
As the COVID-19 pandemic continues to impact upon us all, the author, a reconstructive plastic surgeon, provides a thought-provoking account of a different type of epidemic that is having devastating consequences.
The Oxford English Dictionary defines an epidemic as “a sudden, widespread occurrence of an undesirable phenomenon” [1]. Although we are familiar with epidemics related to infectious diseases, this definition is not usually applied to the occurrence of a traumatic injury requiring surgical management.
This report covers an epidemic of lower limb gunshot wounds amongst the youth of Gaza. The author has worked with cases from the beginning of this crisis to early 2020. The injuries sustained and evolution of this epidemic are reported. Consequences, lessons learnt and possible solutions are discussed.
Clashes continue along the border between the Gaza strip and Israel. From December 2017 to the present day, gunshot wound (GSW) injuries have been sustained to lower limbs. On two specific dates (30 March and 14 May 2018) the numbers of these complex, compound fractures exceeded 500 cases in one day. This epidemic level of identical injury catastrophically overwhelmed the local hospital services and resources. Every Friday, more identical emergencies presented: GSW injuries principally to the lower leg. Since the start of this ‘lower limb crisis’ the local medical teams estimate over 7500 lower limb GSW cases. As more patients required acute care, so those from preceding weeks and those that required ongoing care entered a cohort of chronic and incompletely resolved open fractures and open wounds. Medical resources, both local and non-governmental organisations (NGOs), have struggled to meet the demand for second wave care.

Figure 1a: Example of the small entrance wound from a bullet to a posterior right thigh.
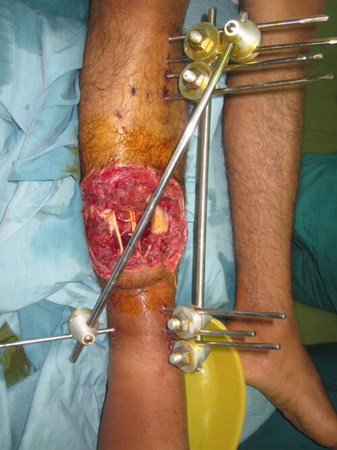
Figure 1b: Bullet exit wound anterior distal 1/3rd of right leg: No tissue is spared from injury.
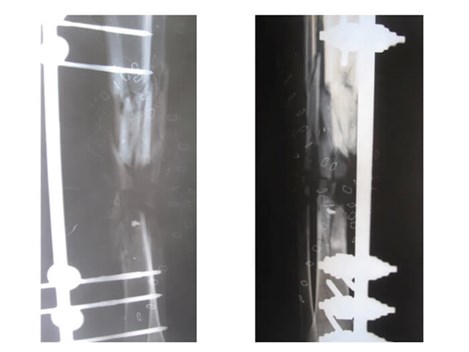
Figure 1c: Bone injury to middle 1/3rd tibia and fibula: comminution over a long segment and bone gap.
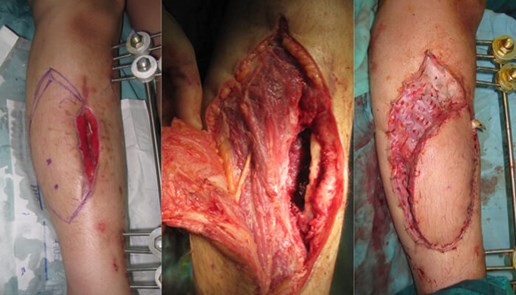
Figure 1d: Anterior compartment muscles exposed whilst raising a fasciocutaneous flap.
Muscles involved in the exit wound are found damaged and fibrosed 2.5 months after the acute GSW injury.
The nature of the injury is consistent. The bullet releases kinetic energy as it tumbles through the tissue [2]. The wounds are characterised by small entrance injuries (Figure 1a) and large exit wounds (Figure 1b). The bullet exits the limb during the cavitation phase and no tissues are spared. Open, fragmented fractures, often with a bone gap, result (Figure 1c). All soft tissues are damaged. Muscle may be viable but is often shredded (Figure 1d). Nerve damage involves division, segmental loss and nerve gap. Vascular injury is associated with vessel division. The outcome of major vessel division is entirely dependent on speed of care: national emergency teams and vascular teams are expert in this. However, with epidemic number of patients presenting, ischaemic injury, compartment syndrome and loss of life have occurred. The delivery of acute treatment is only as rapid and optimal as the local resources that can be provided. It is to be emphasised that local, national surgeons and medical teams did excellent work under the strain of acute, weekly mass casualty incidents. Patient numbers outstripped the capacity of trained local specialists. This article concerns the complications of that delayed second wave response. Click here to access the data on which this article is based.

Figure 2a.

Figure 2b.

Figure 2c.
Figure 2a-c: Success story of patient treated by local surgeons: orthoplastic collaboration in country.
2a: 19-year-old male with a Gustilo IIIb middle 1/3rd tibia and fibular fracture, left leg
2b: Treated acutely with debridement and external fixator: x-ray at 2.5 months shows good alignment and signs of union.
2c: Fracture site was covered by a local fasciocutaneous flap within 11 days of the acute injury
Development of the ‘second wave’ cohort
Cases were screened and many had received timely orthoplastic care with excellent outcomes (Figure 2a-c). The local teams should be applauded that 70% of the open fractures received immediate, acute debridement and placement of an external fixator. The remaining 30%, with less serious open fractures, all received debridement and a fixator within three days of the injury. Forty percent of the fractures seen at screening needed no further orthopaedic intervention and 50% did not need plastic surgery interventions. Local education programmes clearly provide the best overseas aid possible. A UK teaching charity has supported local orthopaedic surgeons with training in limb reconstruction since 2009. This capacity building prior to this crisis saved many limbs.
Thirty percent of the cohort had less than ideal post-acute (or second wave) care. With time progression, the state of these young men deteriorated and their chances of limb salvage with good long-term outcome decreased. Reflection on the data, as well as personal experience in the field for over two years, allows comment on the underlying factors that have led to the development of neglected, chronic open wounds in second wave patients. Factors contributing to the development of this cohort can be arranged chronologically into acute, semi-acute and long-term. Delay in full debridement and definitive soft tissue closure has been the most detrimental factor.
Acute factors
1) The primary cause of the crisis has been large number of acute casualties. Such recurrent major incidents, with all cases presenting with the same injury in a matter of hours, is unprecedented. Manpower and resources could not match this influx. Any hospital in any country would struggle to treat 500 open lower limb injuries in one day. Unique to this situation is that all the patients needed the same medical expertise and same surgical kit: a true epidemic of the same injury.
2) Basic principles around war surgery could not always be followed due to circumstance [2-5]. On days where mass casualties were admitted, the principle of acute wound debridement and a second look at 24 hours was not always possible. Twenty-four hours of operating time was insufficient to clear the daily intake of new cases. Victims of the previous day could not be returned to theatre for a timely second look. Due to pressure of time and numbers, occasionally tissues were primarily closed that would have benefitted from a second look, further debridement and delayed closure.
3) Acute triage and management planning of the severely injured limb. Orthoplastic trauma teams normally have the luxury of time and resources to assess then formulate a definitive surgical management plan. Patient-centred discussion of risks and benefits of retaining a mangled limb versus amputation can take place. In Gaza, during episodes of mass casualties, local surgeons had to act alone, doing the best they could to stem bleeding, debride and immobilise. All available surgical manpower was required: vascular, general and orthopaedic colleagues using every operating room available. Combined cases were not possible. For the patient refusing to give consent to acute amputation, there was no time for a carefully reasoned discussion with the patient and family. This resulted in some limbs being salvaged that in the long-term would have poor functional prognosis. The luxury of a multidisciplinary team was simply not possible in the acute moment.
Semi-acute / long-term factors
1) Refusal of amputation by patients: Patients have refused amputation even when it has been made clear this is life-saving treatment. The author has seen two young men die from their decision to refuse amputation despite their orthopaedic surgeon’s advice. This type of high velocity ballistic injury, with extensive tissue damage, is new to this population. Patients have not grasped yet the reality of the degree of injury and the subsequent non-functionality of the limbs they ask to keep at all cost: even above life. Surgeons cannot act without consent and so some very poor-quality limbs have been ‘palliated’ to prevent loss of life.
2) Delay in the provision of timely, secondary lower limb salvage procedures: The pool of post-acute cases requiring further specialist orthoplastic management increased in size weekly. Hospital wards filled and the number of complex compound fractures exceeded the capacity of orthoplastic teams available. As a result, patients received conservative management in the form of regular dressings on open fractures instead of secondary surgical interventions.
Current state of the second wave patient cohort and possible solutions
A minority of 30% of the originally injured young males have chronic, neglected open fractures receiving variable inpatient or outpatient care. Their injury severity is compounded by the complications of delayed second wave care; failed previous interventions; contamination and infection.
Suggested actions below could have helped advance the care of these complex cases.
1) A Shared database
An accurate, clinical database would serve to map the clinical needs of this large and complex cohort. Once the complexity of the injury is understood the correct resources can be mobilised to meet the challenges of second wave surgery.
The data must be available to all parties invited to help in order to avoid duplication of care and strategise the use of resources and skill sets. International aid must be collaborative and not individualistic so that all resources brought to the field can be channelled to maximum effect for patient care. Specialist orthoplastic teams are not widely available. Logistics and manpower can be shared between NGOs to bring the correct surgeons to the field and optimise surgical outcome.
2) Individualised patient management plans: recorded and shared
Time has lapsed between primary injury and ongoing management. At the time of meeting the patient, clinical options for management may not be straightforward. Many factors will have influenced the patient’s course to date: The severity of the primary injury, evolution of the wound, surgical interventions to date and cultural beliefs relating to context influence patients’ decisions. Surgeons and patients have to decide together a way forward to prevent, or irradiate infection, but also maintain or improve function. Surgeons may have to guide and understand a patient who places more importance on form than function and together they adapt accordingly. Decision making and discussion is facilitated when previously agreed management plans are recorded and available to subsequent clinicians who become involved in the patient’s care [6-8].
This becomes especially important when limbs cannot be returned to function but have been stabilised as a form of palliation. The goal of palliation may be to allow the patient an infection-free time to consider the option of amputation. The addition of management plans and previous surgeries to an accessible database can prevent repetition of failed treatments or initiation of unsuitable care. Outcomes can also be recorded for evaluation on the same database.
3) Shared learning
Specialist local orthoplastic teams have evolved in Gaza as a result of this crisis. Ongoing support and resources will be necessary initially from the international community. However, this is a two-way street and the international community also have much to learn. This cohort of young patients will evolve for the next 40 years with changing medical needs. Local orthoplastic teams will continue their follow-up and medical support. Our orthoplastic colleagues in Gaza will be able to teach us how to holistically manage reconstructed limbs and amputees over the long-term as long as data is recorded accurately.
4) Support for the potential amputee: make amputation a modality of treatment and not a life sentence.
Refusal of amputations, both acutely and in the chronic phase, is the biggest hurdle in management of the most severely damaged legs. Unfortunately, a bitter ‘reality pill’ has to be embraced by both patients and medical teams: some injuries just can’t be fixed. Keeping a functionless leg that is also an infective focus is becoming a reality for some refusing amputation. Focus on amputation as a treatment modality rather than an end-stage procedure is imperative in order to go forward with this cohort.
Although cultural issues are blamed for turning the patients strongly against amputation, two main reasons become evident if time is spent talking to the young men. Firstly, they fear they will never be provided with an adequate, modern prosthesis to walk well on [9]. Secondly, patients are not aware of the gravity of the initial trauma and the poor functional outcome they will get by retaining the limb. They believe their legs can be saved by surgery irrespective of the tissue loss. Patients tend to move between NGOs rather than accept amputation. This is a reason why patients’ notes need to be centralised and available to all medical teams. If duplication of care can be avoided, precious medical funds and time can be channelled to better use.
Urgent education and support concerning amputation is needed. Patients’ minds as well as their limbs require support before this modality of care is accepted. Endorsement and support from local religious, cultural and family leaders needs mobilising. Professional psychological support is imperative: many NGOs have a great track record in supplying this vital element. These young men need mentors to show them the advantages of a good prosthesis versus retaining a functionless limb. A patient support group of amputee mentors with good mobility despite limb loss, could give preoperative visits, postoperative support and allow inclusion [10]. From the technical and medical side, we need to deliver a quality amputation service with a multidisciplinary team approach and a rehabilitation centre: limb fitting unit, a workshop, prosthetist, physiotherapist, orthoplastic team for stump revisions and neuroma care, and a psychologist. This is a young cohort. If they accept an amputation, they will need sustained support into the future.
Reflections on this crisis and lessons learnt
‘Time and the timing’ have been critical factors in dictating the path of this epidemic. Firstly, mass casualties presented in a short time frame. The rapid course of events influenced the availability of care, the number of lower limb specialists and specific kit available for very specific injuries. Finally, the time delay to deliver second wave support influenced long-term patient outcome. Cases of non-union and osteomyelitis are presenting amongst cases of delayed wound closure.
The nature of conflict is changing globally: severe injuries are imparted that maim. The medical response to such events needs to change; trauma surgeons address the acute phase followed by a timely second wave of specialist support. The primary surgery will dictate if life and limb can be saved but the secondary surgery will dictate the function and influence the patients’ way of life thereafter.
Planning second wave surgery will be a considerable challenge to international organisations sending aid: the availability of suitable specialist staff and the cost and quality of care must be considered. The data illustrates the complex nature of these lower limb injuries but also that timely second wave response could have reduced morbidity hence overall suffering and cost.
The aftershock of this lower limb trauma epidemic cannot be avoided. Local surgical manpower and resources have become exhausted as all their energy has been diverted to trying to reduce this sizeable cohort. Other elective surgical work is on hold but will need addressing.
Another global problem has been aggravated during this crisis: antibiotic resistance. Had second wave surgical support arrived earlier, debridement and wound closure would have much reduced the overuse of antibiotics. Accurate microbiology support and antibiotic stewardship were unfortunately applied late with the associated development of antibiotic resistance within this closed community.
As predicted, the crisis is moving into the next challenging phase where 20-30% of the cohort need decisions made as to the long-term fate of their retained limb. The most challenging patients within this group are those with osteomyelitis from multi-resistant bacteria and those who have retained functionless limbs that cannot be improved by reconstructive surgery. For this group we need to enhance the support and education related to amputation. To be mobile, functional members of society, these young men and adolescents will need prosthetic unit support for the next 40 years at least.
References
1. Lexico powered by Oxford.
https://en.oxforddictionaries.com/
definition/epidemic
Accessed 20 January 2020.
2. Giannou C, Baldan M. War Surgery (Volume 1). Geneva, Switzerland; International Committee of the Red Cross; 2010.
3. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am 1976;58:453-8.
4. Gustilo RB, Mendoza RM, Williams DN. Problems in management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 1984;24:742-6.
5. Giannou C, Baldan M, A Molde. War Surgery (Volume 2). Geneva, Switzerland; International Committee of the Red Cross; 2013.
6. Masquelet AC, Begue T. The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am 2010;41:27-37.
7. Karger C, Kishi T, Schneider L, et al. Treatment of posttraumatic bone defects by the induced membrane technique. Orthopaedics & Traumatology: Surgery & Research 2012;98:97-102.
8. Rigal S, Merloz P, Le Nen D, et al. Bone transport techniques in posttraumatic bone defect. Orthopaedics & Traumatology: Surgery & Research 2012;98:103-8.
9. Martinet Y, Gardette O, Ramus RA, Laporte M. Gaza une Jeunesse Estropiee. October 11 2018.
https://youtu.be/ktKrbzIX7Pc
Accessed 20 January 2020.
8. Cairo A. There are no scraps of men. TEDxRC2. November 2011.
https://www.ted.com/talks/alberto
_cairo_there_are_no_scraps_of_men/
transcript?language=en
Accessed 20 January 2020.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






