The COVID-19 pandemic was one of the biggest challenges to face NHS workers. However, history has repeatedly shown that times of difficulty can result in the development of significant social and technological advances. We describe our own experience of this regarding the periocular skin cancer management service at Guys and St Thomas’ NHS Foundation Trust (GSTT) which emerged as a significantly more streamlined, cost-effective, patient-friendly and carbon neutral service as a result of the COVID-19 challenge.
Historically, all non-melanoma periocular skin cancer cases at GSTT received the gold standard treatment of Mohs micrographic surgery (MMS) followed by oculoplastic reconstruction. As is commonly the case, MMS was undertaken in the dermatology skin cancer and laser unit (DSLU) by experienced Mohs dermatologists, and the periocular reconstruction was undertaken by the oculoplastic team at a different time point, in their own eye theatres.
Although Mohs could continue during the pandemic, as the dermatological surgery and laser unit (DSLU) came under the essential ‘amber’ pathway, eye theatres were deemed a ‘green’ area, requiring periods of up to two weeks’ isolation before entry was allowed. This caused great disruption to the periocular skin cancer pathway and made the existing model untenable. While other amber pathways were theoretically possible through emergency theatres, this was not felt to be practical or sustainable in our unit. As a result, an alternative strategy of in-house specialist oculoplastic reconstruction within the DSLU was explored.
Concerns about such a transition to DSLU included the lack of laminar flow, lack of anaesthetic cover, absence of an operating microscope and the limited ophthalmic experience of the dermatology surgery nurses. However, a small number of patients with poor mobility or transport issues had been satisfactorily managed in this manner for many years prior, serving as a good feasibility cohort. Similarly, an internal audit of non-ophthalmic skin cancer cases, who had an established pathway of Mohs and same-day dermatological closure in DSLU, showed negligible infection rates. The use of surgical loupes was felt to provide satisfactory magnification for oculoplastic reconstructions and the dermatological staff were given additional training in oculoplastic instrumentation and surgical requirements. Reconstruction in eye theatres under general anaesthetic remained an option for patients who felt they were unable to tolerate local but, otherwise, the expectation was for all reconstructive surgeries to be carried out under local anaesthetic immediately after Mohs excision of the skin cancer. Thus, a novel periocular skin cancer integrated practice unit (IPU) was developed, based on pathology rather than historic hospital subspecialty divisions.
As well as the obvious benefit of patients being able to have their periocular reconstructions completed in a timely fashion during the COVID-19 pandemic, many other benefits of this new pathway soon emerged, resulting in its ongoing and increasing use. Most obvious was the reduced number of hospital visits required for the patient. Not only did patients combine their two surgical visits into one, but being under one centre rather than two obviated the need for separate pre-assessments. With time, the consultation and postoperative review system was also streamlined so that oculoplastic input became available within the DSLU at the time of initial consultation, and all first postoperative checks were undertaken by the oculoplastic surgeon at DSLU too. Three-month postoperative check-ups were moved to a telephone review, with any patients having functional or aesthetic concerns being able to return for a face-to-face (F2F) assessment. Unusually complex new referrals requiring an additional, more detailed ophthalmic examination would be booked for that within the eye department and the rare cases that required systemic oncological management were plugged into the non-melanoma skin cancer medical decision making (MDM). The new IPU and old two-site pathways are illustrated in Figures 1 and 2.
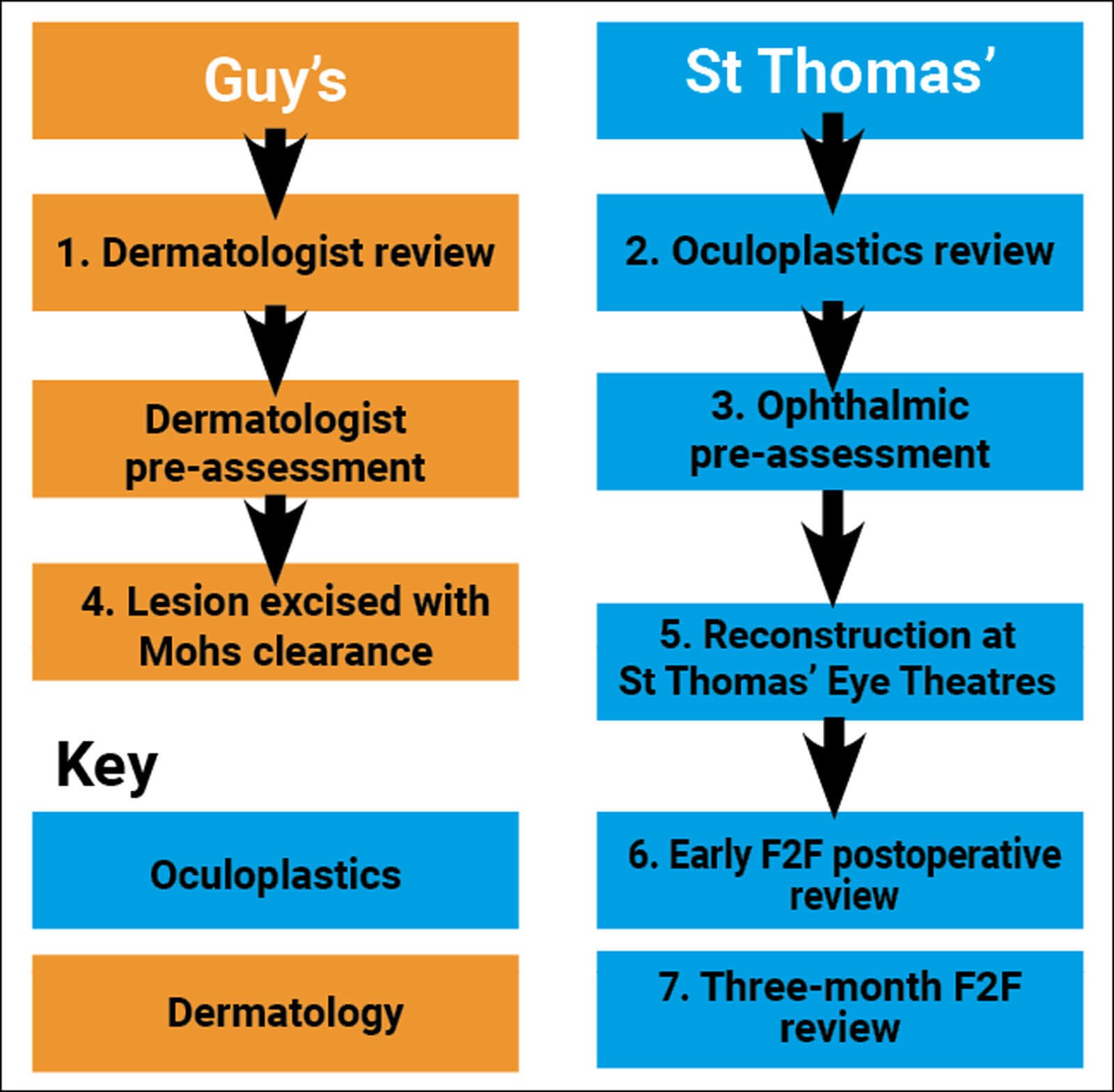
Figure 1: Historic two-site treatment pathway for patients with a localised, periocular, biopsy-positive, non-melanoma skin cancer referral to dermatology or ophthalmology. Numbers represent the count of each F2F visit. Non-numbered visits are telephone reviews.
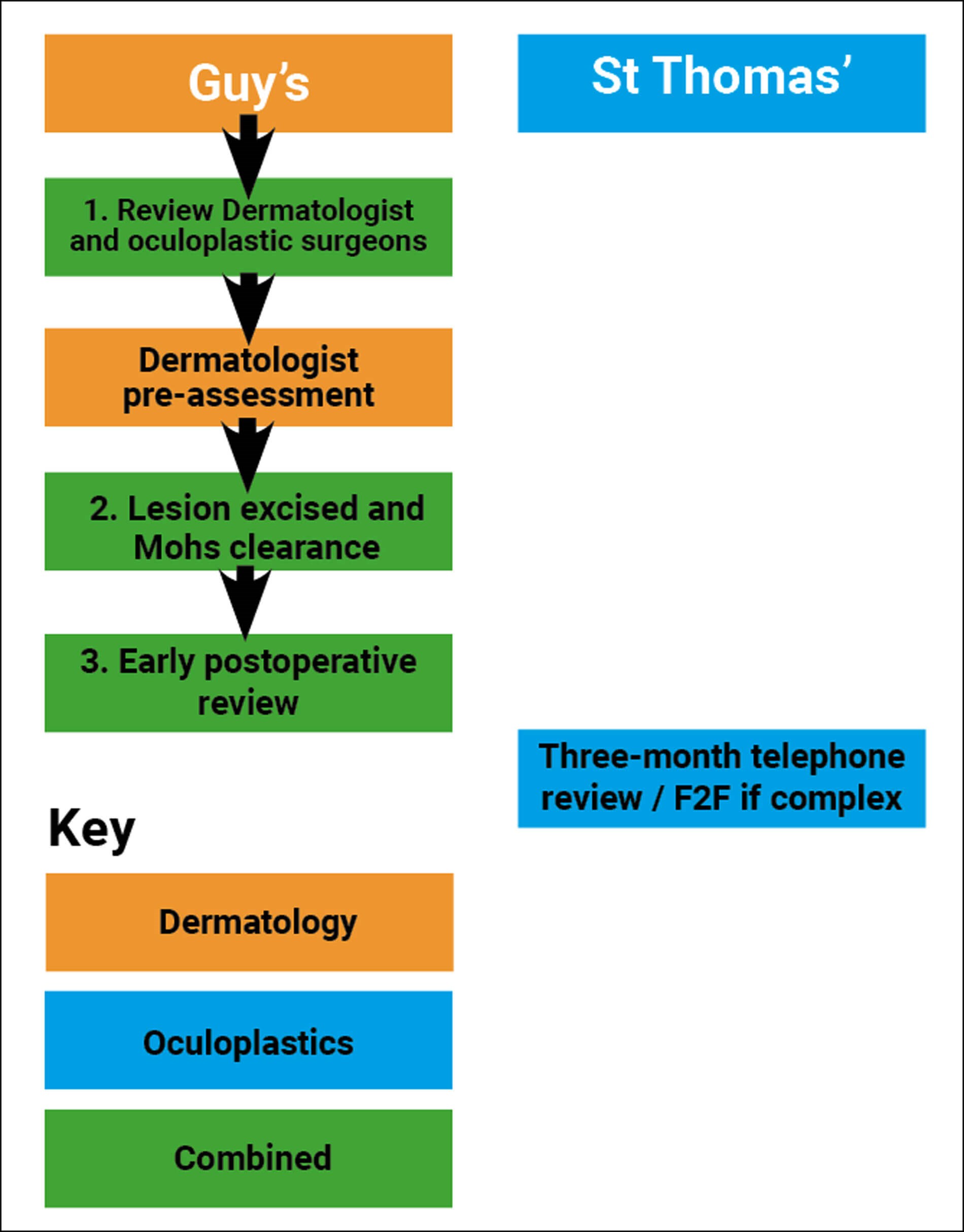
Figure 2: New IPU showing pathway for patients with a localised, periocular, biopsy-positive, non-melanoma skin cancer referral to dermatology or ophthalmology. Numbers represent the count of each F2F visit. Non-numbered visits are telephone reviews.
To better asses these advantages, a formal audit of the service was carried out, comparing patients treated in the old model for the six months from September to March 2020 (prior to COVID-19) to those treated in the novel IPU model from July 2020 to September 2022 (when the service opened again during and immediately after the pandemic). Data was collected on patient demographics, the rate of complications and the reported patient experience. Value to the healthcare system was assessed by the cost of each care episode both to the commissioners and to the patients. Lastly, in view of the recent NHS Green Plan initiative, the use of resources and improvements towards decarbonising were also considered.
A total of 52 patients were identified as having been treated on the old pathway over the six-month treatment period, equating to around 7.4 patients per month. Similarly, 135 patients were identified as having been treated on the new IPU pathway during the 27-month assessment period, equating to around five patients per month. This lower figure reflects repeated dermatology nursing staff deployment during the three COVID-19 lockdowns, as well as some impediments to referral pathways. Indeed, due to increased efficiencies with the new pathway, for the last year, throughput has increased beyond pre COVID-19 levels and the service has been treating around 10 cases per month.
Sociodemographics of the two treated groups were similar, with a mean age of 68 in the historic group and 69 in the new IPU one. Females constituted 52% of the former and 51% of the latter, and the proportion of London residents was similar at 35% and 31% respectively. Anticoagulation levels were also similar, at 25% in the historic and 24% in the IPU. However, there was a reduction in the proportion of diabetics from 15% in the historic to 10% in the IPU, as well as an even more pronounced drop in the proportion of smokers (12% compared to 4%). This is likely to reflect the higher COVID-19 morbidity and mortality amongst such patients during the pandemic and their resultant reduced use of the skin cancer pathway during the pandemic period.
Lesion characteristics were also similar between the two groups, with basal-cell carcinoma (BCCs) accounting for 90% of cases in the historic group and 89% in the IPU one. Recurrent lesions were found to be slightly higher in the IPU group (6%) as opposed to the historic group (4%) but the location of lesions was comparable across the periocular sites.
As demonstrated by the flow charts (Figures 1 and 2), the total number of clinical episodes reduced from eight on the old pathway to five with the new IPU model; a reduction of 40%. Proportionally, the number of F2F visits reduced by a greater degree, as the three-month review was also changed to a virtual consultation on the new pathway. This resulted in there only being three face-to-face episodes on the IPU pathway as opposed to seven on the older model; a reduction of 60%. Most significantly, the number of surgical attendances halved from two on the historic to one with the IPU. This latter point is significant as surgery is arguably the most expensive, administratively burdensome and stressful type of clinical episode for the patient.
Complications of surgery were slightly lower in the IPU group, with no infections noted, as opposed to one in the historic group. There was also a statistically significant reduction in subsequent revision surgery, which occurred in 13% of the historic group but only 4% of the IPU group (p<0.05). Both groups had one patient with an area of graft necrosis and one with a wound dehiscence.
To ascertain patient satisfaction, a consecutive three-month sample of patients treated on the new IPU pathway was contacted by telephone and asked to score their experience out of 10, as well as being asked whether they would prefer to have had their care under the old or new model. Only two of the 17 identified patients were uncontactable and those who answered gave an average satisfaction score of 9.9 out of 10. No patients would have preferred to have had treatment according to the old pre-COVID-19 pathway, specifically quoting same day Mohs and reconstructive surgery as a key advantage.
Assessing the precise financial costs of both pathways to the NHS was difficult but some broad trends were examined. Firstly, the saving to the local commissioners was estimated using the standard 2022/2023 ‘Payment by Results’ hospital tariffs. These listed a new consultation (doctor or nurse) at £173 and a follow up consultation (doctor or nurse, F2F or virtual) at £79. The new pathway reduced the number of new consultations by one and follow ups by one, resulting in a saving of £252 (£173 + £79). The potential saving of performing the oculoplastic surgery in DSLU rather than eye theatres was harder to quantify based on tariffs as the reconstruction could still potentially be classified under the same oculoplastic one. However, combining the surgery into one simultaneous event reduced other NHS costs caused by the need for operating space in both DSLU and eye theatres, such as staffing, administration, heating and lighting, and the requirement for laminar flow in the ophthalmic theatre.
In addition to NHS cost saving, there was a financial gain to the patient and their families. Our demographic analysis showed that 68% of patients came from outside London and therefore faced a considerable journey. We estimated that a return trip would cost an average of around £40, and either the patient or their accompanying partner would have to take at least half a day off work for a face-to-face visit (costing £75). This meant that the four saved visits with the IPU pathway presented an approximate cost saving of £460 (£115 x 4= £460 per patient). This financial gain, coupled with the reduction in inconvenience and stress that hospital visits can cause, was reflected in the fact that all patients questioned preferred the IPU model over the pre-COVID-19 model.
With environmental concerns becoming more pressing, we also looked at the reduction in carbon footprint of the new IPU pathway. The NHS Green Plan, Delivering a Net Zero Health Service, was released in October 2020 and committed the NHS, as Britain’s largest employer, to becoming the world’s first ‘net zero’ health service [1]. Three areas in which the report suggested the NHS could decarbonise were transport and travel, effective use of innovation, and heating and lighting – the IPU model has made major improvements in all of those.
Travel has historically represented 14% of NHS total emissions, and our new pathway has reduced F2F outpatient activity by 60%, well over the NHS Green Plan target of a 25% reduction. The new model also reflects innovative service redesign, as well as the increased use of technology through more virtual clinics. Lastly, the environmental burden of heating and lighting NHS estates, which comprises around 15% of NHS emissions, has been reduced by combining consultations and surgical procedures into one integrated patient unit. Furthermore, when designing a new specific oculoplastic surgical tray for the Mohs unit, we were careful to minimise instrumentation to that which was absolutely essential for our surgery. These sets therefore contain fewer instruments than standard oculoplastic lid ones in the eye theatres, thus improving our carbon footprint through a reduction in supply chain emissions and recycling of surgical instruments.
In conclusion, COVID-19 and its inherent restrictions provided a successful impetus for us to redesign the model of care for patients with periocular non-melanoma skin cancer. The resultant pathway has shifted the emphasis of care from traditional hospital specialty-based departments to a more patient-centred IPU. This more streamlined pathway has not shown any compromise in healthcare outcomes and has been extremely popular with patients who frequently find F2F hospital attendances, and in particular surgical ones, disruptive, stressful and expensive. With it, the new IPU pathway has brought cost savings of approximately £460 for patients, as well as at least £250 per patient for the commissioners.
The reduced clinical workload has also freed up capacity for increased throughput of cases and driven up the efficiency of our unit, reflected by our high throughput figures, short waiting times and our increased referrals from other units. Lastly, the new IPU model has offered an opportunity for our service to improve its carbon footprint, thus contributing significantly to the NHS Green Plan target of net zero by 2040 and exemplifying the role of innovation and service redesign in achieving this.
References
1. Delivering a ‘Net Zero’ National Health Service (2020/2022). NHS England.
https://www.england.nhs.uk/greenernhs/
publication/delivering-a-net-zero
-national-health-service
[all links last accessed October 2023]
COMMENTS ARE WELCOME










