In the UK approximately 40,000 women are diagnosed with breast cancer every year. About 40% of these need, or choose, to undergo mastectomy, where all of the breast tissue is removed. Currently around a third of these patients choose to undergo breast reconstruction, two thirds of these at the time of mastectomy (immediate reconstruction) and the rest later (delayed reconstruction). All patients undergoing mastectomy should be offered breast reconstruction as this has been shown to increase patient satisfaction [1].
There are several options for breast reconstruction, which may be divided into implant-based or flap-based (autologous) reconstruction using the patient’s own tissues. Implant-based reconstruction often involves the use of adjustable saline tissue-expanders initially which usually require replacement with a definitive silicone implant at a later date. Autologous flap surgery uses a combination of skin, fat, and sometimes part of the underlying muscle. The flap is moved from areas such as the abdomen, upper back, inner thigh, upper hip, or buttocks to the chest where it is shaped into a new breast. For implant-based reconstruction, 34% of patients suffer complications such as capsular contracture or a foreign body scarring reaction, which require them to have further surgery within five years [2].
Autologous flaps can be pedicled or free. The most common example of the former is the latissimus dorsi flap, where donor tissue remains connected to the original donor site via an intact vascular pedicle. In contrast, free flaps are completely detached from the body with division of the vascular pedicle, and then the blood supply is re-established using microvascular surgery techniques. The two most common free flap procedures for breast reconstruction are the transverse rectus abdominis muscle (TRAM) free flap and the deep inferior epigastric perforator (DIEP) free flap, named after the vascular pedicle that perfuses it. These procedures harvest an ellipse of lower abdominal tissue and the flap is then transferred to the chest. Unlike the TRAM flap, where one rectus abdominis muscle is taken, the DIEP procedure spares the rectus abdominis muscle which helps to preserve abdominal strength, halving the likelihood of a bulge or hernia, and shortens recovery time. Because of this, the DIEP flap is now considered the gold standard for free flap breast reconstruction and will be the main focus of this article.
The DIEP flap
The DIEP flap was first described in the literature in 1994 by Dr Robert Allen from the USA [3]. It is a microvascular free flap using a woman’s own tissue, composed of skin and fat from the abdomen, without muscle, to recreate a ‘natural’ breast. Contrary to implant-based reconstruction, once the primary reconstruction and secondary fine-tuning are complete, no long-term input from the surgeon is required. This is because, once transferred and shaped into the new breast, it is living tissue which ages naturally and changes volume corresponding to the patient’s overall body weight. It has the additional advantage of leaving a cosmetically improved donor site, as the abdominal tissue that is transferred corresponds to the tissue that would be removed during a full abdominoplasty (‘tummy tuck’).
There is great variation in national and international perioperative practice in DIEP flap breast reconstruction, and there is little evidence-base supporting exact protocols. The Royal Marsden, London protocol that has been developed for DIEP flap breast reconstruction provides a safe and high quality pathway and results in a flap success rate of 99.5%. We describe the protocol here.
Immediate versus delayed reconstruction
For most women the whole process of diagnosis, mastectomy, reconstruction, recovery and other treatments such as chemotherapy or radiotherapy can be a very daunting rollercoaster. It is difficult to make big decisions during this time, such as whether to have reconstruction at all, or whether to have reconstruction immediately or at a later time. However, studies show that immediate reconstruction results in better outcomes and improved patient satisfaction, with less extensive scarring than delayed reconstruction. The main reason for this is that the majority of the skin of the breast can be preserved in the form of a skin-sparing mastectomy and then re-filled with the DIEP flap. In contrast, when a delayed reconstruction takes place, the majority of the new breast skin comes from the abdomen. Women should be supported and given this information so that they can make informed choices at this difficult time.
Nipple sparing mastectomy
Nipple-sparing mastectomy can result in reconstructions that look very similar to the original breast, with a small scar, usually in the fold under the breast. The indications for this are a small tumour, distant from the nipple, with a sufficient sized breast to get a clear margin. The nipple is simply viewed as another margin.
Relative contraindications to DIEP flap reconstruction
Slim women with very little abdominal subcutaneous fat may not have enough donor tissue, but we have found it possible to perform this in most cases. In these women another excellent option is the transverse upper gracilis (TUG) flap, which uses one or both inner thighs as the donor site, giving the cosmetic donor site result of a ‘thigh lift’.
Unilateral versus bilateral reconstruction
There has been an increase in bilateral reconstructions, partly as a result of awareness of BRCA1 and BRCA2 mutations and the ‘Angelina effect’ [4]. If bilateral reconstruction is to be performed using DIEP flaps it must be done in one operation as the DIEP flap can only be used once. This requires careful planning and preoperative genetic testing in high-risk women.
Patient selection
The importance of appropriate patient selection is a well-known predictor of good outcomes in microsurgery. As a result, most of the women presenting for DIEP reconstruction are relatively healthy apart from their breast cancer. Advanced age alone is not a contraindication to surgery as long as co-morbidities and general health allow the patient to undergo long and extensive surgery. Although smoking is not an absolute contraindication, smokers are advised to stop smoking for at least four weeks before surgery. Nicotine-induced vasoconstriction, carbon monoxide-related tissue hypoxia, and blood hypercoagulability caused by increased platelet aggregation can cause problems with breast skin flap vascularity and donor site morbidity. Similarly, obese patients having delayed reconstruction may be advised on weight reduction methods before surgery to improve surgical outcome. Absolute contraindications to surgery are hypercoagulable states, such as sickle cell anaemia and polycythaemia, which greatly increase the risk of anastomotic thrombosis.
DIEP flap breast reconstruction and radiation
Contrary to implant-based reconstruction the expected need for radiotherapy following mastectomy is not a contraindication for immediate reconstruction using the DIEP flap. If radiotherapy is given following mastectomy without reconstruction, it is best to wait until the acute effects of radiation on tissues has subsided, typically six to 12 months, before further surgery, although this can be sooner.
Radiotherapy has occasionally been seen to reduce flap volume and some patients have a temporising implant while radiation is given, to preserve the skin envelope of the breast. The implant can then be replaced at a later date with the DIEP flap for an improved long-term outcome.
Counselling and consent
Patients are seen at least twice in clinic before surgery. Consent is obtained where possible in clinic prior to surgery. The pathway, general and specific risks of DIEP flap reconstruction are covered in depth. Specific risks include 0.5% risk of flap failure in our unit, as well as flap fat necrosis, abdominal bulge or hernia.
Preoperative imaging
CT angiograms are an essential part of preoperative planning. We have found these to be very accurate in identifying suitable abdominal donor site perforator vessels, which contributes to both safety and reduced operating times.
Pre-assessment and preparation for the procedure
All patients are pre-assessed prior to surgery. A thorough assessment is essential before anaesthesia, and should follow general principles, including adequate planning of anaesthesia and postoperative care. Routine preoperative blood tests are taken (haematology and biochemistry, group and save). Standard clinical photographs are obtained and patients are advised to stop smoking.
Patients are asked to obtain a loose-fitting sports bra to bring in for the operation that they don’t mind having a hole cut into for postoperative flap monitoring. This should have no under-wires, and preferentially do up at the front. Patients are also advised to acquire some high-waisted supportive pants to be worn postoperatively to support their abdomen. Abdominal binders are not routinely used as these can roll up and be uncomfortable.
Preoperative low molecular weight heparin (tinzaparin) is prescribed to reduce the risk of venous thromboembolism. The dose is calculated based on the patient’s weight. This is injected into the buttock or thigh and not the abdomen as the flap will be raised from the abdomen. Tinzaparin is routinely given the night before surgery. Where this is not possible this is given on induction. We have not found this to cause increased bleeding. Patients are asked to remain nil by mouth from midnight for food; small sips of water may be taken up to 6am if preferred by patients.
On the morning of surgery
Patients arrive at 7.30am on the day of surgery, when they are marked up by the surgical team. This includes reference points and so not all marks correspond to incisions. Patient consent is confirmed. Patients are prepared for theatre by the nursing staff and are taken to theatre at 8am.
Anaesthesia
Owing to the long duration of surgery, patients are intubated and ventilated. Venous access is gained with a large gauge peripheral line on the opposite side to surgery as many women will have undergone axillary lymph node sampling or clearance. In women who have undergone chemotherapy, this can be challenging and central venous access may be required. An arterial line is also sited to monitor blood pressure accurately throughout the operation, and allow blood sampling in the postoperative period. Blood pressure measurement or intravenous cannulae are avoided in any limb prone to lymphoedema. In addition, a urinary catheter and core temperature probe are used. Anaesthesia can be maintained using a volatile anaesthetic in oxygen-enriched air or a propofol infusion.
Patient positioning, comfort and deep venous thrombosis prophylaxis
Careful positioning of the patient is imperative to avoid peripheral nerve damage and pressure sores. During the procedure patients are supine on the operating table with arms abducted (crucifix position) on padded arm boards supported on gel pads and gently flexed at the elbows. Care is taken to ensure abduction is less than 90 degrees to prevent brachial plexus injury. Padding is also placed underneath the heels, with a pillow under both knees. At the end of the procedure, the patient will be positioned with both hips and knees flexed, supported on two or three pillows to prevent tension on the abdomen.
Deep venous thrombosis is a risk in prolonged surgery. Anti-embolism stockings and cyclically inflating Flowtron® boots (calf-pumps) are used in addition to tinzaparin as described above.
“The DIEP flap is raised at the same time as mastectomy in immediate breast reconstruction, and this shortens the operating time.”
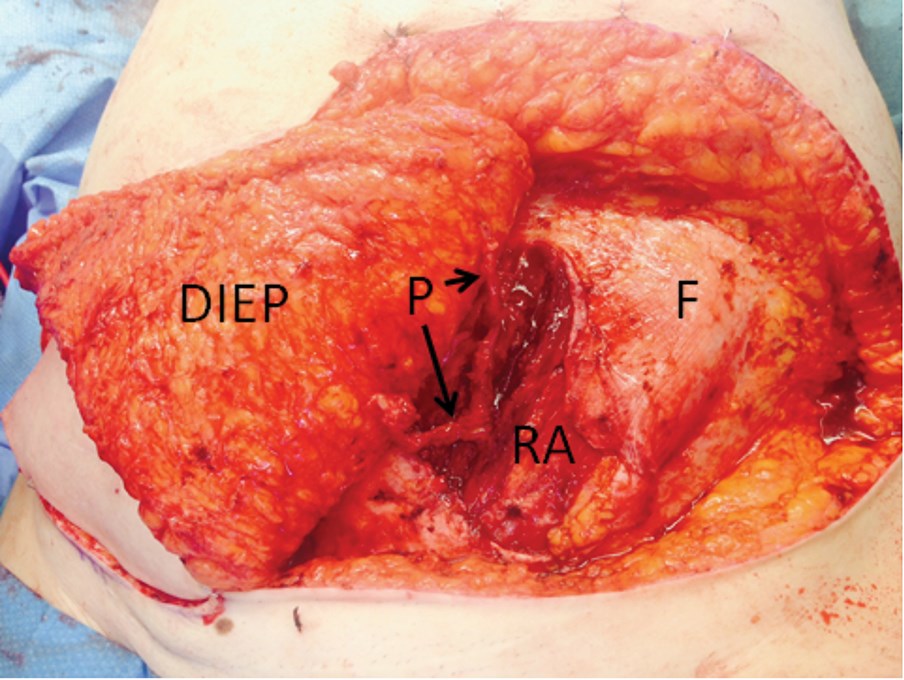
Figure 1: Intraoperative view of DIEP flap viewed from foot of the operating table. The flap has been reflected to the patients right side (to left of diagram) with two vascular perforators (P) shown as they are dissected through a vertical separation in the rectus abdominis (RA) muscle, seen under the deep fascia (F), which is opened for access to the vessels [5].
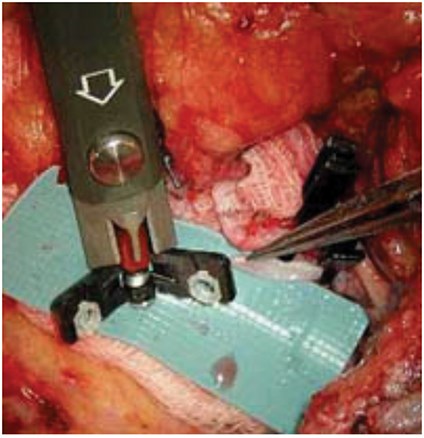
Figure 2: Intraoperative view of venous coupler device on the left of the photograph prior to anastomosis of the veins, one of which is seen held on the right of the picture.
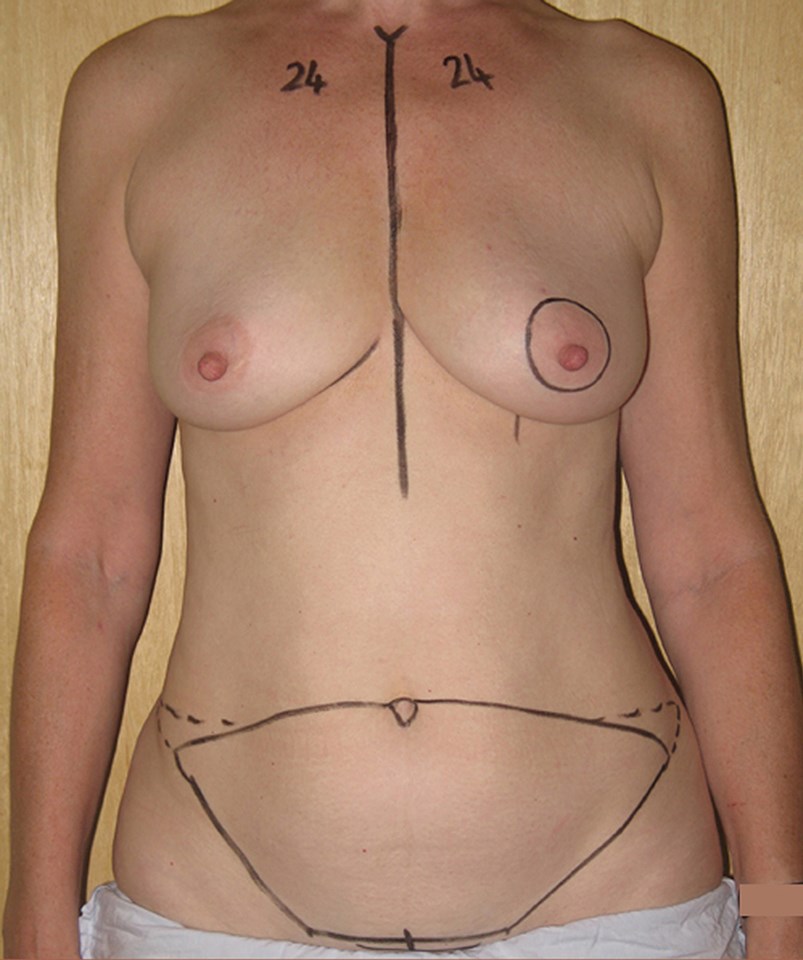

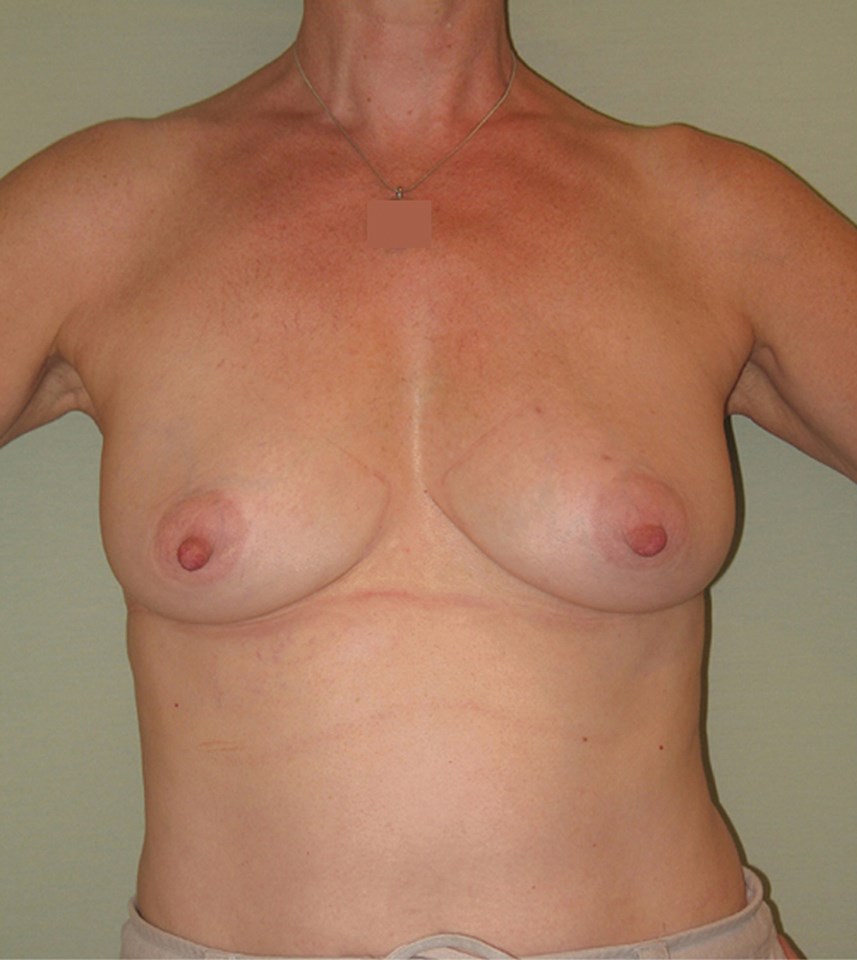
Figure 3. This series of clinical photographs in the same patient shows how a natural attractive breast can be recreated using DIEP flap breast reconstruction. Preoperative view (3a); Preoperative marking (3b); Postoperative view (3c).
Surgical procedure
Surgery may be four to eight hours long, and is longer for bilateral reconstructions. The DIEP flap is raised at the same time as mastectomy in immediate breast reconstruction, and this shortens the operating time.
DIEP flap breast reconstruction involves three main stages:
- Raising of the flap with dissection through a temporary vertical split in the rectus abdominis muscle to meticulously separate out the small perforator vessels originating from the deep inferior epigastric artery (Figure 1).
- Microvascular anastomosis of the flap to the internal mammary artery and vein in the chest using a surgical microscope. The internal mammary vessels are accessed between the costal cartilages in the chest. These vessels are chosen because of their proximity to the breast and excellent size match with the vessels of the flap. Some surgeons elsewhere prefer to use the blood vessels in the axilla although this is rare. The veins are usually connected with a venous coupler device (Figure 2), whereas the arteries are usually sewn together with sutures that are finer than human hair and only just visible with the naked eye, hence the need for the microscope.
- Insetting of the flap, shaping of the transferred tissue and abdominal donor site closure.
As the microsurgical success rates are so high the emphasis is placed on aesthetic outcome: to this end, a great deal of the operation is spent shaping the new breast. The aesthetic goal should not be simply to create a breast ‘mound’, but should reflect the patient’s desires, recreating natural breast beauty (Figure 3), taking into account breast asymmetries and plans for a second stage of surgery where final adjustments are made. The abdominal donor site cavity may be quilted using a ‘barbed’ suture to reduce the incidence of seroma. There may be up to two low suction abdominal drains placed through the pubic area and one to two drains in the breast (depending on whether an axillary dissection has been performed). The breast reconstruction skin paddle and abdominal wound are sutured with absorbable sutures, tissue glue is applied to seal the wound and allow early showering. Micropore® tape is applied to the wounds.
“The aesthetic goal should not be simply to create a breast ‘mound’, but should reflect the patient’s desires, recreating natural breast beauty, taking into account breast asymmetries and plans for a second stage of surgery where final adjustments are made.”
Postoperative care
The patient will be put into their sports bra at the end of the case and a hole will be cut into it for flap observation. Poor flap perfusion, although rare, should be rapidly identified with expeditious return to theatre before compromise becomes irreversible. The patient will initially go to recovery and will need flap observations every 15 minutes for the first four hours postoperatively and thereafter every half hour overnight. Flaps are monitored closely using clinical parameters and a hand-held Doppler device. The following flap observations are made: flap colour, temperature, whether the flap feels soft or firm, capillary refill, Doppler signal, and are recorded on a specific flap chart. In this way any potential venous compromise (brisk capillary refill (less than two seconds) with a dusky or bluish flap and possibly increased drain output or haematoma) or arterial compromise (a pale flap with reduced or absent Doppler signal) are identified rapidly and are an indication for emergent re-exploration. When recognised early and managed promptly (within six hours), compromised flaps have a 75% salvage rate. The definitive management of a struggling or failing flap is usually surgical and patients require urgent re-exploration to inspect the vascular pedicle for kinks and compression, assess patency of the anastomosis, identify thrombus formation, perform embolectomy if appropriate, or administer intra-arterial thrombolysis.
Patients are reviewed routinely by the on call team and as required. Hourly observations are continued from the first postoperative day, as guided by the surgical team. Flap observations are continued until discharge.
While the traditional approach was for aggressive intravenous fluid therapy, our experience in free flap breast surgery suggests this is not necessary, as fluid losses are not great due to the ‘surface surgery’ nature of the procedure, and due to the proximity of the internal mammary artery to the heart, there is excellent perfusion. Fluid overload is avoided as this increases the risk of flap thrombosis and pulmonary oedema. Fluid management is initially via intravenous crystalloid fluids, although these are routinely stopped on the first postoperative day when the patient is drinking to avoid overload. Vital signs include monitoring routine clinical observations. Hourly urine output is monitored, aiming for 40-50ml/hr, approximately 0.5ml/kg/hr. Normally patient care is in intensive care recovery over night for close monitoring purposes. Patients are encouraged to drink clear fluids only during the first postoperative night. Eating and drinking a normal diet may begin the following day after surgical review.
A Bair Hugger™ air-warming device is used to maintain normothermia. This normally remains on for 24 hours postoperatively. Pain management is via a patient controlled analgesia (PCA), with regular anti-emetics being administered while on PCA, if required. The PCA is usually removed on day two with appropriate and alternative oral analgesia prescribed.
Three doses of intravenous augmentin antibiotic (depending on penicillin allergy) are routinely administered.
Routine biochemistry and haematinics (full blood count and urea and electrolytes) are taken on the night of surgery, aiming for a haemoglobin level of between 8-10g/dl. Blood transfusion is rarely required.
Patients are on bed rest for 24 hours. During this time we avoid turning these patients as this may affect the circulation to the flap. Patients should have knees bent at all times in bed and their head should be no lower than 30 to 45 degrees for the first 48 hours. Patients should not be made to lie flat when moving up the bed, with appropriate numbers of staff to assist the patient during moving, in order to reduce abdominal tension. Patients are sat out in a chair on the first day postoperatively, with chest physiotherapy to reduce atelectasis, and may be mobilised gently with the physiotherapist the following day. Flowtron® boots are removed on day one postoperatively to allow greater mobility. The urinary catheter is removed on the second postoperative day if patients are mobile enough.
Anti-embolic stockings are continued until patients are mobile. Tinzaparin is continued for one week postoperatively and two weeks for high-risk patients (including those with high body mass index and those undergoing bilateral reconstruction).
Daily outputs from drains are recorded, with a total for each 24 hours postoperatively, with the drains marked each day at 8am. Drains can come out when less than 30mls in 24 hours if the patient has been sitting out. Drains are removed at three days postoperatively unless there is persistently high output.
Patients are discharged from day three, but typically on day four or five, and slightly longer in bilateral cases.
Wound care
Micropore® tape is left in situ and patients are encouraged to shower from day four onwards. Patients are given instructions about wound care when they go home and given the number of where to call at all times in an emergency post discharge.
Patients are typically seen on day 10 post surgery in our dressing clinic, with outpatient review at two to four weeks and again at six weeks.
Recovery
Patients are advised not to drive for four weeks, or until they can perform emergency manoeuvres, and may return to work from six to 12 weeks depending on the nature of their work. Initially patients may feel some abdominal tightness but are able to stand fully upright within a few weeks. Strenuous exercise should be avoided for eight weeks to allow the abdominal donor muscle and fascia to heal fully.
Breast symmetrisation and secondary adjustments
It should be remembered that almost 90% of women have noticeable asymmetric breasts due to soft tissues or bony chest walls preoperatively. In patients undergoing breast reconstruction, this may not be noticed until they have surgery. Around a third of women want their reconstructions to match their unoperated breast. The remainder are keen to have a lift (mastopexy) or reduction on the other side. Symmetrisation may involve liposuction and fat transfer to either breast.
Most reconstructions require more than one stage and adjustments to one or both sides so it is a journey, not a single operation. If the nipple is removed the nipple can be reconstructed either by ‘sharing’ the other nipple from the other side if this is large or using the newly reconstructed breast skin with local skin flaps.
The final stage is to tattoo the nipple if requested, which can make the final result look very natural.
Conclusion
Deep inferior epigastric perforator (DIEP) free flap is considered the gold standard in free flap breast reconstruction. As the microsurgical success rates are so high using The Royal Marsden pathway the emphasis is placed on aesthetic outcome in the interests of patient satisfaction.
References
1. National Collaborating Centre for Cancer. Early and locally advanced breast cancer: Diagnosis and treatment. NICE Clinical Guideline 80. London, UK; National Institute for Health and Clinical Excellence 2009. [https://www.nice.org.uk/guidance/
cg80?unlid=30968466520158613027
Accessed 30 June 2016].
2. Gabriel SE, Woods JE, O’Fallon WME, et al. Complications leading to surgery after breast implantation. N Engl J Med 1997;336(10):677–82.
3. Allen RJ, Treece P. Deep inferior epigastric artery perforator flap for breast reconstruction. Ann Plast Surg 1994;32(1):32-8.
4. Lebo PB, Quehenberger F, Kamolz LP, Lumenta DB. The Angelina effect revisited: Exploring a media-related impact on public awareness. Cancer 2015;121(22):3959-64.
5. Nimalan N, Branford OA, Stocks G. Anaesthesia for free flap breast reconstruction. Br J Anaesth Edu 2016; 16(5):162-6.
Declaration of competing interests: None declared.
TAKE HOME MESSAGE
-
All patients undergoing mastectomy should be offered breast reconstruction.
-
The DIEP free flap is considered the gold standard in free flap breast reconstruction.
-
The DIEP free flap is a microvascular free flap using a woman’s own tissue, composed of skin and fat from the abdomen, without muscle, to recreate a breast that looks and feels natural.
-
The Royal Marsden protocol that has been developed for DIEP flap breast reconstruction provides a safe and high quality pathway and results in a flap success rate of 99.5%.
-
Most reconstructions require more than one stage and adjustments to one or both sides so it is a journey, not a single operation.
-
Once the reconstruction is complete there is no need for long-term ‘maintenance’.
COMMENTS ARE WELCOME