External ear reconstruction can be challenging. Baskaran Ranganathan and Amr Abdelhamid describe how careful assessment, planning and surgery following the subunit principles and reconstructive ladder will ultimately lead to good aesthetic outcomes with restored form and function.
The external ear, specifically the auricle, is subjected to ultraviolet radiation and consequently, like the rest of the face, is more liable to pre-neoplastic and neoplastic lesions that include basal cell carcinoma and squamous cell carcinoma.
Basal cell carcinoma (BCC) accounts for more than 90% of cutaneous malignant lesions within the head and neck region and is therefore the most common malignant cutaneous lesion in the external ear. The majority arise on the auricle or periauricular region, though occasionally they may arise or extend into the external auditory canal.
Studies have also shown that BCC in the middle of the face, followed by auricular and periauricular areas, has the highest rate of recurrence which can make management of such cases challenging. Specifically, the external ear, because of its curvatures and uneven anatomical surfaces, can confuse the assessment of the lesion boundaries which can then lead to incomplete excision margins as well as high recurrence rates. Therefore, the gold standard technique for high-risk and recurrent BCC is Mohs surgery and second-stage reconstruction. Mohs surgery offers microscopic control of tumour excision, especially with clinically unpredictable cancerous outgrowths. Moreover, it offers maximum conservation of normal tissues which is extremely important in the ear. Preserving the cartilaginous framework of the ear will lead to better reconstruction and more favourable and pleasing aesthetic outcomes.
Assessment and reconstruction
In assessment, excision and reconstruction of lesions in the external ear, one should follow the principles of aesthetic subunits and follow the reconstructive ladder, starting with secondary intention healing, primary closure, skin grafts and flaps. The goal of reconstruction is to recreate an ear symmetrical to the opposite side in orientation, size and shape which makes ear reconstruction very challenging.
Helix and antihelix
For lesions that leave a defect up to 1.5cm involving the helix and antihelix, these can be excised with wedge excision and primary closure. Burrow’s triangles of skin and cartilage on either side of the wedge are often required to facilitate primary closure. Other modifications include crescentic or star excision, which allow better closure as they allow distribution of the tension throughout the auricle. Patients must be made aware that with primary excision and reconstruction, the vertical height of the ear will decrease as compared to the other side, however in most cases it is unnoticeable.
“Basal cell carcinoma accounts for more than 90% of cutaneous malignant lesions within the head and neck region and is therefore the most common malignant cutaneous lesion in the external ear”
For reconstruction of larger defects, up to 2cm, we would advocate the use of local advancement flaps – most commonly the Anita Buch chondrocutaneous advancement flap. This is particularly useful for upper third helical rim defects. This technique offers better cosmetic outcomes with preserved auricular anatomical landmarks and has very low risk of flap necrosis. Other local advancement flaps include the post-auricular advancement flaps, as the post-auricular area is one of the areas of skin reservoirs making it an ideal donor site for reconstruction.
In case of larger defects, more than 2.5cm, with substantial loss of tissue with bigger resections or in cases of human or animal bite, these may require partial pinna reconstruction using autologous costal cartilage grafts covered by temproparietal fascia flap and skin grafts.
Finally, the use of composite grafts from the opposite ear has also been described for helical reconstruction although, in our experience, they can have unpredictable results, thus we prefer the previously mentioned options.
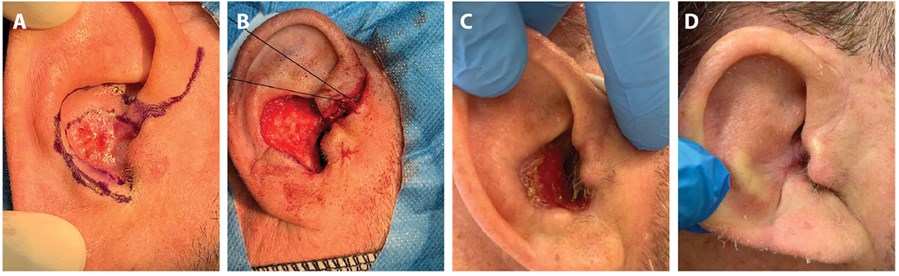
Figure 1A) Interoperative marking of conchal bowl BCC. B) Intraoperative picture demonstrating the defect after lesion excision. C) Postoperative picture at four weeks of secondary intention healing. D) Postoperative picture at 12 weeks.
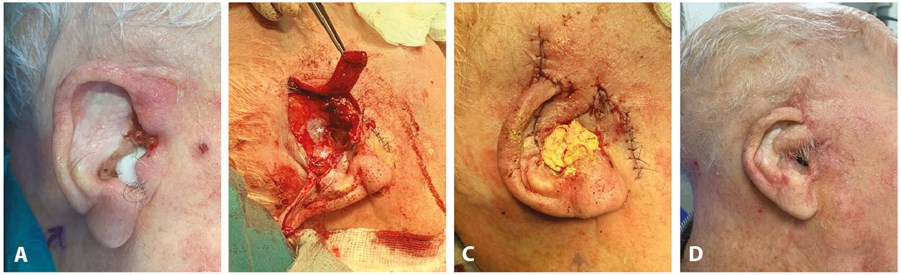
Figure 2A) Interoperative picture demonstrating concha bowl recurrent infiltrative BCC. B) Intraoperative picture following excision with pre-auricular flap used for reconstruction and temporalisfascia grafts (astrix) to line the exposed external auditoty canal. C) Immediate postoperative result. D) Postop result at 12 weeks.
Conchal bowl
The conchal bowl is a portion of the outer ear that is not structurally essential for support, hence it allows greater flexibility and choices used for reconstruction. For small skin defects with preserved cartilage perichondrium, options include healing by secondary intention (Figure 1) or skin grafts which can be particularly useful in high-risk patients with significant comorbidities. If the perichondrium is compromised, then the cartilage should be excised and full thickness skin grafts. Most common donor sites include postauricular or supraclavicular areas.
“For reconstruction of larger defects, up to 2cm, we would advocate the use of local advancement flaps – most commonly the Anita Buch chondrocutaneous advancement flap”
In case of large, full thickness defects we recommend the use of local flaps which can be pre-auricular or post-auricular flaps. The most commonly used flap is the post-auricular island flap which was originally described by Masson in 1972, and then its later modifications by Talmi, Rodendo and Jackson. This is a very robust flap due to the rich vascular supply of this area, auricular branch of posterior auricular artery and superficial temporal artery; the risk of flap necrosis is minimal. It can be utilised to cover defects involving helix, scaphoid fossa, concha and even lesions extending into the external auditory canal. It has the benefits of a single-stage procedure that provides adequate cover to exposed cartilage and helps resurface complex auricular defects, maintaining the three-dimensional shape of the ear. In addition, it offers minimal donor site morbidity with primary closure and a well-hidden scar.
Lesions extending into external auditory canal
The most challenging situation in external ear lesions and reconstruction is when the lesion or defect extends into the external auditory canal. In our experience in such situations, we approach this with an endaural incision that allows access and adequate exposure into the external auditory canal skin to ensure adequate excision with safety margins, then provides easy access for reconstruction. One of the significant postoperative complications if the external auditory canal is involved is external auditory canal stenosis. This is avoided by performing meatoplasty as part of the reconstruction and packing the external auditory canal with BIPP dressing for four to six weeks.
Conclusion
External ear reconstruction can be challenging. However, careful assessment, planning and execution following the subunit principles and reconstructive ladder will ultimately lead to pleasant aesthetic outcomes with restored form and function.
Further reading
1. Armin BB, Ruder RO, Azizadeh B. Partial auricular reconstruction. Seminars in plastic surgery 2011;25(4):249-56.
2. Golash A, Bera S, Kanoi AV, Golash A. The Revolving Door Flap: Revisiting an Elegant but Forgotten Flap for Ear Defect Reconstruction. Indian Journal of Plastic Surgery 2020;53(01):64-70.
3. Pickrell BB, Hughes CD, Maricevich RS. Partial ear defects. In Seminars in plastic surgery 2017;31(3):134-40).
COMMENTS ARE WELCOME










