
During the first wave of the COVID-19 pandemic, guidance advised postponement of elective procedures except for time-critical local anaesthetic (LA) procedures [1-3]; our NHS Trust therefore continued with LA skin malignancy surgery. All patients having possible skin cancer lesions removed during the start of the first UK lockdown, between 24 March and 9 June 2020, were included.
Operations took place in outpatient-based treatment rooms as ‘see and treat’ procedures to reduce the need for repeat hospital visits. Virtual clinics were used for initial video consultations and follow-ups. Three hundred and seventy-nine procedures were performed on 371 patients (mean age = 66.9 years).
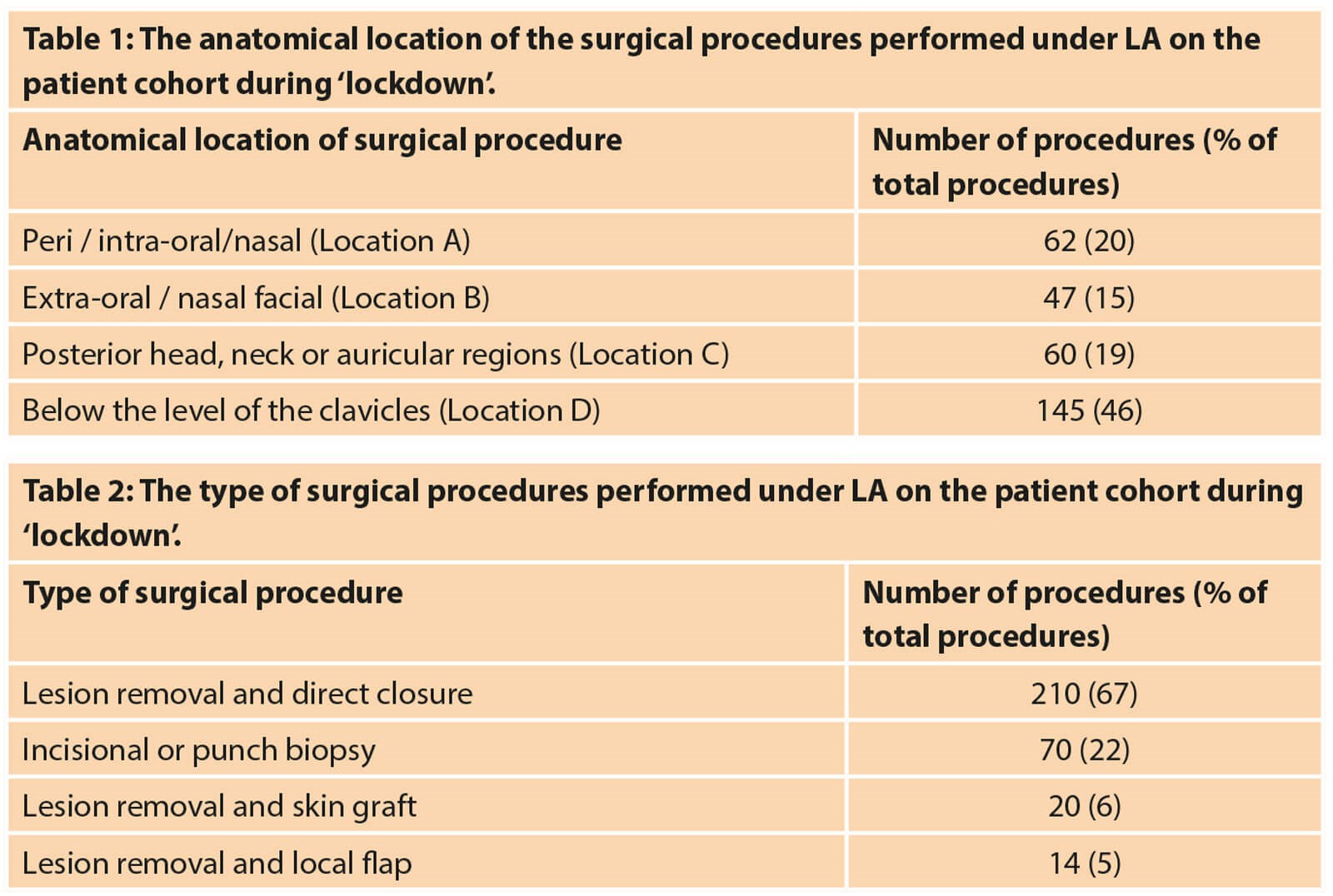
Three hundred and six patients (82%) completed the telephone questionnaire (Figure 1 and 2), at least two weeks after their treatment, providing data for 314 surgical procedures (Table 1 and 2).
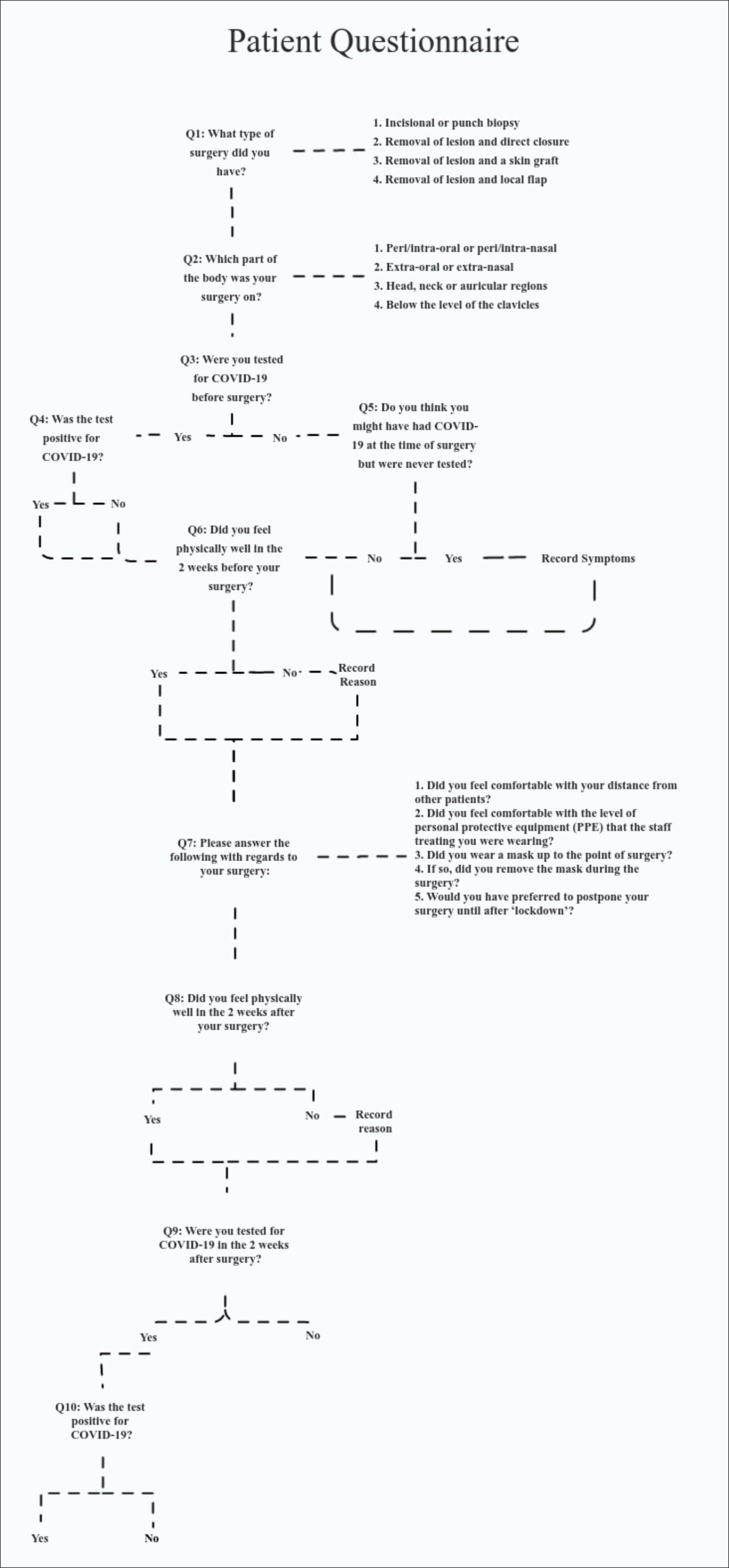
Figure 1: The flow chart of questions asked of each patient during the telephone questionnaire.
Procedures within or around mucosal surfaces are deemed to carry the highest risk of SARS-CoV-2 transmission to surgeons [2]. Twenty percent of procedures were in a peri / intra-oral / nasal location (Location A) requiring removal of patient masks.
These were treated as aerosol generating procedures (AGPs) and full surgical gowning was performed with FFP3 masks and visors. Diathermy was also considered an AGP. Surgical procedures on the extra-oral / nasal face (Location B) were deemed to carry a lower risk; patient masks were not removed where possible, and full PPE was worn. Across 314 procedures, 17% (N=52) of patients wore a mask intraoperatively. Now, we have all patients wearing masks, and only remove them if operating in the peri / intra-oral / nasal location.
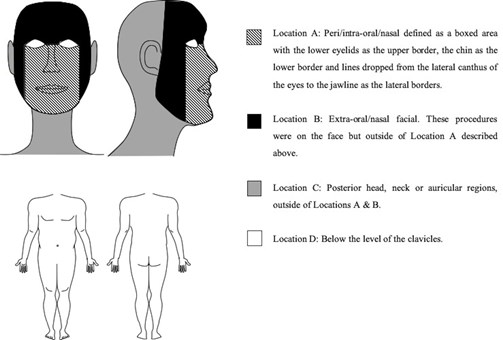
Figure 2: The four anatomical locations where patients had surgical procedures.
Infectious aerosols may remain in a room for up to three hours [4], however the air is changed in our treatment rooms every 15 minutes. Patients were therefore booked for a 45-minute slot followed by 15 minutes for cleaning the treatment room, during which time tele-consultations were scheduled. Patients were asked to arrive at their designated time to further enable appropriate distancing in the waiting areas. Most patients spent less than an hour within the hospital and felt that they were safely distanced throughout (N=294; 96%). The treatment rooms were in designated hospital ‘Green Zones’, reducing the likelihood of contact with a COVID-19 positive patient in the main hospital.
Patients were only screened for COVID-19 symptoms preoperatively. Nine patients had a negative COVID-19 antigen test preoperatively. Two patients believed they had COVID-19 in the two weeks before surgery but were not tested. Due to an administrative error, their surgery was not postponed. A small group (N=6; 1.96%) felt unwell before surgery due to pre-existing health problems. None of these patients went on to develop COVID-19 symptoms after surgery. Patients attending outpatient appointments are still only screened based on symptomatology alone, including those for LA ‘see and treat’ procedures.
In the two weeks following their surgical procedure(s), 10 patients (3%) reported feeling unwell; three due to pre-existing conditions, three had infections which resolved with antibiotics, one wound dehisced, and one patient was hospitalised for severe headaches, but tested negative for COVID-19. Two patients developed a cough in the two weeks following their procedure. One tested negative for COVID-19. The other patient was not tested but did not develop any other COVID-19 symptoms or more significant complications. Therefore, most patients (N=304; 99%) did not develop COVID-19 symptoms in the two weeks following surgery, suggesting that performing these dermatological procedures under LA did not increase the risk of SARS-CoV-2 transmission to patients. None of the healthcare workers (HCWs) tested positive for COVID-19 during the study.
“Our study suggests that neither patients nor healthcare workers in our Trust were infected with SARS-CoV-2 as a result of having an elective dermatological LA surgery procedure during the UK lockdown, when appropriate precautions are taken to mitigate the risks of infection”
No patient questioned in this study developed any severe or adverse COVID-19-related complication as a result of their surgery. Although, in the absence of tests, we cannot conclude that patients did not acquire SARS-CoV-2 during their hospital visit. Symptom screening of patients appears to be sufficient and safe for outpatient-based LA surgery. All but three patients (99%) said they did not want to postpone their surgical procedure during the lockdown due to anxiety from delaying a possible skin cancer diagnosis. None of the seven surgeons and 23 clinic nurses tested positive for COVID-19 on antibody testing at the end of the study despite two symptomatic patients inadvertently attending for procedures, and any number of possible asymptomatic patients. This demonstrates that appropriate use of PPE and the other precautions taken to mitigate risk (staggered appointments, cleaning breaks between patients, mask wearing) is effective in preventing SARS-CoV-2 transmission during minor outpatient procedures.
Of the 65 patients (18%) who did not answer the telephone questionnaire, all were recorded as being alive, had not required a postoperative COVID-19 test or been admitted with COVID-19 symptoms according to the Trust’s database. Twenty-three answered their phone and spoke without obvious respiratory symptoms but refused to participate. Sixteen phone numbers from the computer database were not recognised. One death occurred due to co-morbidities and was not related to COVID-19 or the patient’s procedure.
Although many guidelines in the UK suggest postponing elective surgical procedures during the pandemic, clinicians must balance the risks of a patient potentially contracting hospital-acquired COVID-19 with the risks of postponing surgery for diagnosis or treatment of potentially life-threatening conditions. Our study suggests that neither patients nor healthcare workers in our Trust were infected with SARS-CoV-2 as a result of having an elective dermatological LA surgery procedure during the UK lockdown, when appropriate precautions are taken to mitigate the risks of infection.
The approval of three vaccinations [5] and the subsequent vaccination of healthcare workers further enhances the safety of LA procedures during the COVID-19 pandemic. However, vigilance must be maintained due to the appearance of more infectious variants of SARS-CoV-2 [6] since our initial data collection. We must continue with safe outpatient-based LA dermatological surgery, as crucially, the COVID-19 pandemic must not exacerbate the skin cancer epidemic in the UK and across the globe.
TAKE HOME MESSAGE
-
No patient questioned in this study developed any severe or adverse COVID-19-related complication as a result of their LA skin malignancy surgery.
-
No healthcare worker in this study tested positive for COVID-19 on antibody testing at the end of the study despite two symptomatic patients inadvertently attending for procedures, and any number of possible asymptomatic patients.
-
Symptom screening of patients appears to be sufficient and safe for outpatient-based LA surgery.
-
Appropriate use of PPE and the other precautions taken to mitigate risk (staggered appointments, cleaning breaks between patients, mask wearing) is effective in preventing SARS-CoV-2 transmission during minor outpatient procedures.
-
We must continue with safe outpatient-based LA dermatological surgery, as crucially, the COVID-19 pandemic must not exacerbate the skin cancer epidemic in the UK and across the globe.
References
1. British Association of Plastic Reconstructive and Aesthetic Surgeons. Advice for managing Melanoma patients during Coronavirus pandemic.
www.bapras.org.uk/docs/default-source/
covid-19-docs/corona-virus---melanoma
---final-version-2.pdf?sfvrsn=2
[accessed 29 June 2021].
2. Ozturk CN, Kuruoglu D, Ozturk C, et al. Plastic surgery and the COVID-19 pandemic: a review of clinical guidelines. Annals of Plastic Surgery 2020; [Epub ahead of print].
3. Lima RME, de Andrade Reis L, Thyrso de Lara FS, et al. Recommendations for local-regional anesthesia during the COVID-19 pandemic. Brazilian Journal of Anesthesiology (English Edition) 2020;70(2):159-64.
4. van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med 2020;382(16):1564-7.
5. National Health Service England. Coronavirus (COVID-19) vaccine.
https://www.nhs.uk/conditions/
coronavirus-covid-19/coronavirus-vaccination/
coronavirus-vaccine/
[accessed 29 June 2021].
6. Kirby T. New variant of SARS-CoV-2 in UK causes surge of COVID-19. The Lancet Respiratory Medicine 2021;9(2):e20-e21.
Declaration of competing interests: None declared.
Acknowledgements: Henry MW Bestwick, Henry R Bennett BA, Anjuli A Banerjee, Cedric Banfield, Joseph Walls, Hagen HA Schumacher, Michael A Moses, Mary-Clare C Miller and Peter Goon.
COMMENTS ARE WELCOME












