Breast augmentation is a widely sought-after cosmetic procedure and has empowered individuals seeking aesthetic enhancement or reconstruction following mastectomy for breast cancer. Amid its popularity, the occurrence of implant rupture stands as a critical concern, impacting both physical wellbeing and psychological satisfaction. When considering complications of breast implant surgery, implant rupture is one of the most commonly stated concerns of patients.
The management of ruptured breast implants requires a nuanced understanding of risk factors, precise diagnosis, tailored surgical interventions, and postoperative care to ensure optimal outcomes. Revisional breast implant surgery can be difficult and may not always result in better cosmesis or outcomes for the individual. This article looks at the multifaceted realm of managing ruptured breast implants. It seeks to offer a guide for healthcare providers, navigating through the complexities of this challenging scenario.
Risk factors
The main risk factor for implant rupture is advancing age of the prosthesis [1]. Whereas it is not necessary to indicate to patients that their implants should be replaced after a certain period of time, if those implants are intact and otherwise not causing any symptoms, the risk of implant rupture is known to increase with advancing years. In modern implants, rupture prior to 20 years of implant age would be considered to be premature [2].
Earlier rupture may be related to a variety of manufacturing factors such as incompetent valves, manufacturing defects and underfilling of the implant (leading to folds in the implant capsule and causing stress-related fracture of the wall). These factors are more important where implants have been filled by the surgeon. Patient factors such as blunt-force trauma may also be related to rupture but modern implant construction is designed to minimise this risk.
Modern breast implants are often now provided with a lifetime manufacturer guarantee [3] whereby the company will pay for new breast implants in the event of rupture, although they will not always cover the full costs of revisional surgery and hospital fees.
Types of rupture
In general, breast implant failure with rupture is classified as either intracapsular or extracapsular, depending upon whether silicone has escaped out with the fibrous capsule that forms post-implant placement [4]. Where an extracapsular rupture occurs, the silicone may track into the lymphatic system and cause a regional lymphadenopathy. These silicone nodes give a classical ‘snowstorm’ appearance on ultrasound scan and may be seen in axillary or intra-mammary nodes.
In the US, saline implants were used commonly during the era where silicone implants were not approved by the Federal Drug Administration for cosmetic augmentation, and rupture of this type of implant normally leads to a rapid volume deflation of the breast and reabsorption of the saline.
Diagnosis
Breast implant rupture may present with a variety of symptoms or none at all [5]. A thorough history should be taken including the details of the original surgery, with type, volume and placement of the implant (if available), a history of trauma, the presence of any new lumps in the breast or axilla and any B-symptoms such as fever / night sweats / weight loss.
Examination may demonstrate a change in breast shape or symmetry, the presence of a new mass, associated lymphadenopathy or a change in the volume of the breast. As explained above, diagnosis of implant rupture in saline implants often does not require any further investigation.
Where breast implant rupture is suspected, a comprehensive triple assessment should take place. This involves clinical examination, imaging and any necessary pathology. In the UK, women under the age of 40 would typically be investigated by breast and axillary ultrasound scan. This can often show ‘snowstorm appearance’ of an extracapsular rupture or the ‘stepladder sign’ of an intracapsular rupture (a normal implant should usually be anechoic). In women over the age of 40, mammography should be performed as a routine. It can be difficult to ascertain whether implants have ruptured on mammography but this is essential to exclude a serious underlying lesion such as breast cancer or ductal carcinoma in situ (DCIS).
Where there is any doubt about the diagnosis then MRI can be undertaken, most often with gadolinium contrast injection.Where there is a collection of fluid seen this should be aspirated and sent for cytology, with particular reference to markers of adult large cell lymphoma (ALK and CD30) [6]. If a mass is seen then this would normally be core-biopsied. The exception to this may be benign appearing nodes that have a classical appearance of silicone adenopathy.
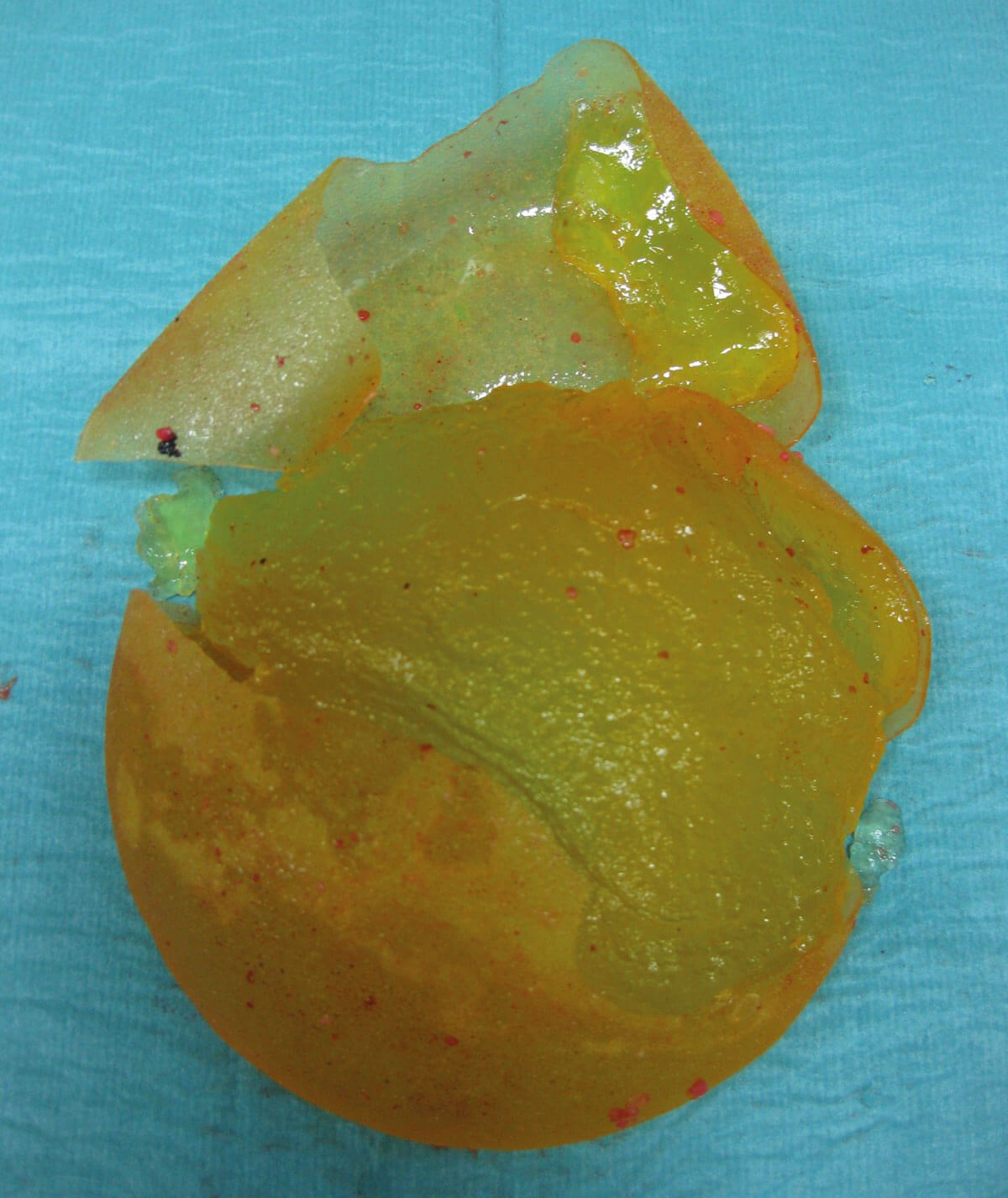
A ruptured silicone breast implant. As is often the case, the implant
details are undecipherable due to degradation and rupture.
Treatment of breast implant rupture
When breast implant rupture has been diagnosed, there are several options available. These include:
- Doing nothing – where there is no perceived cosmetic defect and the patient is otherwise asymptomatic this can be an acceptable course of action, albeit that with the time there is accumulating risk of silicone adenopathy.
- Removal of the implants – this may be combined with another uplift or volume replacement procedure to improve or maintain cosmesis [7]. All free silicone should be removed with a thorough washout. Total capsulectomy is not required but it is the authors’ practice to send routine capsule biopsies provided there is no palpable or visible abnormality at surgery (which would necessitate specific biopsy).
- Removal and replacement of the implants – the patient should be counselled as to the consequences of increasing or decreasing the volume of the implants, where decreasing volume then capsulorrhaphy should be undertaken, perhaps with mastopexy, and when increasing volume then capsulotomy should be performed.In any case, the patient should be carefully counselled about the likely cosmetic outcome, that symptoms may not always resolve and that if biopsies find an abnormality, then further treatment may be required.
Conclusion
In conclusion, managing ruptured breast implants encompasses a spectrum of considerations vital for effective healthcare delivery and patient satisfaction. The complexities of diagnosis, varying types of ruptures, and associated treatment options necessitate a nuanced approach. Understanding risk factors and the evolving landscape of implant technology is pivotal in addressing this concern. While surgical interventions exist, their outcomes may not always align with cosmetic expectations.
TAKE HOME MESSAGES
-
Breast implant rupture may be asymptomatic.
-
Initial investigations should be aimed at identifying patients with a delayed seroma who may have breast-implant related cancer.
-
Surgical options include implant removal and implant exchange, capsulectomy is not routinely indicated.
References
1. Hölmich LR, Friis S, Fryzek JP, et al. Incidence of silicone breast implant rupture. Arch Surg 2003;138(7):801–6.
2. Van Slyke AC, Carr NJ. Reply: Not all breast implants are equal: a 13-year review of implant longevity and reasons for explantation. Plast Reconstr Surg 2019;143(3):664e–5e.
3. https://www.gcaesthetics.com/surgeons/
solutions/surgical/breast-implants
[Link last accessed February 2024]
4. Hillard C, Fowler JD, Barta R, Cunningham B. Silicone breast implant rupture: a review. Gland Surg 2017;6(2):163–8.
5. Maxwell GP, Gabriel A. Breast implant rupture: causes, incidence, clinical impact, and management. Plast Reconstr Surg 2012;129(1):213e–8e.
6. Ravi-Kumar S, Sanaei O, Vasef M, et al. Anaplastic large cell lymphoma associated with breast implants. World J Plast Surg 2012;1(1):30–5.
7. Khan LR, Cartlidge CWJ. Improving cosmesis after breast implant removal. The PMFA Journal 2022;9(3):13–4.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME











