From liposuction to adipose stem cells; from regenerative medicine to tissue engineering; and a vision of the future.
Part 3
Adipose stem cells
There is a major clinical need for strategies that adequately reconstruct the soft tissue defects after deep burns, tumour resection, or trauma. Even in 1988 the author was discussing primordial cells capable of doing everything (Figure 1).
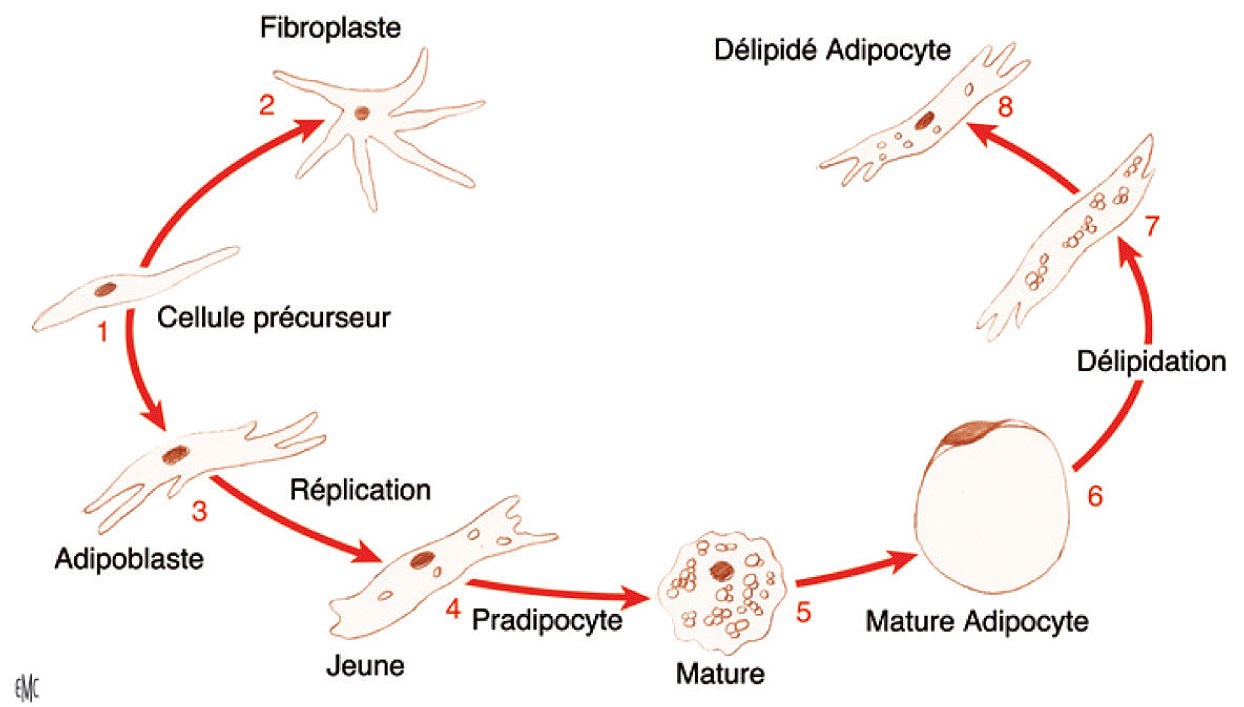
Figure 1: Scheme published by the author in 1988 to explain how a fibroblast can induce a ‘precursor cell’ (now called stem cells) and how that cell can induce an adipocyte and how that adipocyte without any food (insulin glucose) can return to a fibroblast.
Adipose stem cell application has recently been suggested as a possible novel therapy, and because of stem cells’ pluripotentiality and unlimited capacity for self-renewal, they represent a great promise for tissue engineering and are expected to allow significant advances in distinct reconstructive procedures (Figure 2).
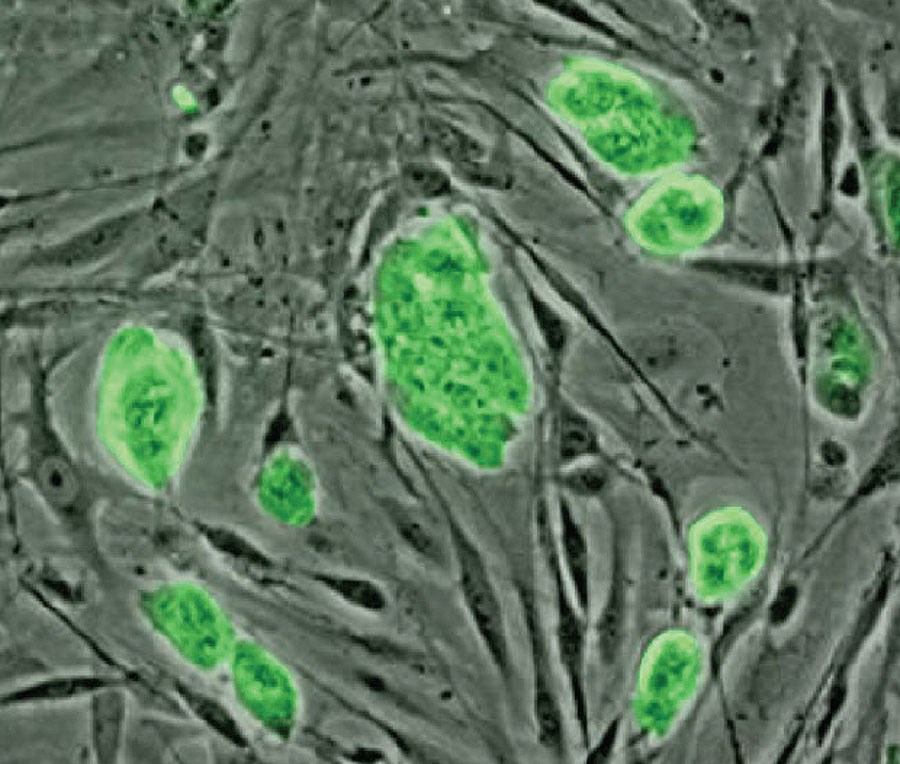
Figure 2: Microscopic view of adipose stem cells.
Adipose tissue is the most abundant and accessible source of adult stem cells. After the introduction of liposuction, adipose tissue harvesting has become easier [1]. While there is some debate as to whether the cells originate in the fat tissue or are perhaps mesenchymal or peripheral blood stem cells passing through the fat tissue, the adipose-derived stem cells (ADSCs) represent a readily-available source for isolation of potentially useful stem cells. Human processed lipoaspirate contains pre-adipocytes that possess one of the characteristic pathways of multipotent adult stem cells and are able to differentiate in vitro into mesenchymal lineages. Adipose tissue, in addition to committed adipogenic, endothelial progenitor cells and pluripotent vascular progenitor cells, also contains multipotent cell types, adipose-derived stem cells, that in cell culture conditions have shown to have an impressive developmental plasticity including the ability to undergo multilineage differentiation and self-renewal [2].
Adipose tissue has the same potential for growth of adult mesenchymal totipotential stem cells of bone marrow and can eventually be differentiated easily by the use of specific growth factors and according to the needs and applications in other cellular lines (osteogenic, chondrogenic, myogenic, epithelial). Their pluripotency, proliferative efficiency, and low donor morbidity have been amply confirmed [3]. Their therapeutic use in preclinical studies and experimental clinical trials has been documented [4,5]. Cell-assisted lipotransfer (CAL) is a novel approach to autologous fat transplantation in which adipose-derived stem cells are attached to the aspirated fat (Figure 3) [6].
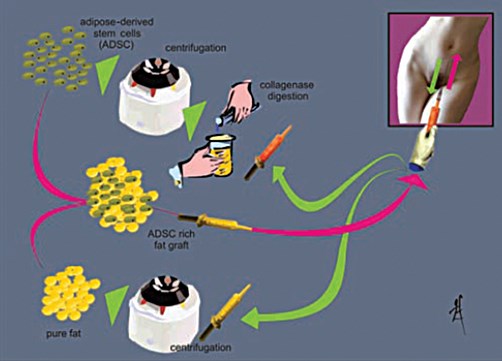
Figure 3: How to harvest fat, to isolate stem cells by centrifugation with collagenase,
how to enrich the fat with these stem cells and to perform a re-injection.
With a scaffold of a non-specific tissue (pig bladder without any cellular inclusion), so called ‘extra cellular matrix’, we can imagine taking a 3D scan picture of the disabled organ and printing that 3D scan on a 3D printer. After that autologous adipose stem cells are seeded on that structure, to obtain, after three or four weeks, a perfect, complete clone of that organ and transplant that new one without the need of a donor (Figure 4 and 5).
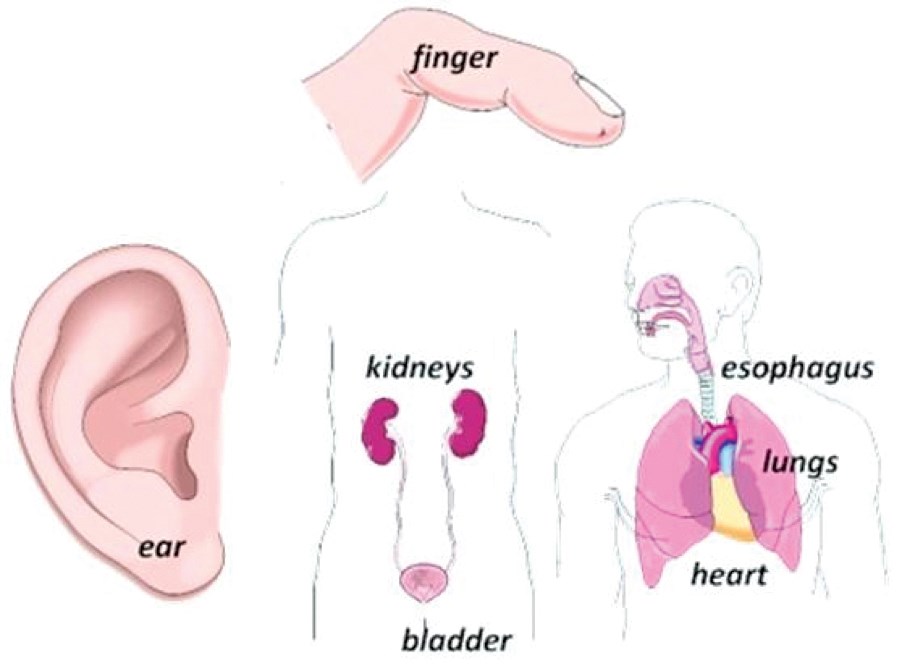
Figure 4: Tissue engineering has been successful in producing a finger, ear, kidney, oesophagus and lung.
Image has been removed.
Figure 5: It may be possible to correct any defect by a complete clone of the missing part.
We can even imagine that it is possible to reconstruct a complete organism with the DNA of that organism (Figure 6). Recently, paleontologists have expressed the theory that it is possible to create a dinosaur with the DNA found in bones.
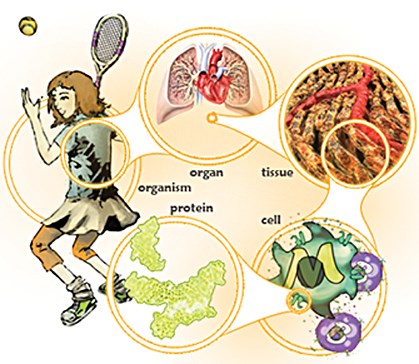
Figure 6: We can imagine that with the specific DNA and protein of an organism, it is possible to reconstitute a cell, that cell can reconstitute a tissue which can reconstitute an organ which can reconstitute a complete organism.
Other applications of fat injection and stem cells
Rejuvenation is the key word! To transfuse autologous ADSC could become a common treatment of fatigue (Figure 7).
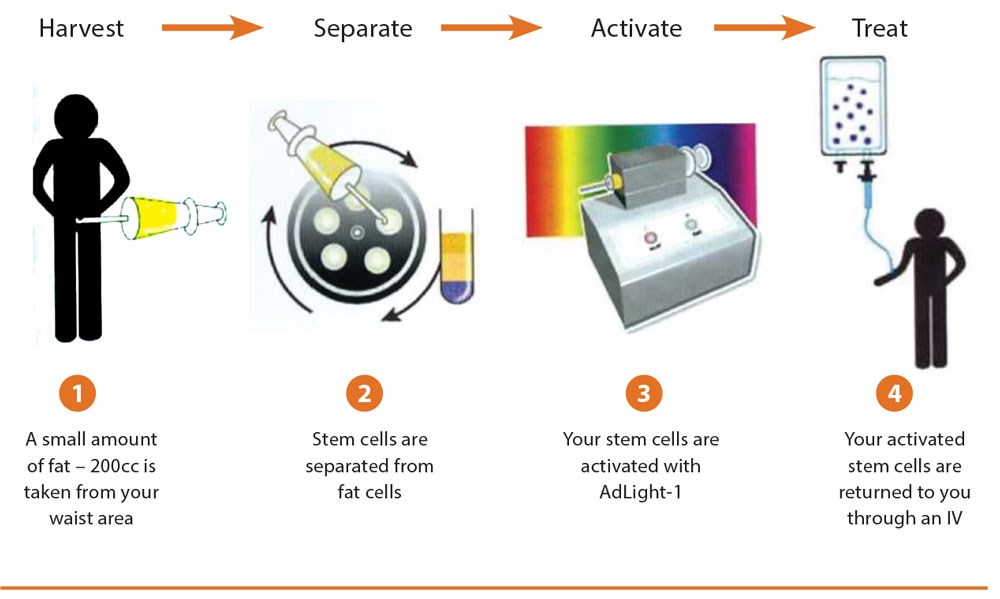
Figure 7: To rejuvenate an organism by transfusion of their own stem cells.
Adipose stem cells against cancer
When the author was a surgeon at the Gustave Roussy Institute of Cancer in France he undertook the following research:
1. Transmission of breast cancer to mice
The author transferred part of human breast cancer tumours to a series of 30 mice: 85% of these infected mice developed breast cancer, but 15% rejected the tumour as an abscess. After many repetitions the results remained the same. The conclusion was that most of the mice were ‘sensible’ to cancer, but some were ‘resistant’ to cancer. That means that some individuals are normally immune to cancer. So we can identify two kinds of families: the ‘sensible’ ones and the ‘resistant’ ones. The descendants of these families inherited the sensibility or the resistance of their parents. But, if a newborn mouse from a sensible family was fed by a ‘resistant’ mother, this mouse became resistant, while, if a ‘sensible’ mother fed a ‘resistant’ newborn, this individual became ‘sensible’. This led to the conclusion that the antibodies against cancer were being transmitted through the mother’s milk.
That means too that the ‘cancer’ is behaving like any ‘infection’ sensible to some kind of antibodies. That’s why we can conclude that the breast cancer (like any other cancer) is induced by a substance like a ‘germ’ or even probably a virus or ultra virus (named ‘virus K’ by the author).
This ‘virus’ seems to act like the AIDS virus, penetrating the cell nucleus to change the programme, by stopping the ‘apoptosis’ of the cell and so transforms the cell into an ‘immortal and monstrous cell’ as can be seen in a microscopic study of cancer cells. AIDS patients can die by opportunist ‘infections’ but many die from liver cancer or Kaposi cancer as they have no antibodies to fight against cancer.
Certain facts seem to confirm my viral theory. Today, everybody agrees that cervical cancer is induced by a transmissible papillomavirus. While, in the animal world, a facial cancer of the Tasmanian Devil in Australia is transmissible and epidemic. These facts are in favour of the existence of a transmissible ‘germ’ responsible of inducing a cancer and sensible to specific antibodies as are any other germs.
2. Autologous fat as a protector against cancer
In 1983 the author started to inject autologous fat into women’s breasts to induce a mammary augmentation or to correct some mammary defects [7]. After 25 years of follow-up, there was no development of cancer. Statistics demonstrate that some breast cancer must appear during these 25 years, but no cancer appeared! So, fat is not responsible for inducing breast cancer but, on the contrary, seems to protect the breast against cancer. Because adipose stem cells are the ‘active’ and ‘regenerative’ part of fat, we can conclude that adipose stem cells are protecting against cancer. We followed this with some experimentation on mice and the results are more than encouraging. These are being written up by the author.
Beyond liposuction
In the near future plastic surgery will become increasingly simple and efficient and, with a simple syringe we will be able to do:
- Liposuction
- Fat filling anywhere in the body
- Face rejuvenation
- Breast augmentation
- Buttock augmentation
- Treatment of disease.
While, with a scaffold we can make a new organ, with an extracellular matrix powder we can heal and regenerate, and with autologous adipose stem cells, we could treat cancer.
Adipose stem cells, as well as telomeres and nanotechnologies and a better knowledge of brain physiology, will bring us to a much longer life in good shape and health. It is possible to imagine that an individual of 90-years-old will look and will feel like an individual of 60-years-old and life will potentially last to 120 or even 140 years (Figure 8).
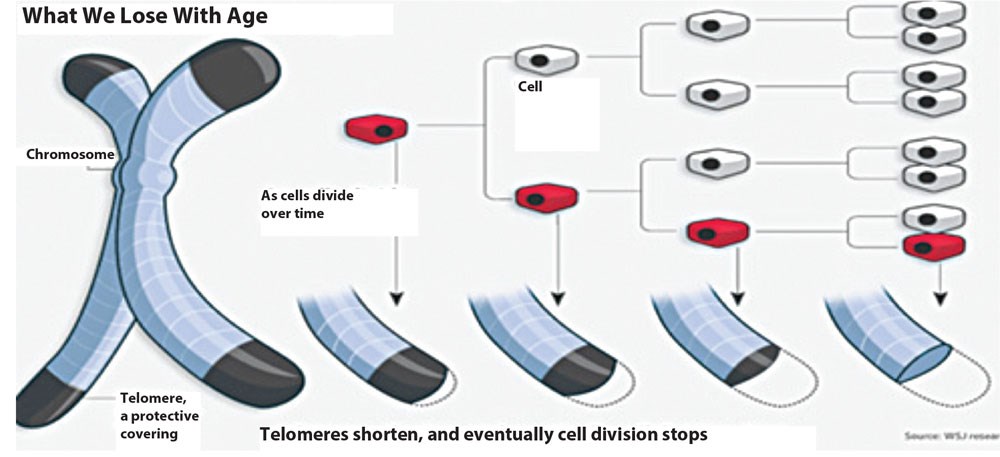
Figure 8: Telomeres become shorter with age. Scientists have found a ‘diastase’ to correct that shortening. Mice treated with that ‘diastase’ are living longer than usual; a great hope to obtaining a longer life for human beings.
Discussion
The author always emphasised the principles which must be followed at all times in order to achieve optimum, aesthetically pleasant results [8]. The core idea is to avoid trauma to the connective tissue septi that connect the skin to the underlying structures. By doing so, one can achieve, not only, better skin retraction postoperatively, but also retain blood vessels, lymphatics and nerve endings.
From the very beginning he introduced the importance of blunt instrumentation for atraumatic aspiration. Additionally, he emphasised the importance of the anatomic layers of the fat and insisted on aspirating deeply and retaining the superficial fat (Figure 9), as removal of the latter can cause postoperative contour irregularities in inexperienced hands [9]. The liposuction technique is easily reproducible for almost all areas of the body. It can be combined with other procedures to improve the final outcome both in cosmetic procedures (e.g. abdominoplasty and innerthighplasty, face rejuvenation) and reconstructive surgery (e.g. defatting of the flaps). It has permanent results and there is no recurrence of the fat tissue once removed. The latter supports the adiposity theory’s main concept: “once an adipocyte is destroyed it cannot reoccur [10]”.
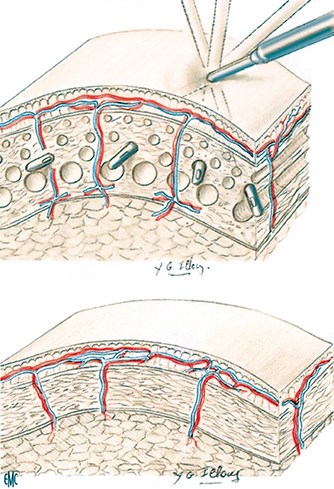
Figure 9: The round tipped blunt cannula avoids destroying vessels
and nerves and remove only fat. It is a ‘Swiss cheese technique’.
Last, but not least, in liposuction there are significantly lower complication rates (seromas, haematomas, skin irregularities, etc.) when compared to other body contouring modalities [10-12]. The main limitation of liposuction, as identified early on by the author [8], is the poor outcome in patients who have extensive lipodystrophy with ptosis. Poor skin quality will not achieve satisfactory results and these patients are more likely to benefit from some type of dermolipectomy rather than pure lipoaspiration. Another precaution that one should keep in mind is the volume of the aspirated fat. The author initially reported 6lbs (Editor’s comment: 6lb=2.7kg. With fat having a density of 0.918 gm/cc that gives a volume of 2.5 litres) of aspirated fat as a safe cut-off [8]. The interplay of volume injected, volume aspirated, total blood loss, and intravenous fluid administration is also very important for the appropriate management of the patient [13,14].
Liposuction has been largely embraced by the surgical community over the last 37 years. Fat injection, however, remains an issue of conflict and controversy. Some claimed it worked while others believed it didn’t. Fat transfer for composite body contouring became the new ‘hot shot’ and research focused on whether adipose cells can survive after injection or not. Early experience showed that fat graft reabsorption was the main drawback, with 50-90% graft loss [15-17]. Studies have shown that the ideal way to harvest fat is by using a 10ml syringe connected to a 2mm cannula [18]. It is also wise to avoid using lidocaine as part of the tumescent solution when fat grafting, as studies have indicated decreased adipocyte proliferation after exposure to lidocaine [19].
As a final point, the plane of the injected fat has been shown to affect the survival of adipocytes. A recent study [20] showed that injecting into the supramuscular plane has a better graft take compared to the subcutaneous or submuscular planes. Today, centres around the world offer fat grafting as their final perfecting procedure after breast reconstruction in order to further enhance cosmetic outcomes or to correct congenital anomalies [21,22]. Illouz and Sterodimas published their 25-year experience with autologous fat transplantation to the breast [23]. Three groups of patients were included in the study: (1) After breast reconstruction; (2) Congenital breast asymmetries; and (3) Breast augmentation. The authors reported excellent cosmetic results, high patient satisfaction as well as low complication rates. Caution, however, is mandated due to the fact that the most common complication of breast lipografting is formation of liponecrotic cysts (Figure 10).
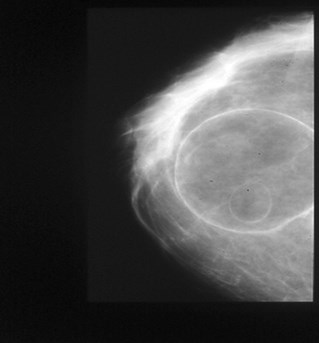
Figure 10: Huge oil cyst after a massive fat injection of 100ml at the same place. Injections
must be done drop by drop to avoid the necrosis of the centre of the fat injected.
As a result it is mandatory for the surgeon to know the appearance of the breast on mammography and ultrasonography, and the evolution of fat necrosis patterns after fat injection. It is easy to see the difference between a fat necrosis and a cancer calcification.
In conclusion, fat is viewed as the ideal filler as it is not allogenic, is widely available, easily collected and has minimal morbidity. Adipose tissue stem cell-based regenerative strategies hold tremendous promise, although this potential must be balanced against stringent standards of scientific and clinical investigation, before developing ‘off-the-shelf’ tissue engineering products [5].
Determining the effectiveness of any cosmetic procedure involves subjective rather than objective criteria. However, survey findings among physicians who use liposuction indicate that the procedure achieves a high level of good results (up to 80% of surgeons and 90% of patients) with a very low level of complications [10].
In the hands of an experienced practitioner, complications from this procedure are very low. It is very important that potential liposuction patients be counselled in advance about the differences between the natural sequelae of the procedure and a true medical complication.
Conclusions
Liposuction is now an accepted and safe procedure that can be used by experienced and skilled practitioners to assist in improving a patient’s aesthetic appearance. With proper patient selection and good counselling on realistic expectations, liposuction can be expected to achieve excellent results with a low complication rate.
On a different note, fat, previously considered as a non useful tissue, has the potential to be a reserve of organ parts while fat stem cells may become a treatment for almost every kind of disease and may at the same time be the key to a longer and healthier life.
References
1. Illouz YG. Body contouring by lipolysis: a 5-year experience with over 3000 cases. Plast Reconstr Surg 1983;72:591-7.
2. Liu ZJ, Zhuge Y, Velazquez OC. Trafficking and differentiation of mesenchymal stem cells. J Cell Biochem 2009;15:984-91.
3. Ogawa R. The importance of adipose-derived stem cells and vascularized tissue regeneration in the field of tissue transplantation. Curr Stem Cell Res Ther 2006;1:13-20.
4. Sterodimas A, De Faria J, Correa WE, Pitanguy I. Tissue engineering in plastic surgery: an up-to-date review of the current literature. Ann Plast Surg 2009;62:97-103.
5. Sterodimas A, De Faria J, Nicaretta B, Pitanguy I. Tissue engineering with adipose-derived stem cells (ADSCs): current and future applications. J Plast Reconstr Aesthet Surg 2010;63:1886-92. 6. Sterodimas A, De Faria J, Nicaretta B, et al. Cell-assisted lipotransfer. Aesthet Surg J 2010;30:78-81.
7. Flynn TC, Coleman WP 2nd, Field LM, et al. History of liposuction. Dermatol Surg 2000;26:515-20.
8. Illouz YG. Illouz’s technique of body contouring by lipolysis. Clin Plast Surg 1984;11:409-17.
9. Bjorntorp P, Ostman J. Human adipose tissue dynamics and regulation. Adv Metab Disord 1971;5:277-327.
10. Pfulg ME. Complications of suction for lipectomy. Plast Reconstr Surg 1982;69:562-3.
11. Vilain R. Suction curettage or not: that is the question. Plast Reconstr Surg 1982;69:1026-7.
12. Schrudde J. Suction curettage for body contouring. Plast Reconstr Surg 1982;69:903-4.
13. Kenkel JM, Lipschitz AH, Luby M, et al. Hemodynamic physiology and thermoregulation in liposuction. Plast Reconstr Surg 2004;114:503-13;discussion 514-15.
14. Rohrich RJ, Leedy JE, Swamy R, et al. Fluid resuscitation in liposuction: a retrospective review of 89 consecutive patients. Plast Reconstr Surg 2006;117:431-5.
15. Chajchir A. Fat injection: long-term follow-up. Aesthetic Plast Surg 1996;20:291-6.
16. Niechajev I, Sevcuk O. Long-term results of fat transplantation: clinical and histologic studies. Plast Reconstr Surg 1994;94:496-506.
17. Mikus JL, Koufman JA, Kilpatrick SE. Fate of liposuctioned and purified autologous fat injections in the canine vocal fold. Laryngoscope 1995;105:17-22.
18. Gonzalez AM, Lobocki C, Kelly CP, Jackson IT. An alternative method for harvest and processing fat grafts: an in vitro study of cell viability and survival. Plast Reconstr Surg 2007;120:285-94. 19. Shoshani O, Berger J, Fodor L, et al. The effect of lidocaine and adrenaline on the viability of injected adipose tissue–an experimental study in nude mice. J Drugs Dermatol 2005;4:311-16.
20. Karacaoglue E, Kizilkaya E, Cermik H, Zienowicz R. The role of recipient sites in fat-graft survival: experimental study. Ann Plast Surg 2005;55:63-8.
21. Kaufman MR, Miller TA, Huang C, et al. Autologous fat transfer for facial recontouring: is there science behind the art? Plast Reconstr Surg 2007;119:2287-96.
22. Sterodimas A, Huanquipaco JC, De Souza Filho S, et al. Autologous fat transplantation for the treatment of Parry-Romberg syndrome. J Plast Reconstr Aesthet Surg 2009;62:e424-6.
23. Illouz YG, Sterodimas A. Autologous fat transplantation to the breast: a personal technique with 25 years of experience. Aesthetic Plast Surg 2009;33:706-15.
Declaration of competing interests: None declared.
CLICK HERE FOR PART 1 or HERE FOR PART 2
COMMENTS ARE WELCOME





