Cavernous haemangiomas are rare, often distressing, and visually conspicuous vascular abnormalities caused by a mass of aberrant tangles of thin walled, easily distended blood vessels.
Fourteen percent will present in the head and neck regions and are histologically characterised by pericyte endothelial hyperplasia. Cavernous haemangiomas typically appear and grow in the first year of life, followed by a period of sustained proliferation, which may eventually stabilise or regress over time.
Case report
A 52-year-old healthy woman was socially embarrassed and upset by an extensive, bulging cavernous haemangioma originating from deep within the temporalis muscle on the left side of her face. When coughing and lying flat the haemangioma filled with blood to create a visible and non-pulsatile bulge that appeared to be more obvious as she was ageing. Up until her presentation she had been able to successfully disguise the blue surface discolouration with stage make-up but could no longer hide the bulge. The case presented as an aesthetic challenge because she was not keen to undertake the risks associated with the traditional options on management.
Management options
A conservative approach incorporating a ‘wait and see’ policy was not an option to the patient because of the presenting psychological impact. The option of a non-surgical approach using corticosteroid injections and sclerosants was also deemed non-sensical because of high-risk, low-reward outcomes with thinning of tissues, weakening of ligaments, discolouration of skin, prominent telangiectasia and without a significant reduction of patient concerns. Radiotherapy as an option carried significant risk and was unlikely to be successful. Surgical excision of the haemangioma was a potential cure but had a perceived high risk of damage to motor nerves with potential for permanent ipsilateral forehead paralysis and brow ptosis. The patient subsequently elected to try and reduce the bulging nature of the pathology using layered IntegraTM.
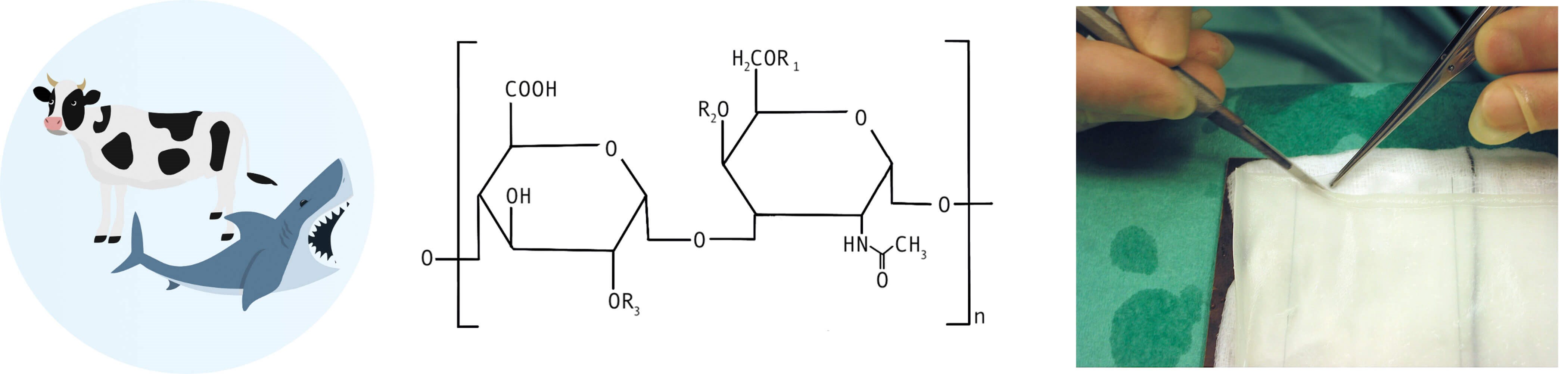
Figure 1: Illustration of the key components of IntegraTM, including bovine [4] and shark collagen [5], Chondroitin-6-Sulfate molecule representing the GAG matrix, and the removable silicone membrane layer.
What is IntegraTM ?
IntegraTM is a dermal regeneration template that was originally developed in the 1980s to act as a scaffold for autologous fibroblast and vascular endothelial cell infiltration and to restore and resurface skin after burn injury (Figure 1) [1]. It has since been used to help heal open wounds, in release of contractures and even as a filler to correct soft tissue contour defects [2].

Figure 2: Patient presenting with a blue, bulging haemangioma in left cheek and temple area. Frontal and lateral view (left picture and right picture).
Rationale for using IntegraTM minus the outer silicone layer
Facelifts have been used to improve the appearance in patients with capillary haemangioma [3]. In this case (Figure 2, left), a preauricular left facelift flap was raised to just beyond the bulging haemangioma that was clearly delineated in a slightly Trendelenburg position on the operating table (Figure 2, right). The flap was extended into the temporal region. The slack superficial musculo-aponeurotic system (SMAS) layer below the zygoma was plicated with non-absorbable sutures.

Figure 3: Integra™ about to be inserted over the plicated SMAS layer.
The silicone layer from a single sheet of IntegraTM was removed and the remaining matrix was tailored and sutured in a double layer to overfit the pre-marked borders of the bulging haemangioma on her left cheek, with care taken to avoid the frontal branch of the facial nerve (Figure 3). The flaps were then returned without a skin tightening procedure. The IntegraTM was expected to biointegrate and in the process, leave a sturdy fibro-collagenous matrix functioning as a restraining fascial layer.

Figure 4: Postoperative, same patient, frontal and side view after plicating SMAS and overlaying a double layer of IntegraTM to reinforce and prevent the bulging. There is a significant and pleasing reduction in bulging and more symmetry in volume (left picture and right picture).
The neo-layer served to contain the haemangioma within its confined space related to the temporalis and the temporal fossa and gave a satisfactory result (Figure 4). There was a degree of blue skin discolouration, but this was easily masked with make-up.
References
1. Moiemen NS, Vlachou E, Staiano JJ, et al. Reconstructive surgery with Integra dermal regeneration template: histologic study, clinical evaluation, and current practice. Plast Reconstr Surg 2006;117(7 Suppl):160S–74S.
2. Frame JD, Frame JE. Modifying integra as a regeneration template in deep tissue planes. J Plast Reconstr Aesthet Surg 2006;59:460–4.
3. Khan JI, Frame JD. Facelift surgery: An adjunct in the treatment of capillary malformations (port wine stains). Aesth Plast Surg 1994;18:201–3.
4. Photo: © Anthony Fever, ‘Cow’s Milk Illustration’ via www.Canva.com, accessed 17 June 2025.
5. Photo: © Good Choice, ‘Shark’, www.Canva.com accessed 17 June 2025.
Declaration of competing interests: None declared.








