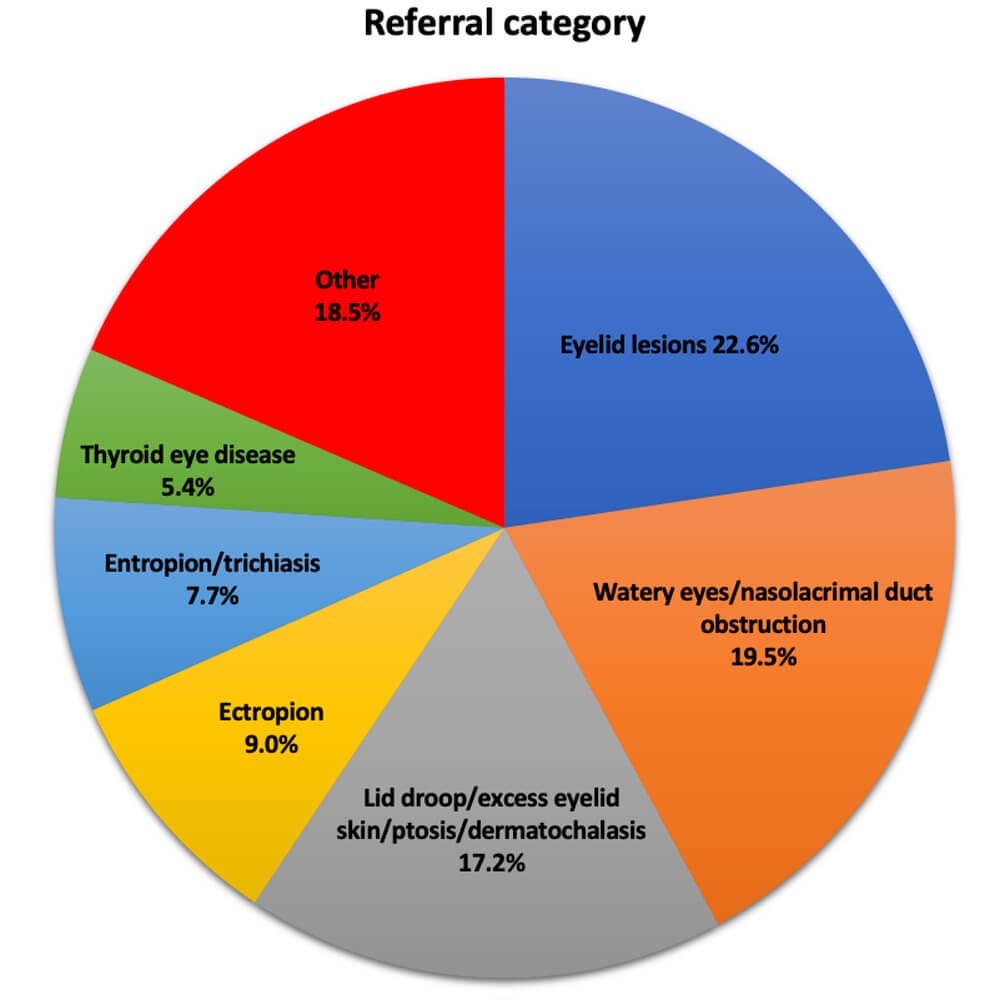
Figure 1: Referrals to the oculoplastics service over one year.
A total of 1581 new patients were seen in our oculoplastics service over the year. The descriptions used in the referrals were used to determine the referral categories of oculoplastic conditions and these are presented in Figure 1. The most common referral category was eyelid lesions (22.6%), followed by watery eyes / nasolacrimal duct obstruction (19.5%), lid droop / excess eyelid skin / ptosis / dermatochalasis (17.2%), ectropion (9.0%), entropion / trichiasis (7.7%) and thyroid eye disease (5.4%); 38.5% of all patients were listed for surgery at the first visit and 23.4% were discharged at this visit. A breakdown of these treatment outcomes is given in Table 1.
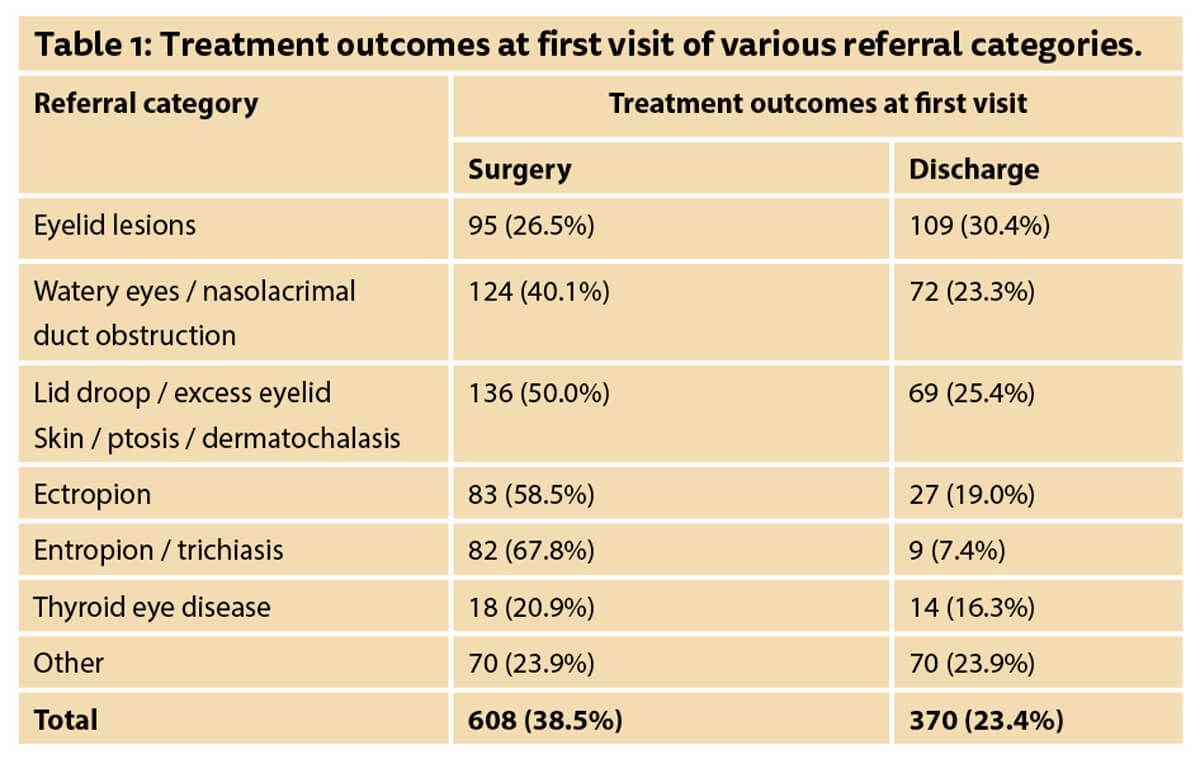
Our data has allowed us to construct a profile of our oculoplastics service and target areas for service redesign and improvement. For example, eyelid lesions formed the largest group of referrals and only 26.5 % were listed for surgery. Therefore, an image-based system is being developed for ACRT of these referrals. Similarly, watery eyes formed our second largest group and 59.9% of these patients were treated conservatively. We have therefore identified this group for video consultation clinics which are currently being piloted in our service.
We believe that our data can be useful to oculoplastics services across the country as they work to redesign their services in view of the current crisis. The development of teleophthalmology in oculoplastics will inevitably lead the way in the form of the use of digital photography and video consultations [3]. While there will undoubtedly be regional variations, our oculoplastics service profile can find application in multiple oculoplastics service improvement projects, especially where there may be a paucity of time or resource to conduct a similar analysis.
References
1. Lanni V, Iuliano A, Laezza MP, et al. Oculoplastic management of patients in the Covid-19 era: experience from an Italian tertiary referral center. Orbit 2020;15:1-3.
2. Scottish Government. Toolkit to support Active Clinical Referral Triage across NHS Scotland December 2019 Scottish Access Collaborative. Scottish Government; 2020
3. Kang S, Thomas PB, Sim DA, et al. Oculoplastic video-based telemedicine consultations: Covid-19 and beyond. Eye 2020;12:1-3.
COMMENTS ARE WELCOME










