This article has been verified for CPD. Click the button below to answer a few
short questions and download a form to be included in your CPD folder.
Breast reconstruction following breast cancer surgery has positive physical and psychosocial health implications for individual patients [1]. Breast reconstruction also has significant socio-economic benefits for the population as a whole [2,3].
Breast conserving oncological surgery techniques have developed rapidly over the last decade and complementary reconstructive strategies have been developed to improve postoperative symmetry and appearance. A mastectomy is still often required for oncological clearance and breast reconstruction should be offered to all patients as a standard of care outlined in the National Institute for Health & Care Excellence (NICE) Breast Cancer Quality Standard [4]. Broadly, breast reconstruction can be considered in two major ways.
Firstly, breast reconstruction can be considered as a synchronous procedure during the same operation as the resectional surgery or it can be performed after the completion of oncological treatment as a secondary procedure. This is described as immediate versus delayed breast reconstruction. Each has benefits and drawbacks so a consultation with a reconstructive surgeon at the time of resection planning is recommended to ensure patients are fully informed about the potential options available to them.
The second consideration relates to the breast reconstruction technique, which can be broadly divided into either using implants or using a patient’s own body tissues. We describe this as implant-based versus autologous reconstruction. Again, each has advantages and disadvantages so careful planning is required to tailor a treatment plan for individual patients.
Lumpectomy, wide local excision and oncoplastic reconstruction
In selected patients with favourable pathology and anatomy, the above procedures can offer equivalent oncological control to a mastectomy while preserving breast tissue. At present, around half of all breast cancer resections are breast conserving procedures [5].
There are several techniques available to reconstruct a partial breast resection, most utilising the remaining breast tissue, a therapeutic mammaplasty, or recruiting local tissue as a flap, usually an intercostal artery perforator flap.
Therapeutic mammaplasty can be considered as a breast reduction where the reduced tissue contains the malignancy. A specialist reconstructive surgeon will be able to adapt the nipple pedicle and skin excision pattern to incorporate the resection and can potentially symmetrise the contralateral breast for size and shape match.
Reconstruction with a local pedicled flap depends on the location of the tumour within the breast. Both lateral and medial intercostal artery perforator flaps (LICAP and MICAP) can be utilised for small to medium volume reconstruction. A larger volume resection can be reconstructed with a thoracodorsal artery perforator (TDAP) flap or muscle sparing latissimus dorsi (MS-LD) flap.
Implant-based reconstruction is an option in breast conserving surgery but can only really be employed if no or minimal skin resection is required.
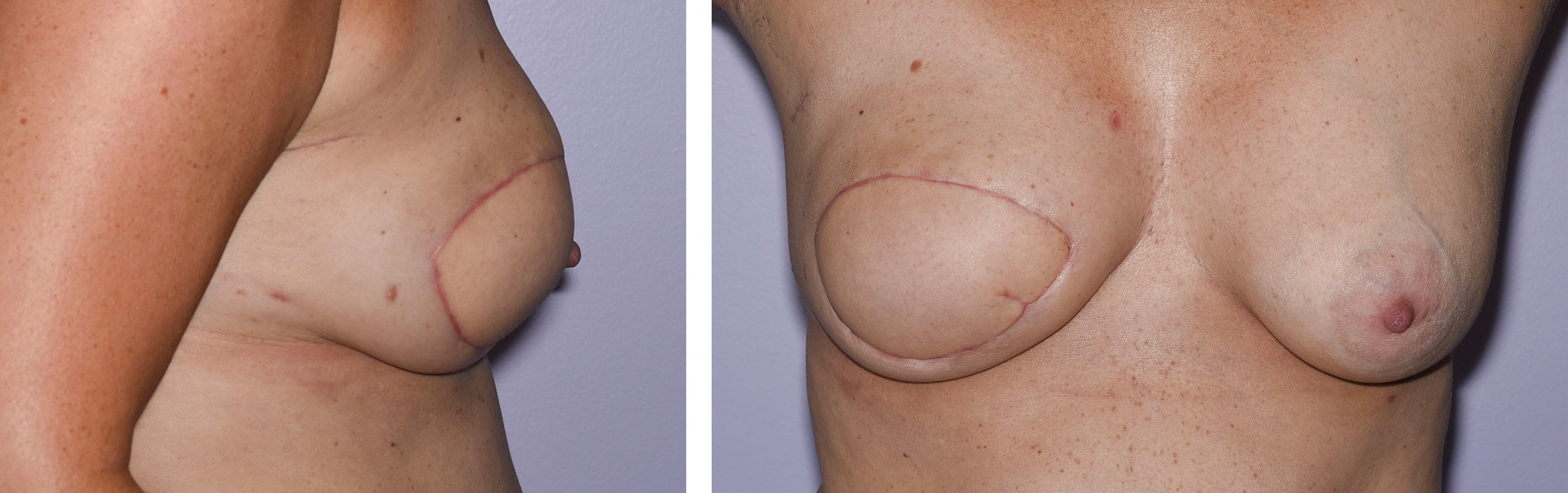
Figures 1a and 1b: Mastectomy and immediate free flap reconstruction - result at six weeks post operation.
Nipple reconstruction and lipomodelling declined by patient.
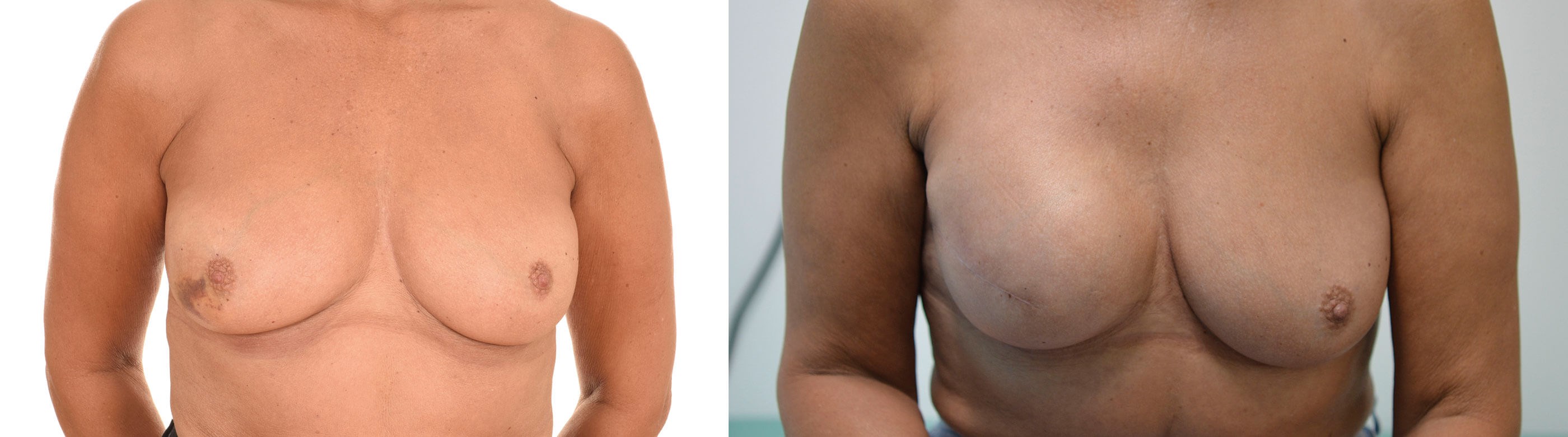
Figures 2a and 2b: Mastectomy and immediate reconstruction with implant and acellular dermal matrix.
Result after first stage reconstruction at eight weeks post operation.
Mastectomy reconstruction
Timing
Immediate reconstruction is gold standard for patients undergoing mastectomy. However, there are clinical circumstances and patient choices that impact on the decision-making process.
A skin-sparing or skin and nipple-sparing mastectomy permits the use of both implant-based and autologous-based immediate reconstruction options. A more radical mastectomy with significant skin resection does not permit immediate implant reconstruction. However, if the patient decides that implant-based reconstruction is right for them, an expander can be placed in the mastectomy pocket for future inflation before the definitive implant is used.
Free tissue transfer for breast reconstruction is the gold standard as it provides patients with a more natural result that will behave more like a native breast and age with a patient. There are various flaps that can be used, mostly commonly from the abdomen and thighs.
Delayed reconstruction is undertaken after completion of the oncologic surgery and adjuvant treatment. This allows patients the most predictable, least complicated and expedient recovery from breast cancer surgery. This comes at the price of living with the mastectomy scar for a period of time and a likely reduction in reconstructive options.
Adjuvant radiotherapy is a relative contraindication for implant-based reconstruction as the tissue expansion required before an implant can be inserted is often not sufficient. This is not a rule as some patients receive only a low dose of adjuvant radiotherapy and have adequate post-treatment skin quality, but the impact on skin health and healing globally is still a concern.
Delayed-immediate reconstruction seems like an oxymoron. It entails placement of an expander or implant in the mastectomy pocket assuming the needs for adjuvant postoperative treatment to maintain breast skin stretch for a more aesthetic final reconstruction [6].
Technique
Implant / expander reconstruction is a good choice for many patients. The ultimate goal being to replace the resected breast tissue with an implant of sufficient size and shape to match the contralateral breast, often with a symmetrising procedure to the contralateral breast. If a significant skin area is excised at the time of oncological resection or the reconstruction is delayed, the first stage of reconstruction involves the insertion of an expander over the breast footprint to recruit skin through mechanical and biological creep. The volume of the expander is gradually increased to and beyond the desired final implant size by injecting saline through the skin into the expander port located within or remote to the expander itself.
Once sufficient expansion has occurred the tissues are allowed time to stabilise before the expander is removed and replaced with a permanent silicone implant which more closely resembles breast tissue in shape and feel. If adequate skin remains after initial resection the definitive implant can be placed immediately without the need for expansion. The implant is usually anatomical or teardrop shaped and can be placed behind the pectoralis major to give a more natural breast take off, or an acellular dermal matrix (ADM) can be employed to disguise the implant under the mastectomy flap skin.
Secondary procedures to improve shape and size such as lipomodelling and scar revision can be utilised together with nipple reconstruction and areolar tattooing to enhance the overall aesthetic outcome.
Implant-based reconstruction has the advantage of being quicker and less invasive meaning operation length, hospital stay and recovery are reduced. The disadvantage is that the implant used is a foreign body and this is likely to need changing in the future. Complications of implant-based procedures include infection, breast implant illness (BII), capsular contracture and anaplastic large cell lymphoma (ALCL). The implant will also not feel and age like the contralateral native breast but for the right patient, wanting a relatively simple reconstruction with minimal downtime, implant-based reconstruction is a good option.
Autologous reconstruction uses a patient’s own body tissue. Historically this was a pedicled flap from the abdomen or back. The latissimus dorsi pedicled myocutaneous flap is still a reasonable option for some patients and it can be used as a lifeboat procedure, however more contemporaneous reconstructions involve the use of free tissue transfer.
A thorough patient assessment is required to define what options are available for each patient. The most common donor sites are the abdomen and inner thighs, but other flap donor locations such as the buttock remain in widespread use.
“Breast reconstruction should be offered to all mastectomy patients as a standard of care outlined in the NICE Breast Cancer Quality Standard”
By far the most common free flap of choice and the gold standard is the deep inferior epigastric artery perforator (DIEP) flap [7]. This is a flap utilising tissue from the lower abdomen, similar to that commonly discarded after an abdominoplasty. The skin and adipose tissue provide a reconstruction similar in consistency to a native breast and will have natural ptosis as the patient ages. The donor site morbidity is relatively low, the scar can be well hidden in the bikini line and the abdomen contouring can be a welcome bonus for a patient. Historically, this flap was harvested with the full width of the rectus abdominus muscle as a transverse rectus abdominus muscle (TRAM) flap. The first modification was the muscle-sparing TRAM where at least part of the muscle was left intact. These flaps are still used when the patient’s vascular anatomy dictates that muscle must be taken to ensure flap viability, but they can cause more donor morbidity.
The second most common donor site for free flap breast reconstruction is the upper inner thigh, namely the transverse upper gracilis (TUG) flap and the profunda artery perforator (PAP) flap. These flaps are excellent for patients who do not have sufficient abdominal soft tissue for a symmetrical reconstruction. They do not offer the same volume of tissue as the abdomen so can only be used for relatively small reconstructions. They are regularly used, ‘stacked’ where the flaps are harvested bilaterally, and transferred together to provide symmetry [8]. The donor morbidity is low, the scar well concealed in the upper thigh crease and there is an element of thigh contouring due to flap harvest.
The benefits of using autologous tissue for reconstruction is that it is natural. It feels and behaves much more like breast tissue and once completed, the reconstruction will last for a lifetime. The downside of autologous reconstruction is the complexity of surgery required that increases operative time, hospital stay and recovery. However, informed patients are regularly willing to undergo a longer procedure in the knowledge that it will ultimately lead to the optimal reconstructive outcome.
Adjunct procedures
After the initial surgery to create the breast mound there are several minor procedures that can be undertaken to add finesse to a reconstruction. These include lipomodelling for contour enhancement, nipple reconstruction and scar revision for maximum symmetry. Often these can be undertaken under local anaesthetic and are day case procedures. Contralateral symmetrising mastopexy or breast reduction are also options available for appropriate patients.
Useful websites
- https://www.bapras.org.uk/professionals/clinical-guidance
- https://associationofbreastsurgery.org.uk/media/382982/oncoplastic-reconstructive-surgery-v9ii.pdf
Declaration of competing interests: None declared.
References
1. Chen W, Lv X, Xu X, et al. Meta-analysis for psychological impact of breast reconstruction in patients with breast cancer. Breast Cancer 2018;25:464-9.
2. Wei CH, Scott AM, Price AN, et al. Psychosocial and sexual wellbeing following nipple-sparing mastectomy and reconstruction. Breast Journal 2016;22(1):10-7.
3. Department of Health, Macmillan Cancer Support and HNS Improvement. Living with & beyond cancer: taking action to improve outcomes (an update to the 2010 The National Cancer Survivorship Initiative Vision). 2013
https://www.gov.uk/government/
publications/living-with-and-beyond-cancer
-taking-action-to-improve-outcomes
[Last accessed 11 July 2022].
4. De La Cruz L, Blankenship SA, Chatterjee A, et al. Outcomes after oncoplastic breast-conserving surgery in breast cancer patients: a systematic literature review. Ann Surg Oncol 2016;23:3247-58.
5. Gilmour A, Cutress R, Gandhi A, et al. Oncoplastic breast surgery: A guide to good practice. Eur J Surg Oncol 2021;47(9):2272-85.
6. Kronowitz SJ, Hunt KK, Kuerer HM, et al. Delayed-immediate breast reconstruction. Plastic and Reconstructive Surgery 2004;113(6):1617-28.
7. McAllister P, Teo I, Chin K, et al. Bilateral breast reconstruction with abdominal free flaps: a single centre, single surgeon retrospective review of 55 consecutive patients. Plastic Surgery International 2016;6085624.
8. Yoo A, Palines PA, Maier MA, et al. Autologous breast reconstruction with bilateral stacked free flaps in massive weight loss patients. Plastic and Reconstructive Surgery - Global Open 2022;10(3):e4186.
COMMENTS ARE WELCOME











