All aesthetic practitioners will face complications during their career. It is therefore vital to be prepared. Dr Nestor Demosthenous provides a comprehensive guide to potential complications when treating patients with fillers.
A complication during or following a treatment carried out by any practitioner can occur to any patient, at any time. While serious complications are rare, our treatments inherently carry associated risks. In medicine, a complication can be defined as “an unanticipated problem that arises following, and is a result of, a procedure, treatment, or illness. A complication is so named because it complicates the situation” [1].
The more invasive the treatment, the greater the severity of the risk. (Editor’s comment - The question of what constitutes an invasive procedure is a difficult one. As a houseman I realised that it is far easier to kill a patient at the end of a needle than it is to kill them at the end of knife. - Andrew Burd.) Careful assessment, history taking, diagnosis, planning and execution of the treatment are all important factors to reducing the risk of a complication occurring. In this article we will examine which patient factors should be considered, discuss cautions and contraindications as well as considerations before embarking on a filler treatment. We will also look at what we can do pre, peri and post treatment to minimise the risk of complications. Lastly, we will look into how to identify early and late onset complications.
In his book Complications: A Surgeon’s Notes on an Imperfect Science, Atul Gawande discusses weekly mortality and morbidity meetings and concludes that “mistakes are an inevitable part of medicine” [2]. We will all have a complication, if not several, throughout our careers. The General Medical Council stresses the importance of our professional duty of candour [3]. We must be open and honest with our patients, our colleagues and ourselves when things go wrong. Because things will go wrong. We must know how to recognise them when they do, correct them, or seek help if we can’t.
Minimising risks: pre-treatment
A wide range of dermal fillers are available for use in facial aesthetics [4]. All are potentially capable of causing complications [5]. The EU’s Medical Device Regulation (2017/745) now expressly classifies dermal fillers as medical devices [6]. Therefore, as with any medical treatment, we must take a thorough history. “Careful attention to patient selection, education, and injection technique can minimise the incidence of complications, and an understanding of the early signs of complications and their proactive management can decrease their impact [7].”
In 2015 De Boulle et al. collated their experience of complications as well as conducting a literature review of PubMed and Ovid Medline databases, searching the terms “complications” OR “soft filler complications” OR “injectable complications” AND “dermal fillers” [7]. They then looked at factors which had influenced the complications discussed. Patient selection was a core topic of concern. They described refraining from treating an inappropriate patient as the “first and crucial step in avoiding complications with dermal fillers”.
Patient factors
The importance of a comprehensive medical history has been well documented in aesthetics [8]. It includes a past medical history (to establish any contraindications or cautions to be considered), social history (smokers have a delayed healing time), drug and allergy history, and an aesthetic and surgical history [8]. Knowing whether a patient has recently had a filler, which one, where and with whom, can help avoid complications of a reaction, infection and overfilling. A history of surgery to an area a patient wants treated is equally important. For example, a previous surgical rhinoplasty can, in itself, be a reason for some practitioners to not treat the nose due to the altered anatomy resulting in potentially increased risk of skin necrosis and / or blindness.
Managing patient expectations helps to minimise patient dissatisfaction as well as complications [9]. Caution should be exercised when confronting an individual who exhibits signs of an underlying mental disturbance or dysmorphic tendencies [7]. The treatment of body dysmorphic disorder is rarely, if ever, an aesthetic treatment. The importance of psychological screening in aesthetic medicine is becoming increasingly evident [10].
Contraindications
Contraindications can be absolute or down to a physician’s discretion. De Boulle et al. offer a convenient way of considering patient-related factors by dividing them into skin-related or systemic factors and also provide a comprehensive list of conditions considered to be a contraindication to treatment or warranting caution in the use if dermal fillers [7]. It is important to note that contraindications provided by the manufacturer of a filler should be adhered to (mainly related to the product constituents or excipients).
Patients with multiple or severe allergies should not be treated [7]. Patients with abnormally thin skin or skin atrophy (e.g. cortico-steroid induced) are not suitable for superficial or medium depth placed fillers. Infections (viral such as HSV, HPV), bacterial (streptococci or staphylococci) or yeast infections in, or adjacent to, the region to be treated can overwhelm the site and lead to complications [7]. Propionibacterium acne anywhere on the face is a complete contraindication to treatment for some clinicians. Treatment to an area of active dermatitis (inflammatory dermatitis, allergic contact dermatitis, seborrheic dermatitis) may result in a further flare up and have negative consequences [7]. Clinicians must consider delaying injectable treatment until these lesions have been treated and resolved.
Patients with infections such as sinusitis, periodontal disease, ear, nose, or throat infections, or dental abscesses should not be treated until the condition has resolved [11]. Increasingly, clinical evidence is emerging indicating that these infections might subsequently invade implanted filler areas, inducing biofilm reactions [11].
Cautions
Wound healing, and all conditions that may affect this, should be considered a contraindication or caution. Diabetics and smokers exhibit delayed healing. Auto-immune conditions where patients are on immunosuppressants (e.g. methotrexate for rheumatoid arthritis) may have an increased risk of infection. Conditions with altered healing such Ehlers Danlos, Marfans and systemic lupus erythematosus may be a cause for declining treatment or for referring the patient. In all these examples, an open and honest conversation about the merits and risks of treatments must be discussed with the patient.
Practitioners are cautioned regarding coagulation disorders and medications (e.g. aspirin, rivaroxaban, warfarin) as this could transform a simple bruise into a haematoma (may require drainage), which in itself may become infected and carry further need for treatment. Once again, identified increased risks should be discussed with patients.
Considerations
Some of the contraindications mentioned are not absolute. These, along with the cautions, should all be considered and measures put in place to minimise risks. Factors to consider include: the timing of treatments (e.g. how soon before or after one treatment follows another), whether patients should be referred to a more experienced colleague, whether it is necessary to liaise with the patient’s GP, dentist or specialist, and whether we should proceed at a slower pace (for example, a smaller amount of filler volume over a greater number of treatment sessions).
“We must be open and honest with our patients, our colleagues and ourselves when things go wrong”
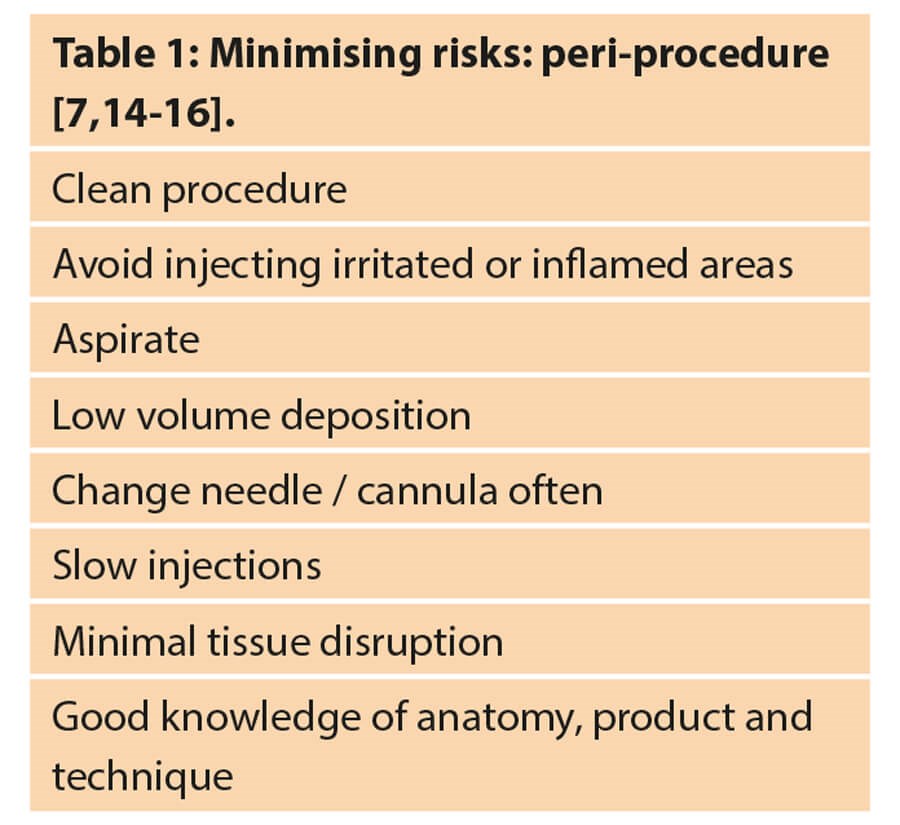
Minimising risks: peri-treatment
Every step of the treatment should be deliberate and considered. First, and foremost, we must have a clear treatment plan, and an understanding of the relevant anatomy, risks involved and protocols in place to initiate treatment should a complication arise [12].
The procedure must be carried out in the cleanest possible environment. Practitioners must clean their hands, and that of their patients (as they have a habit of touching their face). Gloves must be worn. Any material placed under the skin should be injected under sterile conditions using asceptic technique [7]. The patient’s skin should be cleansed, degreased and disinfected [7]. There are several antimicrobial agents available. Hypochlorous acid solutions are gaining popularity as they are kinder to skin than alcohol-based solutions and have strong microbicidal and anti-biofilm properties [13]. Table 1 summarises ways of minimising risks during a procedure.
Minimising risks: post-procedure
During the consent process we should advise patients of what to expect following treatment, as well as describe any instructions they need to follow. Following the treatment, we should re-visit these, as well as give the patient written post-treatment instructions (for example, keeping the area clean, avoiding intense heat, etc.) Patients should be encouraged to contact their practitioner with any concerns sooner rather than later. A follow-up appointment should be arranged. De Boulle et al. advise against re-treatment within a two-week window due to oedema and extravasation of blood in the area [7].
Complications
Identifying a complication once it has occurred and either initiating treatment or referring a patient to a more experienced colleague is the cornerstone of managing the complication and decreasing morbidity.
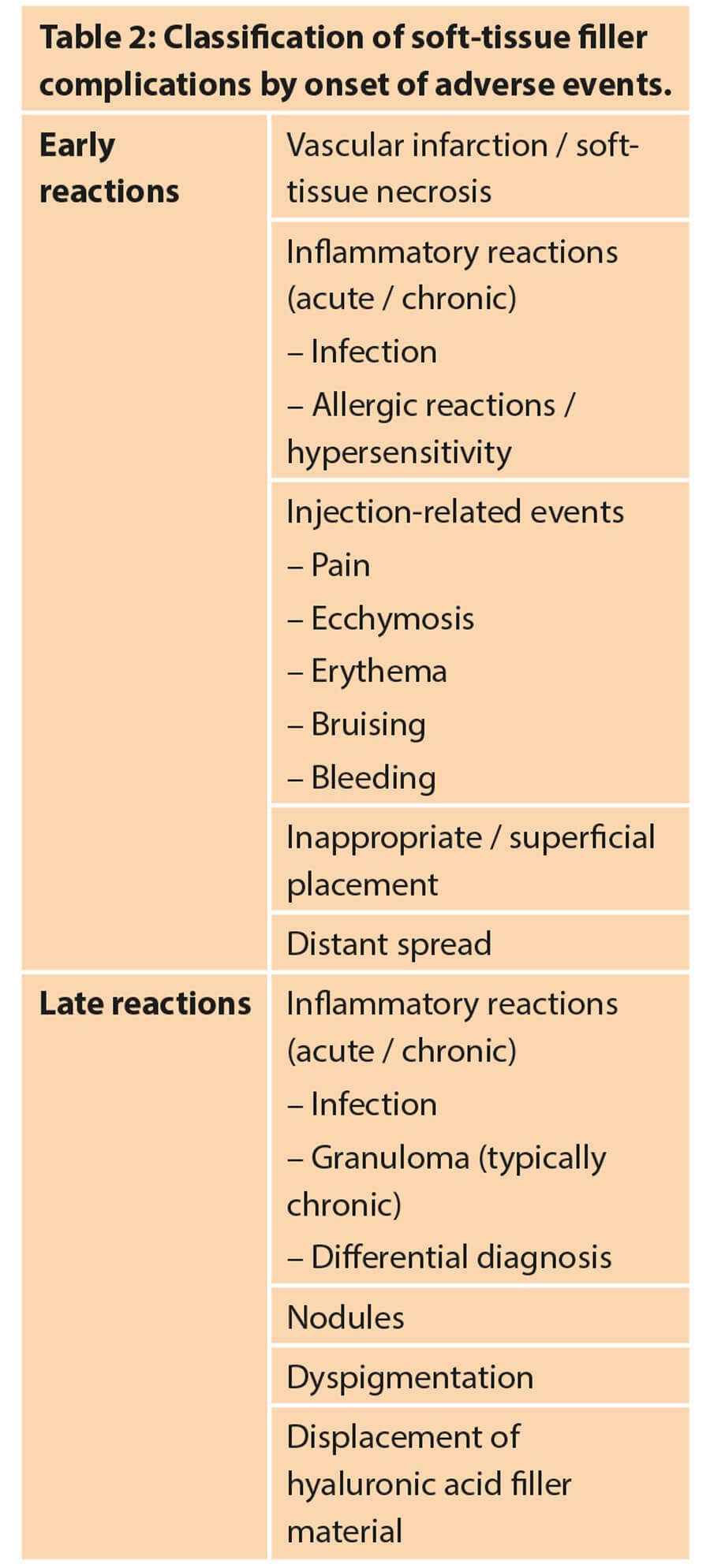
In 2016 Signorini et al. reviewed available evidence for the avoidance and management of complications from hyaluronic acid fillers, as well as expert opinions [16]. This was a global initiative to structure consensus recommendations for avoiding and treating these complications.
Importantly they distinguished complications into early and late reactions. These are seen in Table 2. This helps the practitioner be aware of which signs and symptoms to look out for during and immediately after the treatment.
Vascular infarction and compromise
Injecting hyaluronic acid (HA) filler into an artery or vein, or injecting enough HA filler around a vessel, can stop the flow of blood through the vessel and result in vascular compromise, with impending tissue necrosis, or even vision loss [17]. Vascular accidents are best minimised with knowledge of vascular anatomy, adequate training, and appropriate technique. Several sources in the literature describe strategies for diminishing this risk [18]. Precautions include aspiration before injection, slow injection with minimal pressure, and delivery of material at different points and in small volumes per pass [18]. Signorini et al. advocated, “keep the needle moving, and use small needles or blunt microcannulas” [16].
Signs and symptoms of a vascular injury and compromise can vary depending on whether it is an arterial or venous occlusion. Arterial occlusions tend to be evident immediately; they are severe, pain (when present) is disproportionate, and there is an acute onset of colour changes (blanching). Venous occlusion presentation can differ in that it can be less severe, with dull or delayed pain (sometimes no pain), delayed skin colour changes (red / bluish discolouration). Later stages of both includes blisters, pustules and tissue necrosis. There are several recommendations and publications on the treatment of vascular occlusion. Perhaps one of the one most cited is De Lorenzi’s recommendation of a high dose pulsed hyaluronidase protocol [19].
Allergic / hypersensitivity reaction
A reaction can occur due to the filler or agent used in the gel production [20]. Type I reactions are early onset (minutes to hours), while Type IV reactions are one to three days (up to weeks post treatment). Signs and symptoms include oedema, erythema, pruritis, pain or tenderness, and / or a rash [7]. All practitioners must have adrenaline readily available in their treatment room and know how to recognise and treat anaphylaxis.
Infection
Infections can be acute or delayed onset [16]. Acute infections tend to be secondary to common skin pathogens, inflammation or abscess. Delayed onset infections tend to present two or more weeks post treatment, span a more generalised area and may involve an atypical organism (mycobacteria or e-coli). They have been associated with biofilms. These tend to be treated with empiric antibiotics in the first instance. Microscopy, culture and sensitivities should be obtained if possible. Incision and drainage are sometimes required.
Nodule formation and granulomatous reactions
Nodules can be classed as inflammatory or non-inflammatory. They can be related or unrelated to an infection. A nodule is defined as a small collection of tissue that is palpable at any level of the skin (in the epidermis, dermis or subcutis) or in another tissue of the body, >0.5cm.
Early onset nodules, usually occurring within four weeks of treatment, are typically painless and non-inflammatory. They are likely a result of suboptimal techniques, such as excess filler placement, incorrect product for the indication or superficial placement.
In contrast, delayed onset nodules typically occur after four weeks. They are likely to be inflammatory, and / or infection-related and may constitute persistent non-inflammatory nodules. Sclafani and Fagien advise incision and drainage and antibiotic treatment of fluctuant nodules [21], and empiric antibiotic therapy followed by re-evaluation for non-fluctuant nodules; if there is no improvement, biopsy and culture are indicated.
A granuloma is a mass of granulation tissue typically produced in response to infection, inflammation, or the presence of a foreign substance [16]. It is a histological diagnosis. Granulomas may present months or even years after treatment. They tend to be adherent to tissue above and therefore carry a risk of erosion. Granulomatous reactions to hyaluronic acid fillers can be treated with hyaluronidase. Empiric antibiotic therapy should be considered. Granulomas may respond to oral or intra-lesional steroids after infection is ruled out or quiescent [16].
Conclusion
In summary, we must accept and expect that we will be involved in a complication at some point. We must discuss the risk of these with patients prior to any treatment, as well as advise on what measures we would take to treat / correct them.
To minimise the incidence of complications there are measures we can take before, during and after treating a patient. A meticulous history and examination will identify cautions and / or contraindications to treatment. An extensive knowledge of anatomy and of the products we are using, will help us avoid danger areas, guide our product choice, injection technique and placement of product.
Lastly, identifying when a complication has occurred will allow us to act promptly and treat accordingly to decrease morbidity.
References
1. Shiel Jr. WC. Medical Definition of Complication.
https://www.medicinenet.com/script/
main/art.asp?articlekey=25405
[Accessed 30 June 2020].
2. Gawande AN. Complications: A Surgeon’s Notes on an Imperfect Science. Profile Books Ltd; 2008.
3. GMC. Openness and honesty when things go wrong: The professional duty of candour. 2015.
www.gmc-uk.org/ethical-guidance/
ethical-guidance-for-doctors/candour-
--openness-and-honesty-when-things-go-wrong
[Accessed 30 June 2020].
4. Requena L, Requena C, Christensen L, et al. Adverse reactions to injectable soft tissue fillers. J Am Acad Dermatol 2010;64:1-34.
5. DeBoulle K. Management of complications after implantation of fillers. J Cosmet Dermatol 2004;3:2-15.
6. Regulation (EU) 2017/745 of the European Parliament and of the council of 5 April 2017 on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC.
https://eur-lex.europa.eu/legal
-content/EN/TXT/PDF/?uri=
CELEX:32017R0745
[Accessed 30 June 2020].
7. De Boulle K, Heydenrych I. Patient factors influencing dermal filler complications: prevention, assessment, and treatment. Clin Cosmet Investig Dermatol 2015;8:205-14.
8.Demosthenous N. Consultation skills: a personal reflection on history-taking and assessment in aesthetics. Journal of Aesthetic Nursing 2017;6(9).
9. Vedamurthy M, Vedamurthy A, Nischal KC. Dermal fillers: do’s and don’t’s. J Cutan Aesthet Surg 2010;3:11-5.
10. Jafferany M, Salimi S, Mkhoyan R, et al. Psychological aspects of aesthetic and cosmetic surgery: clinical and therapeutic implications. Dermatol Ther 2020;e13727.
11. Narins RS, Coleman WP, Glogau RG. Recommendations and treatment options for nodules and other filler complications. Dermatol Surg 2009;35:1667-71.
12. Funt D, Pavicic T. Dermal fillers in aesthetics: an overview of adverse events and treatment approaches. Clin Cosmet Invest Dermatol 2013;6:295-316.
13.Gold M, Andriessen A, Bhatia AC, et al. Topical stabilized hypochlorous acid: the future gold standard for wound care and scar management in dermatologic and plastic surgery procedures. J Cosmet Dermatol 2020;19(2):270‑7.
14. Bailey SH, Cohen JL, Kenkel JM. Etiology, prevention and treatment of dermal filler complications. Aesthetic Surg J 2011;31:110-21.
15. Glogau RG, Kane MA. Effect of injection techniques on the rate of local adverse events in patients implanted with non-animal hyaluronic acid gel fillers. Dermatol Surg 2008;34:S105-S109.
16. Signorini M, Liew S, Sundaram H, et al; Global Aesthetics Consensus Group. Global Aesthetics Consensus: avoidance and management of complications from hyaluronic acid fillers – evidence and opinion-based review and consensus recommendations. Plast Reconstr Surg 2016;137(6):961e-71e.
17. Lowe NJ, Maxwell CA, Patnaik R. Adverse reactions to dermal fillers: review. Dermatol Surg 2005;31:1616-25.
18. Lazzeri D, Agostini T, Figus M, et al. Blindness following cosmetic injections of the face. Plast Reconstr Surg 2012;129:995-1012.
19. DeLorenzi C. New high dose pulsed hyaluronidase protocol for hyaluronic acid filler vascular adverse events. Aesthet Surg J 2017;37(7):814-25.
20. Bailey SH, Cohen JL, Kenkel JM. Etiology, prevention and treatment of dermal filler complications. Aesthetic Surg J 2011;31:110-21.
21. Sclafani AP, Fagien S. Treatment of injectable soft tissue filler complications. Dermatol Surg 2009;35(Suppl 2):1672-80.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME









