A survivor of large full thickness skin burns will have suffered for months during repeated grafting surgeries to heal, yet real recovery will take years, if at all, because of the inevitable physical and mental challenges. Time spent on the burns unit will be repeatedly traumatic, painful and medically challenging with repeated bouts of sepsis and intensive care.
With advances in anaesthetic and surgical care, large burns can be effectively excised soon after admission and before sepsis intervenes, but autologous skin cover must thereafter be provided in a timely fashion. In major burn injuries where donor sites will be at a premium, fresh allograft will provide the same level of protection as autograft until it is replaced or inevitably rejects, although immune suppression to prolong the survival time may be possible using cyclosporin [1]. Xenograft, allograft or BiobraneTM are commonly used to achieve temporary cover, but they can also be applied over autologous micrografts or widely meshed autograft to achieve one-stage healing [2].
IntegraTM is an expensive bilaminate skin equivalent with a bio-integrating C-GAG layer covered by an adherent layer of silicone sheet that can be easily separated. It has proven invaluable in the management of serious burn injury and reconstructive surgery. When considered overall it is cost-effective in healthcare management terms when the costs of keeping victims alive in an intensive care environment can be reduced if earlier healing and functionality is achieved.
IntegraTM requires a second-stage procedure to remove the silicone cover and resurface the neo-dermis with an autologous skin graft, usually between the second and fourth weeks after application. IntegraTM should therefore be applied at least two weeks prior to when donor sites are expected to be available. In large burns IntegraTM can be prioritised early in the surgical plan for use over flexor creases or other anatomically important areas such as the face.
Sheet grafts are generally used at the second stage for quality outcome though. In other areas, such as the scalp, sheet grafting can be avoided by micrografting hair follicles that contain their pilosebaceous glands [3]. Early scalp healing and a degree of hair restoration becomes possible if enough hair follicles are transplanted.
Method
Single or multiple follicle grafts can be harvested from any unburned hair bearing area, with the scalp being the obvious first choice in many. Follicle grafts can be easily inserted using magnification and jeweller’s forceps through large bore needle punctures sited approximately 1cm apart, into the silicone layer of the C-GAG. The penetration is likely to go beyond the depth of the C-GAG layer. The shortened hair shafts of each graft act as a support for the follicle by impacting on the silicone layer (Figure 1).

Figure 1: Immediate excision of burn eschar and coverage with IntegraTM and micrografted hair follicles. The silicone layer is being carefully removed to reveal a newly epithelialised wound with hair at day 28.
Surrounding each hair follicle is a cuff of intact auto skin from which the epidermal cells proliferate. The follicle grafts are protected from shearing forces or haematoma by applying a good foam support dressing. Instead of requiring a second stage split skin graft, the silicone layer can be gently removed, as it naturally separates at three to four weeks, to reveal surface epithelialisation between the CGAG infiltrated neo-dermis and the silicone layer (Figures 2, 3a & 3b).

Figure 2: Second patient showing one op healing using IntegraTM and micrografted hair follicles. A secured, non-adherent, mouldable support sponge dressing was applied over the follicle grafts. Removal of the foam dressing and silicone layer reveals good integration of the CGAG layer and almost complete surface re-epithelialisation.
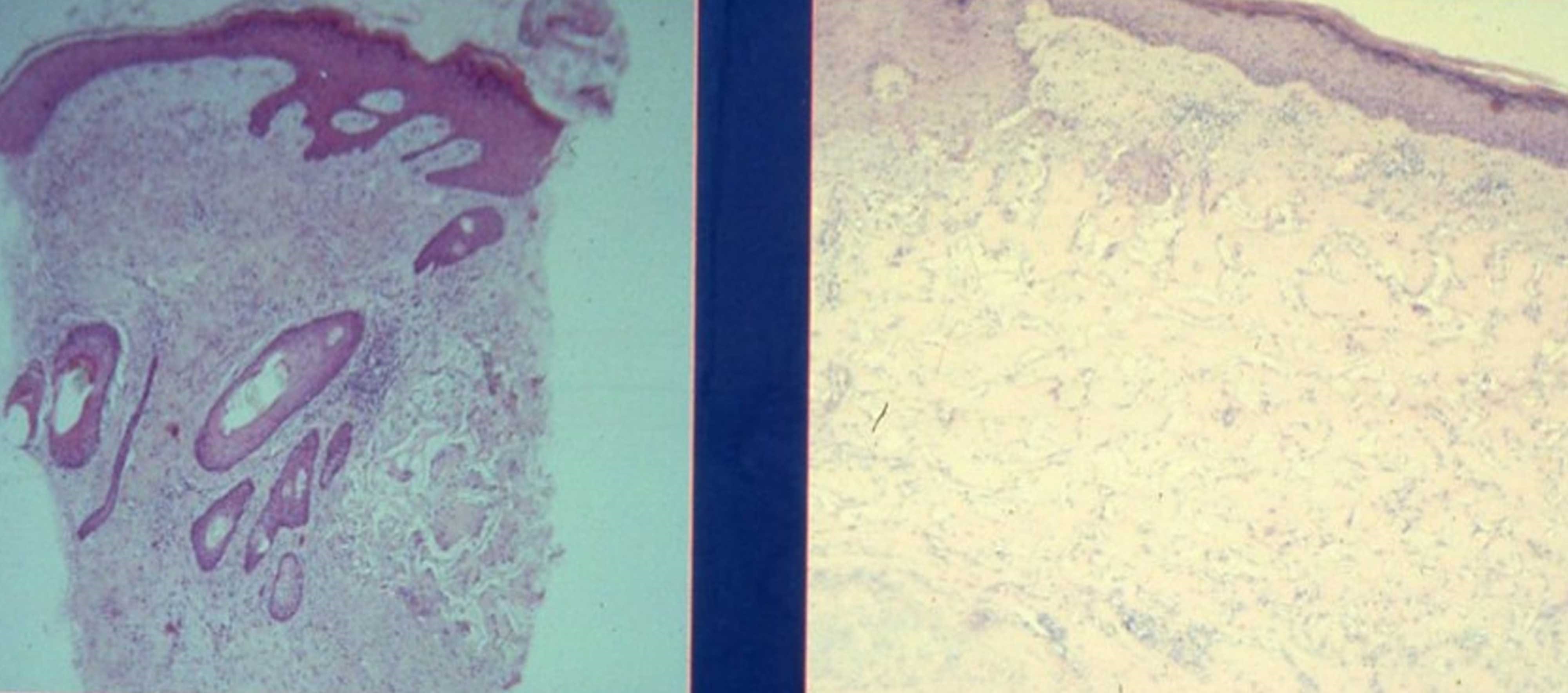
Figure 3a (left): Haematoxylin and eosin stain showing the survival of transplanted hair follicle with adjacent rete folds around the integrated hair follicle.
Figure 3b (right): Histology of the neo epidermis with flattish rete pegs and a revascularised neo-dermis full of collagen and fibroblasts.
This technique was first described in a case report in 2004 [3] and following other preliminary studies [4,5]. In addition, allografted hair follicles may transfer immunoprivileged epidermal stem cells that are normally sited within the follicular outer sheath zone known as the bulge [6,7].
Conclusion
Surprisingly, there are few in-vivo studies that investigate this use of hair follicles to regenerate skin in burn injury, but the use of autologous follicles could be considered in suitable burn patients because it supports the principle of early eschar excision and coverage for burn victims. Other advantages include:
- It can save the patient the painful experience of split skin graft harvest.
- It can be used when donor skin graft sites are at a premium in major burn injuries.
- It preserves donor sites.
- It saves in the number of surgical procedures.
- It achieves faster wound coverage.
- It reduces total cost to the healthcare provider.
References
1. Frame JD, Sanders R, Goodacre TEE, Morgan BDG. The fate of meshed allograft skin in burned patients using cyclosporin immunosuppression. Br J Plast Surg 1989;42(1):27–34.
2. Wang NZ, Reynolds PS, Coumbe A, Frame JD. Microskin grafting with Biobrane: a new application. Eur J Plast Surg 1995;18:157–61.
3. Navsaria HA, Ojeh NO, Moiemen N, et al. Reepithelialization of a full-thickness burn from stem cells of hair follicles micrografted into a tissue-engineered dermal template (Integra). Plast Reconstr Surg 2004;113(3):978–81.
4. Moiemen NS, Staiano JJ, Ojeh NO, et al. Reconstructive surgery with a dermal regeneration template: clinical and histologic study. Plast Reconstr Surg 2001;108(1):93–103.
5. Ojeh NO, Frame JD, Navsaria HA. In vitro characterization of an artificial dermal scaffold. Tissue Eng 2001;7(4):457–72.
6. Adler S, Neuman Z. Persistence of active donor follicles after skin allograft rejection by hamsters. Br J Plast Surg 1970;23(4):326–8.
7. Meyer KC, Klatte JE, Vu Dinh H, et al. Evidence that the bulge region is a site of relative immune privilege in human hair follicles. Brit J Dermatol 2008;9(5):1077–85.
Declaration of competing interests: None declared.











