During the ageing process, many different anatomical changes contribute to the aged appearance of the face [1]. Focusing on the forehead, typical age-related changes are regression of the hairline, solar damage, skin laxity, dynamic wrinkles, reduction of fat and bone resorption. As with other facial areas, the ideal approach for treating the forehead is a multi-level, multi-modality treatment that targets all of these age-related anatomical changes.
Thus, a personalised treatment plan is necessary for each patient after assessing the entire forehead, and its relationship with adjacent aesthetic units including the periorbital and the temporal areas. It is also essential to discuss with the patient their concepts of beauty as well as cultural aspects that may influence the desired outcome.
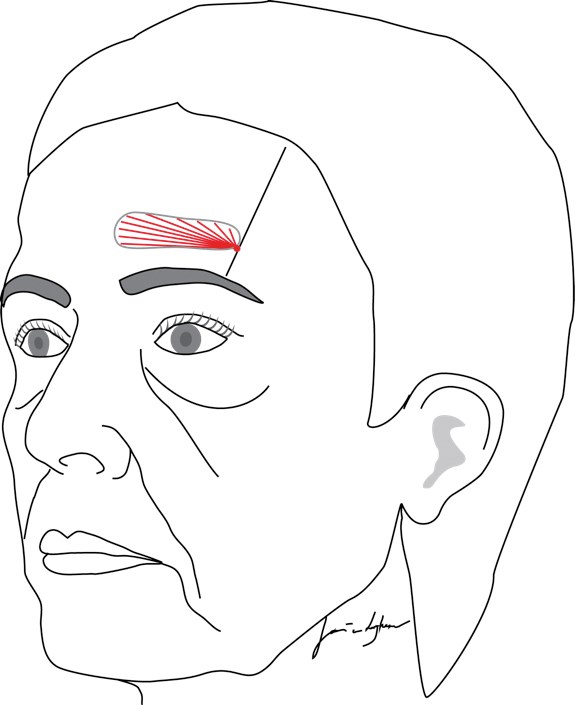
Figure 1: Schematic drawing of product injection at the frontal concavity. The straight line marks the medial border of the temporal crest. The red dot marks 1-2cm above the orbital rim and the red lines indicate the subgaleal retrograde linear threads of soft-tissue filler.
The frontal concavity
The frontal concavity is a depression that disrupts the youthful contour of the forehead and changes the light reflection. It runs approximately parallel to the supraorbital rim, just cranial to the brows and it is believed to be the result of predominantly bone resorption, but volume loss in the superficial fat and the frontalis muscle can also play a role. Commercially available soft tissue filler products can be used to correct this loss of volume and can be placed in different anatomical levels:
Intradermal / dermal
To correct wrinkles, thin to medium thickness soft tissue fillers can be used for treatment while keeping in mind that the wrinkles here are dynamic and will also benefit from pre-treatment with botulinum toxin. Ideally, a filler with a low visco-elasticity, but high cohesivity should be used, preferably in a blanching technique (indicating papillary dermis placement) to correct forehead wrinkles. In order to inject intradermally, a sharp needle should be used, as non-traumatic cannulas do not penetrate the dermis. Subsequently, arterial danger zones have to be considered and care should be taken that the needle tip does not proceed through the dermis, but rather stays intradermally [2].
Subcutaneous
In the superficial fat compartments (the central forehead fat compartment, the middle forehead fat compartment and the lateral temporal cheek fat compartment) [3]; medium-thickness fillers can be used for volumising the frontal concavity. Caution should be taken as important danger zones run in this area: the supraorbital artery (medial branch), the supra trochlear artery, the central forehead artery and their branches. Intra-arterial injection into any of these arteries can potentially lead to permanent blindness [4], so injection with a non-traumatic cannula should be considered. On movement of the brows, superficially placed product can potentially be seen as the position of the filler will change relative to the concavity. This will result in a visible convexity just above the concavity when the patient raises the brows which might produce a suboptimal aesthetic result [4].
Intramuscular
Soft tissue fillers are generally not injected, as muscular contractions can displace the product and cause visible nodules. Both intramuscular injection and intragaleal injection will result in the same aesthetic problem as subcutaneous injection: the position of the product will change on animation [1].
Therefore, the ideal depth for placing soft-tissue fillers is in the subgaleal and supraperiosteal spaces and generally a medium to thick filler should be used, with high viscoelastic properties. The ideal instrument is a non-traumatic cannula to reduce the chance of intra-arterial injection of the supraorbital artery (lateral branch) and its branches. Also, a cannula will likely provide more precision with respect to product placement in the subgaleal level compared to sharp needle injection [5].
Step-by-step technique
- A supraorbital nerve block may be considered.
- Mark the frontal concavity and the medial border of the temporal crest.
- On that line, approximately 1-2cm above the orbital rim, a low-risk access point can be marked, although the location of the superficial temporal artery is known for its anatomic variability. The temporal branch of the facial nerve is dividing in many branches, while the main branch passes the temporal crest more cranially to that point.
- If needed, anaesthetise this point before using a needle to make a puncture in the skin.
- With a rigid cannula (e.g. 25G, 50mm), advance through the skin until the subcutaneous fat is reached.
- With thumb and index finger of the non-dominant hand, pinch the skin just in front of the cannula so that the muscle is lifted from the periosteum. Thus a horizontal path of least resistance toward the deep level has been created.
- Manoeuvre the cannula through the resistance of the galea. This requires a well-controlled amount of force, as the galea can be quite tough here. Usually, a pencil-rolling technique can be of value [1], where the syringe is rotated between the fingers in order to let the tip of the cannula find the path of least resistance.
- Advance the cannula in the subgaleal space while lifting the muscle in front of the cannula and start at the most caudal part of the frontal concavity, as many products contain lidocaine that will anaesthetise the supraorbital nerve.
- Place multiple retrograde linear threads in a fanning technique.
- Even out the product with direct massage.
After injection, the frontalis muscle might be temporarily relaxed due to the lidocaine in the product. Also, transient distension of the veins can be observed due to increased pressure in the area. Swelling might be uneven in the forehead, so the patient should be advised that any swelling is to be expected and is temporary.
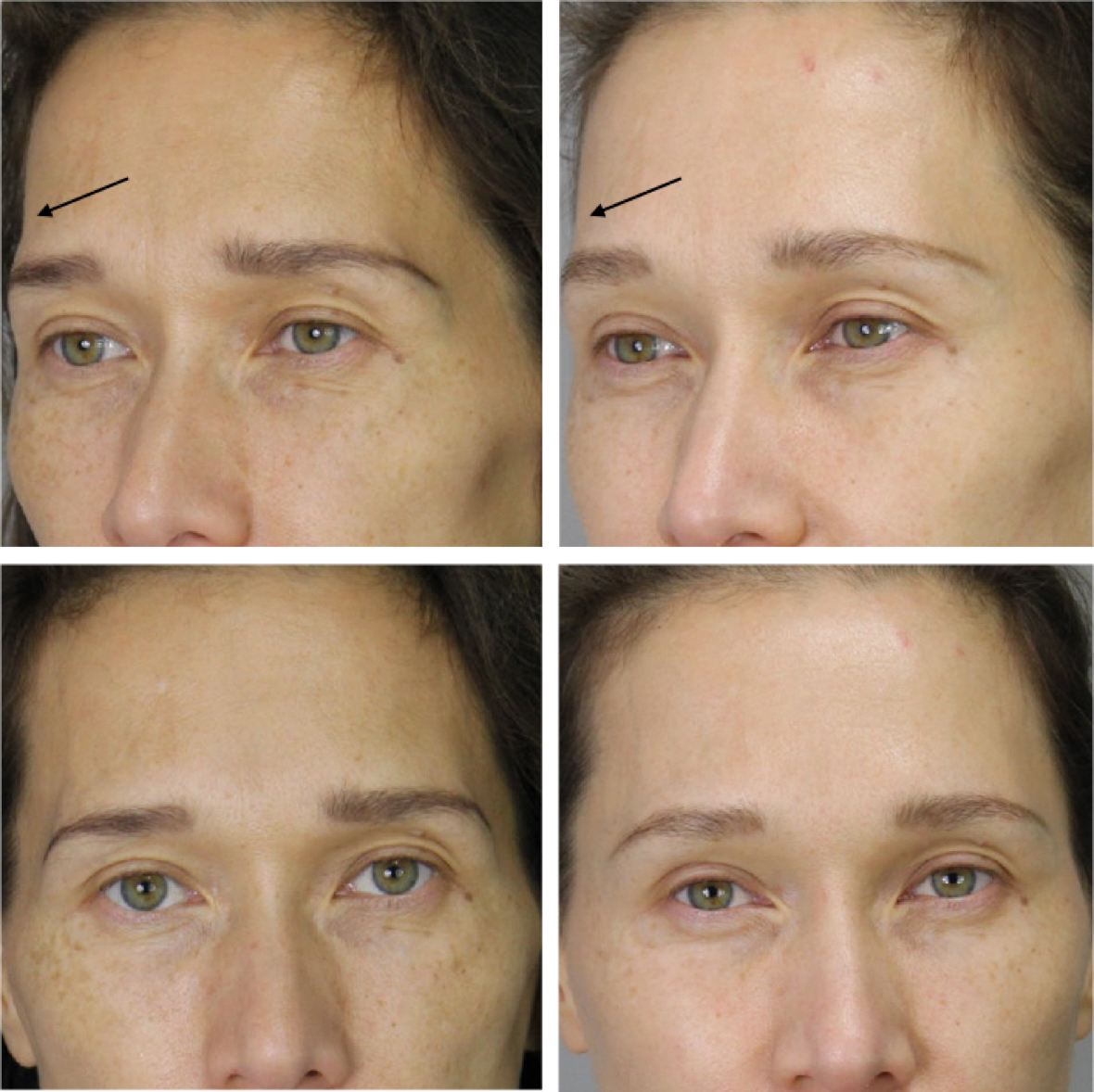
Figure 2: Example of a patient treated with 1ml of hyaluronic acid (Belotero Intense) in the subgaleal level, resulting in a more optimal light reflection of the forehead (this patient has also been treated in other facial areas).
References
1. Van Loghem J, Yutskovskaya Y, Werschler P. Calcium Hydroxylapatite over a decade of clinical experience. J Clin Aesthet Dermatol 2014;7:38-49.
2. Prager W, Michiels P. A prospective, comparative survey to investigate practitioners’ satisfaction with a cohesive, polydensified-matrix®, hyaluronic acid-based filler gel with and without lidocaine for the treatment of facial wrinkles. J Cosmet Dermatology 2015;14:124-9.
3. Rohrich R, Pessa J. The fat compartments of the face: anatomy and clinical implications for cosmetic surgery. Plast Recon Surg 2007;119:31S-39S.
4. Li X, Du L, Lu JJ. A novel hypothesis of visual loss secondary to cosmetic facial filler injection. Ann Plast Surg 2015;75:258-60.
5. Van Loghem J, Humzah D, Kerscher M. Cannula versus sharp needle for placement of soft tissue fillers: An observational cadaver study. Submitted for publication.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME