In the first of a two-part series, Andrew Burd takes us through the background to the development of his protocol for the acute management of chemical assault burns (see Part 2 here).
I have maintained a long-term interest in how chemicals interact with living tissues, in particular with regard to crimes of assault. Clinical observation has a very important role in how we should treat such patients. The reason is that, although such patients should hopefully be rare for individual doctors, this does complicate the process of having an evidence-based treatment plan.
Randomised, controlled, clinical trials have no place in determining the acute clinical care of chemical assault cases. Before I introduce my current protocol for the acute management of chemical assault burns I want to fill in some of the background to my work in this field. This is an emotive topic and has been used and abused by politicians, journalists, commentators and celebrity-seeking surgeons to further their own agendas. That is not good.
From extravasation to assault
During the Chinese 9th National Congress of Plastic Surgery held at Changsha, Hunan Province in 2007, the reality of facial transplantation was a topic of great interest. In an editorial written to celebrate this event I described briefly the first patient I had seen who had lost their face. This was a tragic accident but the causation was a chemical, in this case alkali, burn [1]. This early experience as a junior doctor led to a lifelong interest in the interaction between chemicals and human tissues. One devastating example of this is the extravasation injury where an accidental leakage of a fluid substance intended for intravascular administration can cause extensive destruction. I reported on such a case many years ago [2] and it is interesting how one clinical experience and observation leads to another. Having expressed an interest in extravasation injuries I was soon referred more cases and a notable one was a case of extravasation of 10% calcium gluconate in a renal transplant patient [3].
“New strategies can be further encouraged, in particular urgent excision of HF burns specifically but also with acid assault burns in general, to decrease the acid load”
Hydrofluoric acid burns
The hyperosmolar calcium gluconate had caused a full thickness ‘burn’ injury of the medial ankle and required debridement and skin grafting. Not long after I was called to the accident and emergency department to see a patient who had sustained hydrofluoric acid (HF) burns to his right thumb and index finger. He had been in considerable pain and the emergency doctor had given what was then standard treatment, subcutaneous calcium gluconate. Aware that this could cause a devasting iatrogenic disaster my primary concern was to reduce the hyperosmolar effect by using hyaluronidase. I then proceeded to read around the treatment of hydrofluoric acid burns.
The result was an extensive review of the evolution of treatment of HF burns. By extensive I mean that we undertook to identify every paper written in the English language that discussed hydrofluoric acid burns. This was also undertaken at a stage when we were becoming increasingly interested in medical algorithms in preparation for the day when artificial intelligence (AI) would be a driving force in clinical medicine. The result was two papers, one a review and one an algorithm [4,5]. This foundation of knowledge created a desire to build on it with new insights in the evolving literature. This resulted in various personal communications with authors from a number of disciplines and also resulted in a number of letters to journals which stimulated open, professional discussion.
There was one paper though that did cause considerable concern. The paper was simply titled ‘Hydrofluoric Acid Burns’. It came from the Brisbane unit in Australia and the senior author was one of the grandees of the international burn community [6]. This paper described a series of hydrofluoric acid burns admitted to a single unit between 1977 and 1999. On the basis of this clinical experience the authors developed a series of clinical algorithms that were remarkably similar to the ones we had previously developed 10 years before. One of the stated objectives of the paper was to present “a novel way of delivering calcium combined with dimethyl sulphoxide (DMSO) for cutaneous burns”.
It was notable that this paper did not include any reference to either our detailed review of the literature or the algorithms which we had developed based on that literature. This was unfortunate as the “novel” treatment was not novel and had been discredited for reasons we detailed in our review. Whilst revisiting historical precedent and contributing to the advancement of medical knowledge it is important to be focused on the entirety of the available evidence. Following a series of private communications with the editor of the journal the following commentary and case report was published, ‘Hydrofluoric acid – revisited’ [7]. This was my first experience of quietly and patiently going through a published, i.e. peer reviewed, paper and systematically exposing its flaws and inaccuracies.
Hatzifotis’s paper repeated some common fallacies. They declared that the incidence of HF burns is low. This is a statement with no meaning without further clarification. The incidence of severe HF burns is mercifully low but, because of its widespread use in multiple industries, HF acid burns are not uncommon. In occupational medicine journals there are many series of hundreds of patients who sustain burns treated with water alone or more contemporaneously with calcium gluconate gel. The next comment related to the common misconception repeated by Hazifotis et al. that “HF is one of the strongest inorganic acids”. This is simply not true. What followed in the commentary was a detailed explanation of the nature of acids and their tissue interactions compared to the action of HF. In particular HF readily crossed lipid membranes.
Evolution of treatment is more often driven by experience that traditional strategies do not work rather than evidence that new ones are better.
Having penetrated into the skin the molecule disassociates into hydrogen and fluoride ions. The fluoride ion is responsible for liquefaction necrosis in the tissues but of far greater significance is the affinity of the fluoride ion for calcium ions producing calcium fluoride. It is this chelation of calcium from the systemic circulation that causes the cardiac arrythmias and death associated with hypocalcaemia. In the severe HF burn lifesaving first aid requires urgent replacement of calcium. Methods and strategies had been reviewed in our 1995 papers. Ten years later when Hazifotis et al. wrote their paper they also described a “novel” technique. The problem was that it had in fact been discredited due to the number of adverse effects reported with DMSO. This was unfortunate but was matched by a very questionable intellectual claim that experience with 42 patients had enabled the authors to “create” a number of algorithms which were remarkably similar to those we had previously published. In addition, it is difficult to relate the algorithms, for example, to HF ingestion when no such burns were described in the series. It is always of concern when papers appear in the scientific literature which raise both factual concern regarding proposals for treatment but also ethical concerns. Politics should make no difference to a scientific publication, but on occasions they do.
I took the opportunity of this commentary to describe the first reported case of murder by hydrofluoric acid in the UK. It occurred whilst I was senior trainee in Manchester. The patient had been treated as an acid assault victim with the assumption that the active agent was sulphuric acid.
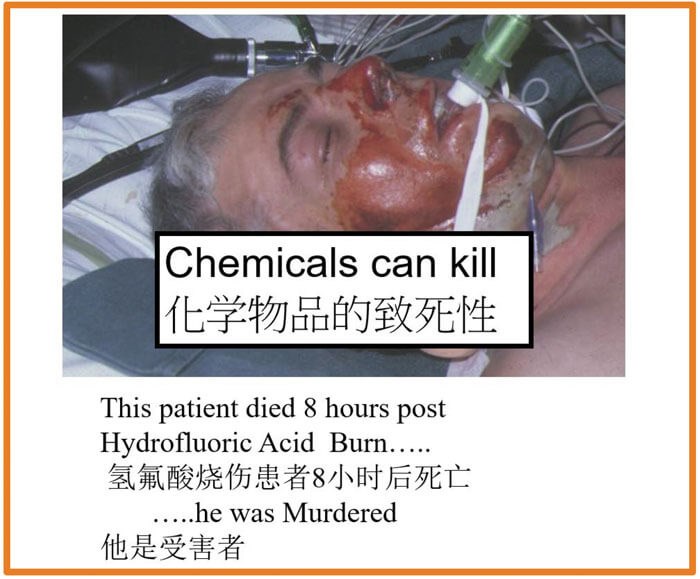
The clinical appearance of HF burns from concentrated solutions is a greyish discolouration of the skin. I happened to see the patient being wheeled into the burns unit but had him re-directed to the intensive care unit. Valuable hours had already been lost and despite a rapid infusion of intravenous calcium the patient died eight hours after the assault.
This was a 4-5% body surface area (BSA) burn. The point that I am raising here is that publication of experience is important but so is a thorough, and honest, review of the literature.
Whilst our original review does not conform to the relatively narrow definitions of graded evidence-based guidelines the review, and its accompanying algorithm published simultaneously in 1995, represents the closest to level two evidence with grade C recommendations to this day. What I can say quite confidently is that if I came across that patient today I would have no hesitation in redirecting them, not to the intensive care, but to the operating theatre. By 2004, when this commentary was published I was already beginning to engage in urgent excision of acid burns. There is no level four evidence to support such a strategy, but this illustrates a continuing dilemma in burns care. I put in print my oft repeated remark when teaching:
The editor of the Burns journal was at that time Peter Shakespeare. He was in a difficult position regarding both the authorship and also that the paper had been through the peer review process. In the current era of more rigorous oversight of possible lapses in ethical conduct in the publishing process one could make a case for retraction. This is now more widely regarded as a responsible thing to do and does not negatively impact on the reputation of the journal or the editor.
Retraction does have problems for publishers and indexers and there are also legal considerations. Retraction with the authors’ consent is a very different matter from retraction associated with serious allegation of misconduct against any authors. In my words at the time: “The paper from Hazifotis et al. was sloppy. It was poorly researched, made unsubstantiated claims of a novel treatment and presented algorithms not substantiated by the evidence provided”. Peter Shakespeare published my commentary on the paper in full without any changes. I am grateful for his comments on the commentary and quote from them here: “The journal will always accept comments on published material that enhances its value. I urge all readers to read both Professor Burd’s original and Dr Hatzifotis’ reviews together with this paper. In an area so difficult and uncertain as the diagnosis and treatment of burns caused by hydrofluoric acid a continual process of review is probably necessary. I am grateful to both sets of authors for their work in keeping this important subject in the public eye”.
As indicated above the incidence of serious HF burns is thankfully low but they do occur and appear in the literature as case reports. Commentary on these can emphasise part of the evidence base and new strategies can be further encouraged, in particular urgent excision of HF burns specifically but also with acid assault burns in general, to decrease the acid load [3,8].
Assault by nitric acid
The next devastating case of an acid assault burn occurred in England in 1996 or shortly thereabouts. The reason I can be so certain about this is because of the way the patient, a young woman, was treated. For Beverley, it was a tragic case of mistaken identity. She was babysitting for a lady who was going through a very acrimonious divorce. In an act of evil treachery, the husband paid a man in a pub to take “this yellow liquid” up to a house, knock on the door and when a woman answers, throw it in her face and scarper; all for a couple of hundred quid. The yellow liquid was industrial strength nitric acid which contained a dye to prevent reselling. Media accounts of the attack can be found at:
http://news.bbc.co.uk/2/hi/uk_news/63861.stm
https://www.independent.co.uk/news/twelve-years-for-jealous-husband-in-acid-attack-1149353.html https://www.theguardian.com/theobserver/2003/aug/03/features.magazine97
I include one quote from Beverley that featured in the last article: “I remember feeling even before this happened that negative emotions are a waste of time, and I’ve never believed in holding grudges. But what’s really helped is that I’ve never thought looks are that important anyway.”
Beverley is a truly amazing woman who has tremendous support but also a profoundly simple philosophy of life that has enabled her to survive and overcome challenges that would have been unsurmountable for so many.
Beverley was just in the wrong place at the wrong time and as a result her face had to be cut off and replaced with a tissue engineered material, Integra, which was first brought into the UK in May of 1996. The illustrations of the case can be found buried in a chapter entitled ‘Burns: Treatment and Outcomes’ [9]. This was a contribution to a monograph edited by Samir Mardini, Christopher Selgaldo and Hung-Chi Chen called ‘Advances in Head and Neck Reconstruction, Part II” and was published in the journal, Seminars in Plastic Surgery. The chapter / paper was 19 pages long with multiple illustrations and gave a good platform to share experience. The illustrations were unfortunately in black and white. The format of the chapter tells a story. It begins by focusing on the prevention of burns and progresses to first aid and acute management.
The acute management of a severe burn is a team effort involving medical and surgical inputs. Of note a burn injury is a systemic injury which can have profound effects on all organ function. The principle goal in the acute phase is survival. This has to be put very carefully in the context of quality of survival. Survival per se is a matter of restoring a chemical balance to cellular activity in the various organs and tissues. Chemical balance is a far more complicated challenge than restoring physiological levels of chemicals with exogenous therapy. It involves restoring the multi-functional aspects of cellular control including hormones, cytokines and extracellular matrix composition. As stability is returned to the core life functions, attention can be paid to the longer term sequalae and focus on the quality of survival. This is essentially a matter of limiting the actual and potential scarring. Of interest to the evolving discussion was that chemical burns of the head and neck were specifically mentioned.
A key dilemma is how to prevent the ongoing process of damage occurring at the interface of the penetrating chemical and the viable tissue. The traditional and still widely practised method was to try and reduce the concentration of the chemical by lavage with water. This is not a clinical situation where best practice can be determined by randomised controlled clinical trials. What is needed is the honesty to accept that results with conventional treatment are not optimal, then look at the underlying pathophysiology and come up with a rational departure from the traditional management pathway. The most important principle to follow is the fundamental ethical principle of medical practice: primum non nocere (first, to do no harm).
I shall finish this part one with just a short observation. We live in a world where almost everyone can be an expert (courtesy of Google). But Google is susceptible to the uncritical comments of the misinformed. Take for example this website which relates to Beverley: https://worldwidefeatures.com/feature_info.php?feature_id=438
“The acute management of a severe burn is a team effort involving medical and surgical inputs”
The “amazing” operation Beverley had was the use of a tissue engineered dermal regeneration template in the acute phase. I do not consider tissue expansion 10 years later to be anything other than standard procedure. It is very important to remain objective, particularly when speaking with the media. Too often they get things wrong in the process of trying to hype up their ‘piece’. We must guard against this ‘misinformation’.
References
1. Burd A. Face. Journal of Plastic, Reconstructive and Aesthetic Surgery 2007;60:1173-4.
2. Burd DA. Santis G, Milward TM. Severe extravasation injury: An avoidable iatrogenic disaster?’ British Medical Journal (Clinical research ed.) 1985;290(6481):1579.
3. Burd A. Hydrofluoric acid burns: rational treatment. Journal of Burn Care and Research 2009;30(5):908.
4. Kirkpatrick JJR, Enion DS, Burd DAR. Hydrofluoric acid burns: a review. Burns 1995;21(7):483-93.
5. Kirkpatrick JJR, Burd DAR. An algorithmic approach to the treatment of hydrofluoric acid burns. Burns 1995;21(7):495-9.
6. Hatzifotis M, Williams A, Muller M, Pegg S. Hydrofluoric acid burns. Burns 2004;30(2):156-9.
7. Burd A. Hydrofluoric acid – revisited. Burns 2004;30(7):7202.
8. Burd A. Hydrofluoric Acid Burns of Head and Neck. Journal of Burn Care & Rehabilitation 2005;26(3):291.
9. Burd A. Burns: Treatment and Outcomes. Seminars in Plastic Surgery 2010;24(03):262-80.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME









