This article will explore local anaesthesia (LA) and how its misuse can have severe negative consequences. We will also look into how we can address this important issue and help make the industry safer for patients.
In the last few years, we have seen a great surge in practitioners offering aesthetic treatments across the UK and the trend is set to continue – many of these treatments require a local anaesthetic.
As the aesthetics industry continues to boom, it is no coincidence that the global local anaesthesia drugs market is expected to grow significantly in the next few years [1].
Safe and effective use of local anaesthesia is crucial in aesthetic procedures, providing benefits such as pain reduction, improved recovery, patient satisfaction and reduced downtime. However, its misuse or abuse can result in serious and potentially life-threatening consequences.
The advent of local anaesthesia has revolutionised surgical practice, making prolonged, complex and painful procedures possible and transforming the patient experience. However, as with all pharmacological interventions, a detailed understanding of the drug being used is vital for safe practice.
Healthcare professionals receive significant training on the pharmacology and safe use of local anaesthetics and only progress to independent practice when supervised workplace training indicates they are safe to do so.
Unfortunately, the truth is many providers of aesthetic treatments are not qualified enough to consistently provide safe and adequate treatments to their patients. Aside from the low-quality courses people are undertaking, a working medical understanding is not something you build in a day, even weeks or months; it takes years.

How does local anaesthesia work?
The basic pharmacologic mechanism of all local anaesthetics entails interrupting axon depolarisation by preventing Na+ influx into the neuron. Simply put, LA works by diffusing into the cell and acting as a physical barrier to the sodium potassium (Na+, K+) pump, by stopping the flow of Na+ into the cell, thereby stopping the activation of the pump which is needed for a nerve impulse to be propagated [2]. This ultimately means the patient loses ‘feeling’ in the area.
Some of the most common local anaesthetics used in aesthetic treatments include:
- Lidocaine (Lignocaine): fast-acting local anaesthetic, widely used in a variety of aesthetic procedures, including injections, laser treatments, and minor surgeries.
- Bupivacaine (Marcaine): long-lasting local anaesthetic, often used in procedures that require a longer duration of numbness, such as tummy tucks and facelifts.
- Prilocaine: faster-acting anaesthetic, often used in combination with other anaesthetics because of its rapid diffusion to the target site.
- EMLA: A eutectic mixture of prilocaine and lignocaine for topical application.
Amethocaine: Another topical local anaesthetic cream.
Which local anaesthetic to choose?
When selecting a local anaesthetic for an aesthetic treatment, it is important for the practitioner to consider the following factors:
- The patient’s medical history: the practitioner should consider any underlying medical conditions that may affect the patient’s ability to tolerate a particular anaesthetic. For instance, patients with liver or kidney disease may have a decreased ability to metabolise and eliminate the local anaesthetic, leading to a faster onset of toxicity.
- The type of procedure being performed: different local anaesthetics may be more suitable for different procedures. For example, lidocaine may be preferred for injectable treatments, while bupivacaine may be preferred for longer-lasting surgical procedures.
- The duration of anaesthesia required: the practitioner should consider the length of the procedure and the amount of anaesthesia needed.
- The potential for adverse effects: the practitioner should consider the potential for allergic reactions, cardiovascular effects, and neurotoxicity, and be prepared to manage any adverse reactions that may occur.
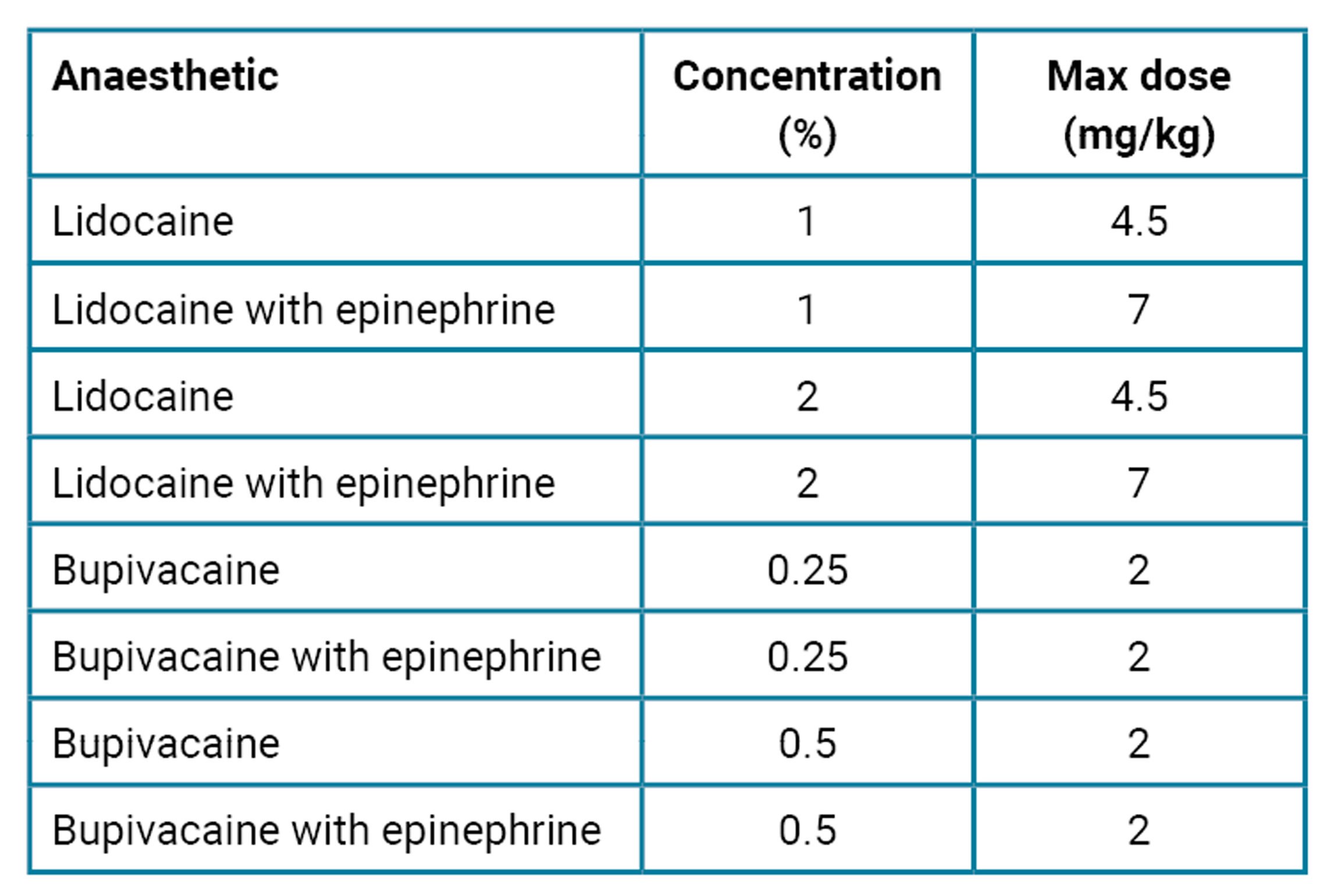
Table 1: Local anaesthesia maximum dosage reference guide.
With various routes and sites of administration and each one possessing its own maximum safe dose, local anaesthetics are associated with varying degrees of risks of toxicity and each specific drug has specific instructions (Table 1).
The safe dosage of lidocaine is 4mg / kg without epinephrine. So, for a 70kg adult, that is 280mg. This 10.56% solution contains 100mg / ml, therefore the toxic dose is 2.8mls. You can easily see how little of this solution is needed and how easily it could be mishandled.
The dangers of local anaesthetic systemic toxicity (LAST)
LAST is a life-threatening adverse reaction resulting from local anaesthetic reaching significant systemic circulating levels, which can result in a range of minor to more severe effects on the cardiac or central nervous system (CNS) (Figure 1).
With the continuous growth of aesthetic treatments all over the world, it is important that, whilst rare, we do not ignore the increasing possibility of LAST incidents. Common symptoms of LAST include [3]:
- Numbness or tingling around the mouth or in the limbs
- Metallic taste in the mouth
- Visual disturbances, such as blurred or double vision
- Tinnitus or ringing in the ears
- Dizziness or light-headedness
- Muscle twitching or convulsions
- Difficulty breathing or respiratory distress
- Changes in heart rate, such as bradycardia (slow heart rate) or tachycardia (rapid heart rate)
- Hypotension (low blood pressure).
The toxic effects of LAST can occur rapidly and progress quickly, making early recognition and intervention critical to prevent further complications. If left untreated, CNS toxicity can result in seizures, loss of consciousness and even permanent brain damage, while cardiovascular toxicity can lead to arrhythmias, cardiac arrest and death. Steps that may be taken to manage LAST include [4]:
- Supportive measures: initiate basic life support (BLS) measures, including airway management and oxygen administration. Vital signs, including blood pressure, heart rate and oxygen saturation, should be closely monitored. From my personal experience, many aesthetic practitioners are not trained in most of the above.
- Intravenous lipid emulsion (ILE) therapy: has been shown to be effective in reversing the toxic effects of local anaesthetics on the CNS and cardiovascular system. The lipids in the solution bind to the local anaesthetic molecules, reducing their concentration and preventing them from binding to their targets in the nervous system and other tissues.
- Other medications such as benzodiazepines and muscle relaxants may be used to manage seizures and muscle rigidity associated with LAST. This requires specialist training which aesthetic practitioners don’t necessarily have.
- Transfer to a hospital: patients with LAST should be transferred to a hospital as soon as possible for further management and monitoring.
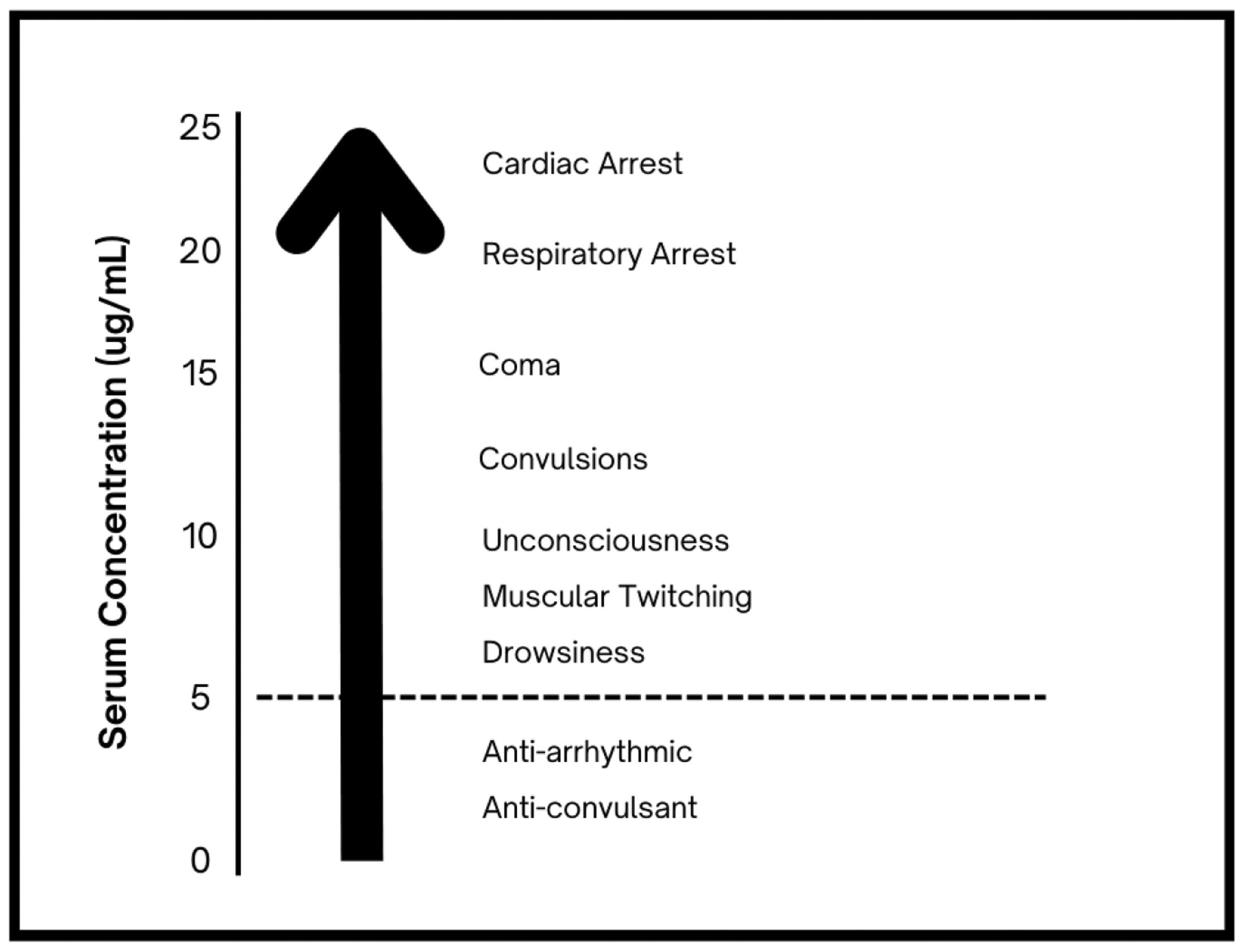
Figure 1: Serum lidocaine concentrations and systemic effects.
Based on the above, you may now understand the severity of the possible dangers caused by local anaesthetic misuse and how a robust understanding is crucial to ensure patient safety.
So, how can we mitigate these risks and create a safer environment for patients?
- Ensuring that aesthetic practitioners are properly trained and qualified in the use of local anaesthetics, including the risks and potential complications. By staying informed, well-trained, and up-to-date on the latest research and best practices, practitioners can help ensure that they are using these medications safely and effectively and are capable of managing any adverse effects that may occur.
- Regulating the practice of aesthetic medicine: it is crucial that the industry is held accountable to standards for training, qualification and practice.
- Ensuring that aesthetic practitioners have appropriate supervision: in some cases, it may be necessary for aesthetic practitioners to have appropriate supervision when administering local anaesthetics, particularly if they are inexperienced or have not received formal training.
- Ensuring that patients are fully informed: patients should be fully informed about the potential complications of local anaesthetic use, as well as the qualifications and experience of the practitioner administering the anaesthetic. This can help patients to make informed decisions about their treatment.
Conclusion
In summary, as the demand for aesthetic treatments continues to grow, it is important to raise awareness about the dangers of local anaesthetic misuse and promote its responsible use. With accountability, awareness raising, quality education, and proactive government regulation, we can minimise the risk of negative consequences and ensure the best outcomes for patients.
TAKE HOME MESSAGES
-
Safe and effective use of local anaesthesia is crucial in aesthetic procedures, however, its misuse or abuse can result in serious and potentially life-threatening consequences.
-
Many providers of aesthetic treatments are not qualified enough to consistently provide safe and adequate treatments to their patients.
-
Local anaesthetics are associated with varying degrees of risks of toxicity.
-
Local anaesthetic systemic toxicity is a life-threatening adverse reaction which can result in a range of minor to more severe effects on the cardiac or central nervous system.
-
As the demand for aesthetic treatments continues to grow, it is important to raise awareness about the dangers of local anaesthetic misuse and promote its responsible use.
References
1. Global local anesthesia drugs market size share, and COVID-19 impact analysis by drug type, by mode of administration, and by region, analysis and forecast 2021 – 2030. Spherical Insights 2022
https://www.sphericalinsights.com/
reports/local-anesthesia-drugs-market
2. Taylor A, McLeod G. Basic pharmacology of local anaesthetics. BJA Educ 2020;20(2):34-41.
3. Mahajan A, Derian A. Local Anesthetic Toxicity. StatPearls [Internet] Florida, USA; StatPearls Publishing: 2023
https://www.ncbi.nlm.nih.gov/
books/NBK499964
4. Sekimoto K, Tobe M, Saito S. Local anesthetic toxicity: acute and chronic management. Acute Med Surg 2017;4(2):152-60.
[All links last accessed 28 June 2023]
Recommended further reading
1. Marra DE, Yip D, Fincher EF, Moy RL. Systemic toxicity from topically applied lidocaine in conjunction with fractional photothermolysis. Arch Dermatol 2006;142(8):1024-6.
2. Adriani J, Campbell D. Fatalities following topical application of local anesthetics to mucous membranes. JAMA 1956;162(17):1527-30.
3. Tran AN, Koo JY. Risk of systemic toxicity with topical lidocaine/prilocaine: a review. J Drugs Dermatol 2014;13(9):1118-22.
4. Hahn I-H, Hoffman RS, Nelson LS. EMLA®-induced methemoglobinemia and systemic topical anesthetic toxicity. J Emerg Med 2004;26(1):85-8.
Declaration of competing interests: None declared.
Acknowledgement: The author would like to thank Thomas Collyer, Consultant in Anaesthesia and Intensive Care Medicine, Harrogate and District NHS Foundation Trust Hospital, for his contribution to the article.
COMMENTS ARE WELCOME








