Describing an approach to the straightforward and reliable flip-flop axial flap for reconstruction of the conchal bowl subunit of the auricle. The ‘flip-flop’ flap describes an axial subcutaneous island flap lying between the auricular sulcus and mastoid process. The flap is supplied by the auricular branch of the posterior auricular artery, occasionally with an additional contribution from the superficial temporal artery [1]. The flap is wholly fasiocutaneous in nature, though can be extended deeper to create a myocutaneous flap [2].
The flap was initially described in 1972 for the reconstruction of defects of the concha and medial rim of the anti-helix following skin malignancy excision [3]. The term ‘flip-flop’ appeared in the 1990s and variations have been reported to reconstruct auricular defects in the triangular fossa and the upper-third zone anti-helix [4,5]. Additionally, the flap can be used to reconstruct defects following harvesting of a perichondrial cutaneous graft for reconstruction at other sites, most commonly the nasal alar and nasal tip.
The lesion is marked and excised with clear surgical margins in accordance with established guidelines, followed by cleaning and draping of the pinna and post-auricular area [6,7]. If more than 50% of the conchal bowl subunit is lost, excision of the whole subunit is advised to aid reconstruction. Primary closure and grafting of this site is virtually impossible once underlying cartilage has been excised. The size of the defect is measured in millimetres in both the superior-inferior / vertical plane and anterior-posterior / horizontal plane.
“It is important that an additional 10% is added to these lengths when planning the reconstruction to minimise tension at the reconstruction site and to account for wound contracture during further healing”
It is important that an additional 10% is added to these lengths when planning the reconstruction to minimise tension at the reconstruction site and to account for wound contracture during further healing. Whilst Krespi et al. described the maximum dimensions of the flap to be 6x6cm, in our experience this is an upper rather than maximal limit [8]. Increases in flap surface area above 36cm2 have allowed safe reconstruction of the external auditory meatus and the middle-third zone anti-helix in our series.
The pinna is cleaned with 10% providone-iodine and the area draped as per surgeons’ preferred style. The excision site is then infiltrated slowly with Lignospan special (2% lidocaine with 1:80000 adrenaline), followed by the donor site. Massaging these sites after infiltration facilitates diffusion through the tissue planes and improves local vasoconstriction. Lesion excision and development of the flap are accompanied by limited spot bipolar diathermy to maintain the axial and random elements of the flap’s blood supply.
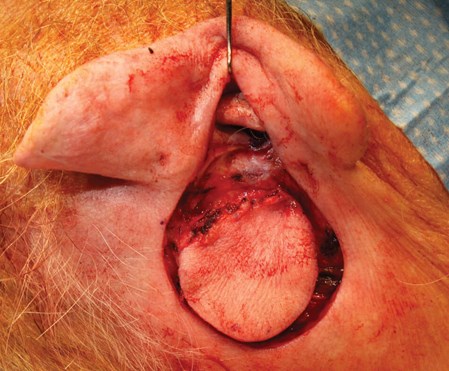
Figure 1: Deep flap dissection to the muscle layer, matching defect size and shape.
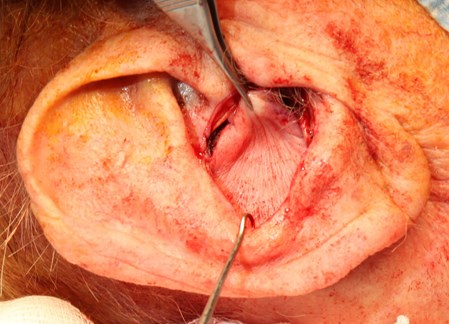
Figure 2: Flap delivery through the defect and secured anteriorly.

Figure 3: Flap closure around the defect with good wound edge eversion.
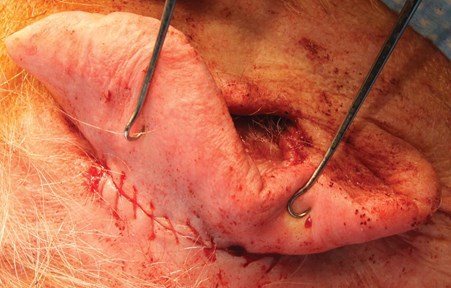
Figure 4: Completed posterior closure between the excision and donor sites posterior rims.
Dissection of the flap should remain perpendicular to the surface to prevent inward bevelling that can disrupt the axial pattern of its blood supply (Figure 1). Extension to the muscle layer improves rotation and provides additional calibre for larger defects, particularly when the lower-third zone anti-helix has been removed. The island is then delivered through the defect and sutured initially to the posterior half of the external auditory meatus (Figure 2). This secures the flap in place and reduces the handling required as the remainder of the flap is sutured to the edge of the primary defect. Interrupted vertical mattress sutures with 5-0 prolene are used to provide good wound edge eversion to facilitate healing (Figure 3). These are removed seven days after surgery to limit the foreign body reaction and to allow flap and donor site status to be assessed.
The posterior defect between the posterior rim of the excision and donor sites are sutured together using a continuous 4-0 vicryl rapide (Figure 4). This post-auricular wound and the conchal bowl region are protected by Jelonet (paraffin) gauze dressing with five 10x10cm dry gauze pieces. A head bandage is then applied, with gauze packing dissipating the pressure from the bandage. The head bandage remains in place during the first postoperative night and removed the following morning.
TAKE HOME MESSAGE
-
Excising the whole conchal bowl subunit is advised to aid reconstruction if over 50% of the subunit is lost.
-
An additional 10% is included to reconstruction measurements when designing the flap to minimise wound tension.
-
Suturing the island as close as possible to the posterior external auditory meatus facilitates closure of the flap onto the auricular remnant.
-
The flip-flop flap can be used to reconstruct auricular defects in the triangular fossa.
References:
1. Kolhe PS, Leonard AG. The posterior auricular flap: anatomical studies. Br J Plast Surg 1987;40(6):562-9.
2. Talmi YP, Liokumovitch P, Wolf M, et al. Anatomy of the postauricular island ‘revolving door’ flap (‘flip-flop’ flap). Ann Plast Surg 1997;39(6):603-7.
3. Masson JK. A simple island flap for reconstruction of concha-helix defects. Br J Plast Surg 1972;25(4):399-403.
4. Talmi YP, Horowitz Z, Bedrin L, Kronenberg J. Auricular reconstruction with a postauricular myocutaneous island flap: flip-flop flap. Plast Reconstr Surg 1996;98(7):1191-9.
5. Oh MJ, Kang SJ, Sun H. A simple modified flip-flop flap for the reconstruction of antihelix and triangular fossa defects. Arch Plast Surg 2016;43(1):122-4.
6. Newlands C, Currie R, Memon A, et al. Non-melanoma skin cancer: United Kingdom multidisciplinary guidelines. J Laryngol Otol 2016;130(S2):S125-132.
7. Ahmed OA, Kelly C. Head and neck melanoma (excluding ocular melanoma): United Kingdom multidisciplinary guidelines. J Laryngol Otol 2016;130(S2):S133-141.
8. Krespi YP, Pate Jr BR. Auricular reconstruction using postauricular myocutaneous flap. Laryngoscope 1994;104(6):778-80.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME










