
What do you do when a patient refuses amputation? The author shares various cases and outlines her team’s approach to this scenario in Gaza.
What to do when a patient refuses amputation for a severely damaged lower limb that will never function normally again and be a burden to mobility? This is not an uncommon dilemma faced by orthoplastic teams in the developing world. Present and long-term care has to be formulated. An interim solution must be found if consent for amputation is initially refused but the state of the limb could threaten life.
Refusal of amputation can be for religious and cultural reasons but is also strongly influenced by patients’ knowledge that following amputation the chance of getting a quality prosthesis in their country is slim.
The following account outlines how we approach this scenario in Gaza where there is currently an epidemic of severe lower limb gunshot injuries (see An epidemic of lower limb gunshot injuries on our website).
The mindset has to evolve. Amputation must be discussed when limb salvage is attempted. Repeated ineffectual surgeries are not an option. There has to be compromise between what surgical interventions are available, advisable and affordable in the context of the country’s facilities and finances.
Method and case selection
Sound assessment by the surgeon plus clear, sympathetic communication with the patient is the key to dealing with a limb so badly damaged that amputation would give the best functional outcome. The decision for amputation relates to the degree of injury, the limitations of the medical context and level of surgical skill available. The orthoplastic team assess all limb components: the bone injury, neurovascular issues and the paucity of soft tissue options for cover. Two lower limb surgeons should review the case and the combined severity of injury to each tissue component dictate whether amputation is advised.
Should the patient refuse consent for amputation, salvage has to be considered despite the prediction of poor functional outcome. The orthoplastic team may have to modify their concept ‘of end goal of treatment’. In Europe, the goal of post-traumatic amputation is to restore function and avoid morbidity. Without consent to amputate, the goals are different. The leg is stabilised to offer the patients a reprieve: prevent sepsis, close open wounds, allow the patient a pain-free interval to consider amputation after proper support and education. Limb ‘salvage’ is not limb reconstruction. The principles of treatment involve 1) 100% debridement of necrotic bone and necrotic soft tissue, 2) stabilisation of the fracture with an external fixator, 3) soft tissue cover of exposed bone and closure of wounds. It gives the limb a last chance to heal and the patient time to consider what future function can be expected of this limb. Some have called this in Gaza ‘palliative’ limb surgery.
Within the orthoplastic team, it falls to the plastic surgeon to come up with a soft tissue cover solution. The use of local and distant donor sites must justify the outcome. Using multiple donor sites and causing donor site deficit is not justifiable for a limb that may never come to bone union or never again be weight-bearing. The patient must be left with at least ‘one good leg to stand on’, hence my reluctance for any procedure that violates a normal, contralateral leg for a limb salvage procedure. Local flap selection must not violate tissue necessary for a good amputation stump in case amputation is necessary at a later date.
Having mutually decided that salvage is to be attempted, surgeon and patient must discuss an action plan should the patient become septic. It is imperative to spend time with the patient (and an effective translator) and enter into a crucial agreement before the salvage surgery starts. Figure 1 is a summary of consent form we have made. The patient is told clearly this is the last attempt: if it fails, amputation must be considered. If sepsis occurs, it is life over limb and amputation will be the only operation possible.
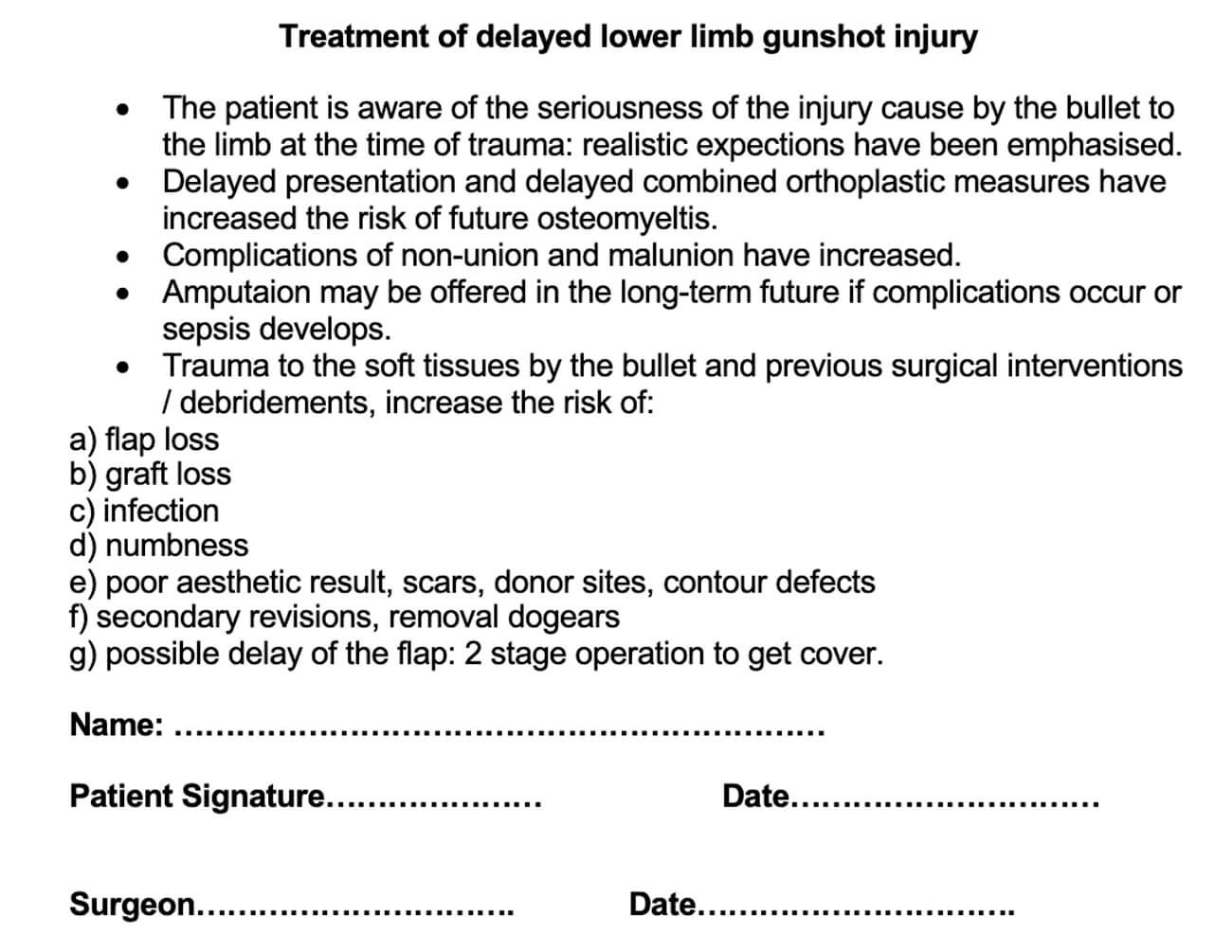
Figure 1: Record of discussion form: used to document the discussion with the
patient before limb salvage is attempted on severely traumatised limbs.
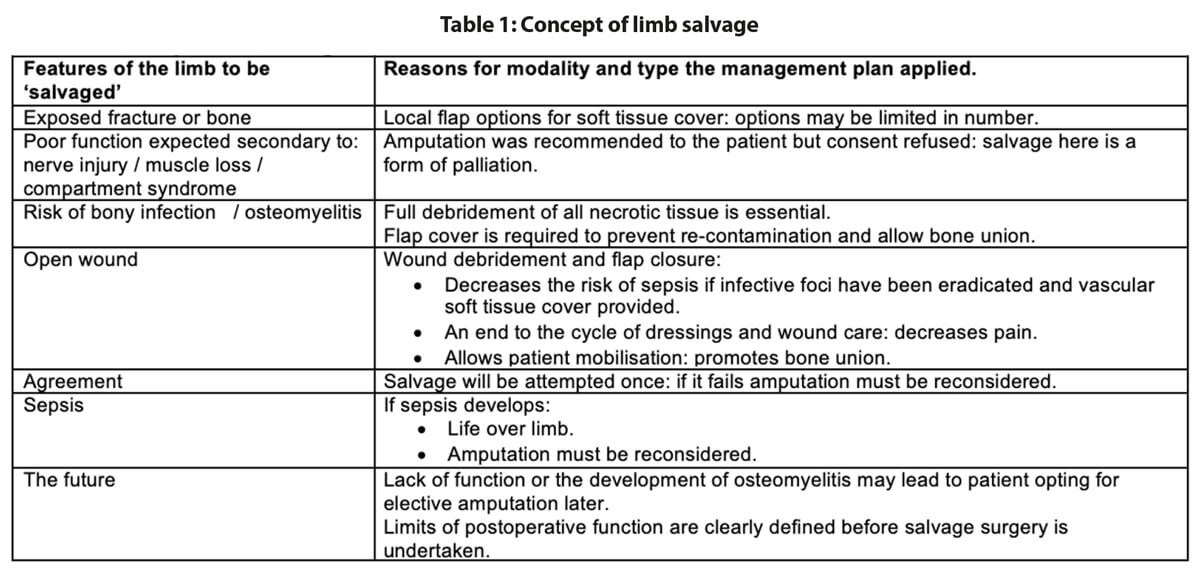
Amongst these ‘last chance legs’, several patients have presented with only one local flap option available due to the extent of local soft tissue and vascular damage. Our patients call these ‘Inshallah’ flaps (Table 1) since they are aware that should the flap fails, soft tissue cover will not be possible and amputation will be offered as a solution.
The future is also clearly outlined before surgery. The expected level of function of the limb is defined. Repeated interventions on functionless limbs will not be an option. In short, the patient’s request has been met; they will keep their limb. This may be a palliative procedure. Infectious risk from the limb has been minimised but possibly not obliterated. A limb of limited function is the predicted outcome and does not automatically qualify the patient to enter a complex reconstructive programme unless, of course, function can be improved by reconstruction.
Once the patient and surgeon agree to go ahead with limb salvage, co-operation, trust and mutual respect has to be established. Both surgeon and patients need to do their part to give the limb the best outcome possible. The patient must want to comply, elevate the leg when asked, stop smoking and engage in rehabilitation.
Case studies
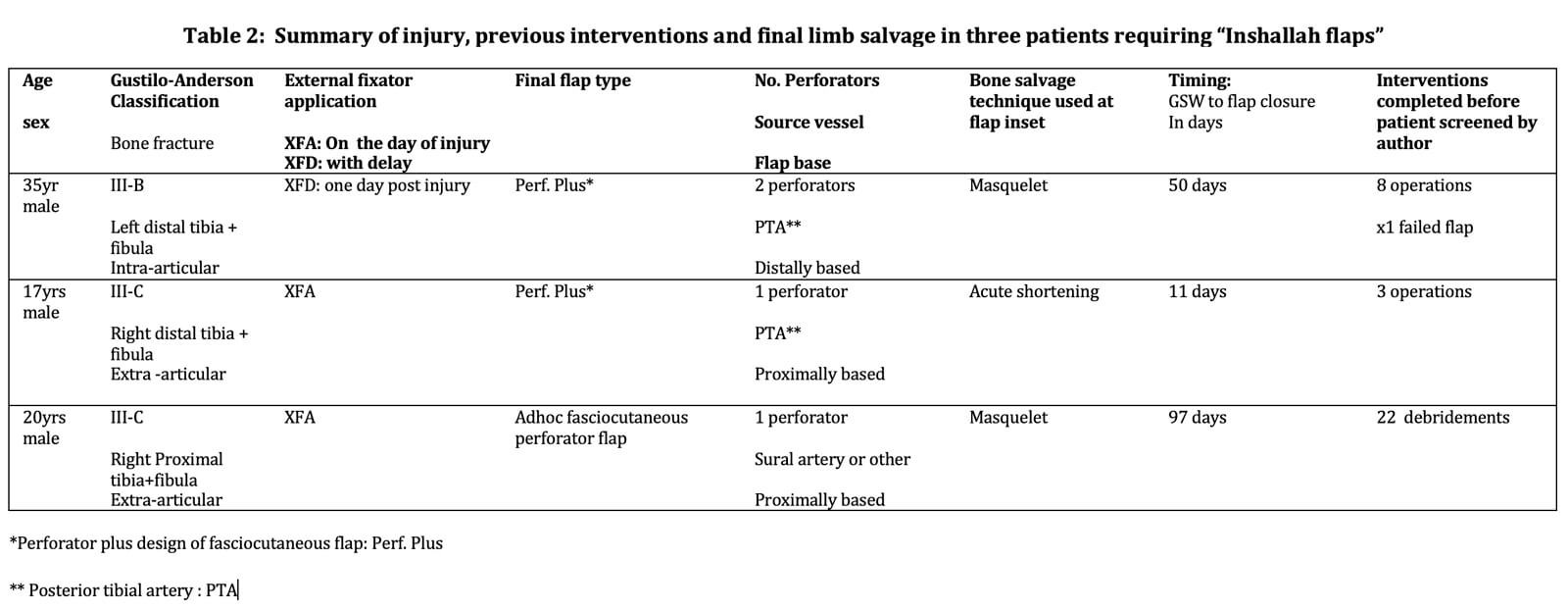
Table 2 summarises the three case histories presented. For case 1, local soft tissue was the limiting factor. In cases 2 and 3, salvage was performed because amputation was absolutely refused. All limbs are on their last chance of salvage.
The aim in all cases was total debridement, removal of bacterial contamination, to stabilise the bone, try to maximise the chances of eventual bone union and decrease the risk of osteomyelitis. Once fully debrided, wound closure prevents recontamination and cuts the endless cycle of pain and ineffectual visits to dressing clinics. In all cases bone and soft tissue were sent for culture: appropriate, specific antibiotic therapy was applied and monitored [1].
Case 1
A 35-year-old man presented to screening clinic six weeks after a gunshot wound (GSW) to the left leg (Figure 2a & b). The bullet entrance point is dorso-medially with an anterior exit causing a compound intra-articular fracture (Figure 2c).

Figure 2a: Six-week-old GSW injury to left ankle: medial small entry point.

Figure 2b: Large anterior bullet exit wound.

Figure 2c: Antero-posterior and lateral x-rays: intra-articular, comminuted fracture of the ankle joint.
The patient had received eight previous surgeries: two debridements followed by a split thickness graft (SSG) that had failed. Six weeks later, four more debridements were done followed by a peroneal muscle flap that also failed (Figure 3).

Figure 3: 10 weeks from the initial trauma, patient has had treatment elsewhere
and presents with a necrotic peroneal muscle flap.
The previous interventions narrowed any remaining flap options. Both lateral fasciocutaneous and reverse sural artery flaps were no longer possible due to damage to peroneal perforators. The external fixator had been placed through the medial flap options.
Three perforators were found on which a final ‘last chance flap’, could be raised (Figure 4a & b).
Figure 4a: Defect after flap and bone debridement.

Figure 4b: Bi-pedicled delay of a postero-medial fasciocutaneous flap:
the flap is based on three proximal posterior tibial artery perforators.
A bi-pedicled delay was used to maximise the flaps length and get full defect closure without tension [2,3]. Four days later, following regular daily washout of the bone cavity, the first stage of a Masquelet [4] procedure was done and the flap inset (Figure 5a & b).

Figure 5a: Final debridement and washout of bone:
Masquelet technique with placement of cement plug in bone defect.

Figure 5b: Proximal division of the flap, 1600 rotation, inset and closure
any remaining soft tissue defect and donor site with split skin graft.
Figure 6 shows the flap three weeks from surgery. Three months from surgery, the patient remained free of infection. He will go forward for removal of cement and bone grafting.

Figure 6: Flap and donor site at three weeks.
Case 2
A 17-year-old adolescent sustained a GSW to his right distal leg (medial entrance wound, lateral exit wound) (Figure 7). He had a Gustilo IIIc [5,6] compound fracture (Figure 8). Acutely, the posterior tibial artery was ligated, tissues debrided and an external fixator placed. Two further soft tissue debridements were performed and unfortunately, the medial wound was closed. There was total loss of function in the peroneal and posterior tibial nerves.

Figure 7: GSW to the distal third right leg: medial entrance wound and lateral exit wound.

Figure 8: X-ray right leg: Gustilo IIIc comminuted, compound fracture
of distal third tibia and fibula with bone gap.
He presented 11 days post injury, with a history of a pyrexia and foul fluid seeping from the closed medial wound (Figure 9). He was taken immediately to theatre. All wounds were opened. Devitalised tissue was obvious as soon as the medial sutures were released (Figure 10). In view of the bone, muscle and neurovascular injury, along with contamination and symptoms of infection, amputation was considered the best modality of treatment but the boy refused his consent. Complete debridement of all non-viable tissue and through washout was performed. All wounds were left open. Broad-spectrum antibiotics were commenced: bone and tissue cultures were sent. A discussion with him and his parents was organised immediately to propose amputation.

Figure 9: Foul fluid seeps from prematurely closed medial wound.

Figure 10: Removal of sutures medial wound: necrotic fat,
shredded muscle and devitalised bone fragments.
Consent for amputation was refused again. It was therefore agreed to give the limb one chance of salvage surgery. A clear understanding was given that should sepsis occur, the boy should undergo amputation. If the limb salvage were successful, the function would be poor: an insensate, shortened leg.
Acute shortening and adjustment of the external fixator was followed by the raising of a fasciocutanteous flap on a single proximal perforator. The flap rotated easily to cover the fracture site. The donor site and any remaining medial and lateral soft tissue wounds were closed using SSG (Figure 11).

Figure 11: Medial, proximally based perforator-plus flap is used to cover exposed bone after thorough
debridement, washout and bone shortening. Skin graft covers the flap donor site and lateral wound.
Three months from this salvage there were no signs of osteomyelitis yet (Figure 12). There was no motor or sensory neural recovery. Regular follow-up and monitoring continue. The surgery has afforded the patient time to consider his options whilst the full debridement prevented imminent sepsis. If the boy elects to keep this limb, the function will always be poor and not consistent with the mobility a 17-year-old should enjoy whatever reconstructive options are applied. Amputation, good rehabilitation and a good prosthesis would give him superior mobility.

Figure 12: Appearance of leg three months from salvage surgery and bone shortening.
Case 3
A 20-year-old man presented 46 days after a GSW injury to his right leg. He sustained a Gustilo IIIc fracture of the proximal tibia and fibula with division of the popliteal artery (Figures 13 & 14). The vascular defect was bridged acutely with a vein graft by a vascular surgeon. All toes were necrotic from either acute ischaemia or embolic injury. All compartments below the knee had been affected during the acute ischaemic episode. There was no neural function below the knee: the patient had an insensate foot with a pressure sore on the heel. This equated to a poor foot on an ‘almost dead’ stick.

Figure 13: Right lower leg following compound fracture and vascular injury. The sponge of a vacuum
assisted closure system is still in situ. Extension of the medial wound for access during
acute vascular repair as well as to allow extension as a medial fasciotomy.

Figure 14: Bone loss in the proximal tibial metaphysis.
The patient had been immobile for 1.5 months, he was thin and unwell but not septic yet. He had received 22 ‘debridements’ of this limb with necrotic tissue being removed from the deep and superficial posterior compartments. A vacuum dressing was in situ.
It was explained to the family and patient that the prognosis for this leg was very poor; both for function and chances of bone union. The risk of future infection and sepsis from retaining this leg was emphasised. Despite four family meetings, the young man refused amputation.
He was taken to theatre for examination under anaesthetic (EUA) and further debridement. Pus was present in the bone medullary cavity when the vacuum dressing was removed (Figure 15). The only flap option was a medial adhoc perforator flap based on a perforator proximal to the zone of arterial repair.

Figure 15: Pus found in the tibial medullary cavity on removal of the vacuum sponge.
Flap planning: a single perforator was found proximal to the vascular repair on
which a fasciocutaneous flap could be based.
Compete debridement was undertaken to eradicate septic foci. Once clean, a Masquelet type procedure and closure with the medial adhoc perforator flap was undertaken providing limb salvage (Figure 16).

Figure 16: Flap cover following thorough bone debridement and Maquelet cement plug.
Split skin graft covers the flap donor site and any remaining soft tissue defects.
The patient was discharged home 10 days later with no new signs of infection and all areas closed by flap and SSG. At three months review, he was mobile on one leg with crutches. He was well and grateful to have the time to consider his options; he could accept the functional limitations of the leg. He was considering elective amputation if he could be guaranteed a good prosthesis. One year from surgery (Figure 17), he still retains the functionless leg with no episodes of clinical osteomyelitis but minimal chances of bone union. He will have to come to his decision shortly.

Figure 17: one year post surgery.
Discussion and conclusion
The three case histories illustrate the management of three young men with severely traumatised limbs for whom amputation was not an option. In case 1, soft tissue cover was the problem: the severe GSW was compounded by iatrogenic injury and errors of planning. This emphasises the importance of humanitarian surgeons working only within their skill set and acknowledging when they should not go beyond. In an environment where microsurgery is not an option, the surgical context also becomes a limiting factor. Added together, these issues left only one potential flap option before amputation. The second two cases, both patients have two issues: imminent sepsis and long-term poor function if they survived. For these two patients, limb salvage has afforded them time to consider their options whilst the full debridement has prevented imminent sepsis.
The patient in case 1 may go onto a reconstructive programme. The patients in cases 2 and 3 have elected to keep their limbs but the function will be poor and they may request elective amputation later. All three may present with osteomyelitis in the future and so their management may further change course.
In Gaza, unless amputation can be presented as a modality of treatment, rather than a life sentence of immobility, it will never be accepted [7]. There are cultural, religious and psychological hurdles that need to be overcome. Alberto Cairo has shown us by his work in Afghanistan that the ‘impossible’ is possible if the correct approach is taken [8].
When so many patients present with limbs beyond repair in a short space of time, setting up all the necessary support following amputation is as important as concentrating on advanced plastic and orthopaedic techniques. An amputation well done, a good prosthesis and a centre for rehabilitation and prosthesis maintenance is still not universally viewed as a modality of treatment. We could be offering solutions instead of prolonging poor function and allowing the psychological decline that occurs in these young men. They continue to dream of advanced surgeries that will fully restore them to a level of mobility a young man should enjoy when this is not possible due to the primary damage sustained. We need to start on the journey of the provision of rehabilitation and a future for these young men as surgery alone is not the solution.
References
1. Staruch RMT, Hettiaratchy S. Warzone trauma and surgical infections. Surgery 2019;37:58-63.
2. Godwin Y, Righi B, Robotti E. A user’s guide to local perforator flap reconstruction in a post-conflict setting. J Plast Reconstr and Aesthet Surg 2016;69:e57-e60.
3. Godwin Y, Righi B, Robotti E. ‘Chapter 66: Local perforator flap reconstruction in the surgical mission setting’. In: Shokrollahi K, Whitaker I, Nahai F (Eds). Flaps; Practical Reconstructive Surgery New York, USA; Thieme; 2017: 698-708.
4. Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am 2010;41:27-37.
5. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 1976;58:453-8.
6. Gustilo RB, Mendoza RM, Williams DN. Problems in management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 1984;24:742-6.
7. Martinet Y, Gardette O, Ramus RA, Laporte M. Gaza une Jeunesse Estropiee. October 11 2018.
https://youtu.be/ktKrbzIX7Pc
Accessed 20 July 2019.
8. Cairo A. There are no scraps of men. TEDxRC2. November 2011.
https://www.ted.com/talks/
alberto_cairo_there_are
_no_scraps_of_men/transcript?
language=en
Accessed 20 January 2020.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME







