The complex biological process of facial ageing engenders many structural changes that are influenced by the combined effects of gravity, bone resorption, soft tissue atrophy, displacement of fat and a complex synergy of textural skin changes [1]. One of the most important and integral parts of the upper face is the temporal region; however, this is an area consistently overlooked, neglected and under appreciated by both patient and practitioner. Loss of volume in the temporal region can have a profound effect on facial appearance; patients are often described as looking gaunt, wasted or skeletonised [2].
Therefore, after careful examination, consideration should be given to temporal volume restoration when performing a global assessment of the face for loss of volume. However, the safety of this procedure is still under scrutiny owing to severe complications reported in the literature [3]. Injecting in the temporal region is considered by many practitioners to be a high risk procedure and the temple to be ‘treacherous territory’. Vascular occlusion post dermal filler is without doubt under reported [4] and reports of catastrophic iatrogenic blindness are increasing worldwide [5].
The purpose of this article is to highlight the anatomy and physiology of the temple, raise awareness of the anatomical structures to consider and respect when injecting in the temporal region, and discuss the author’s experience of injecting with a hyaluronic acid (HA) based dermal filler using a supraperiosteal small bolus injection technique to the superior temple region to achieve a safer temporal augmentation. The content of this article is based predominantly around the opinion of the author who is a recognised and respected medical aesthetic practitioner in the UK with over 20 clinical peer reviewed papers published.
Anatomy and physiology of the temporal region
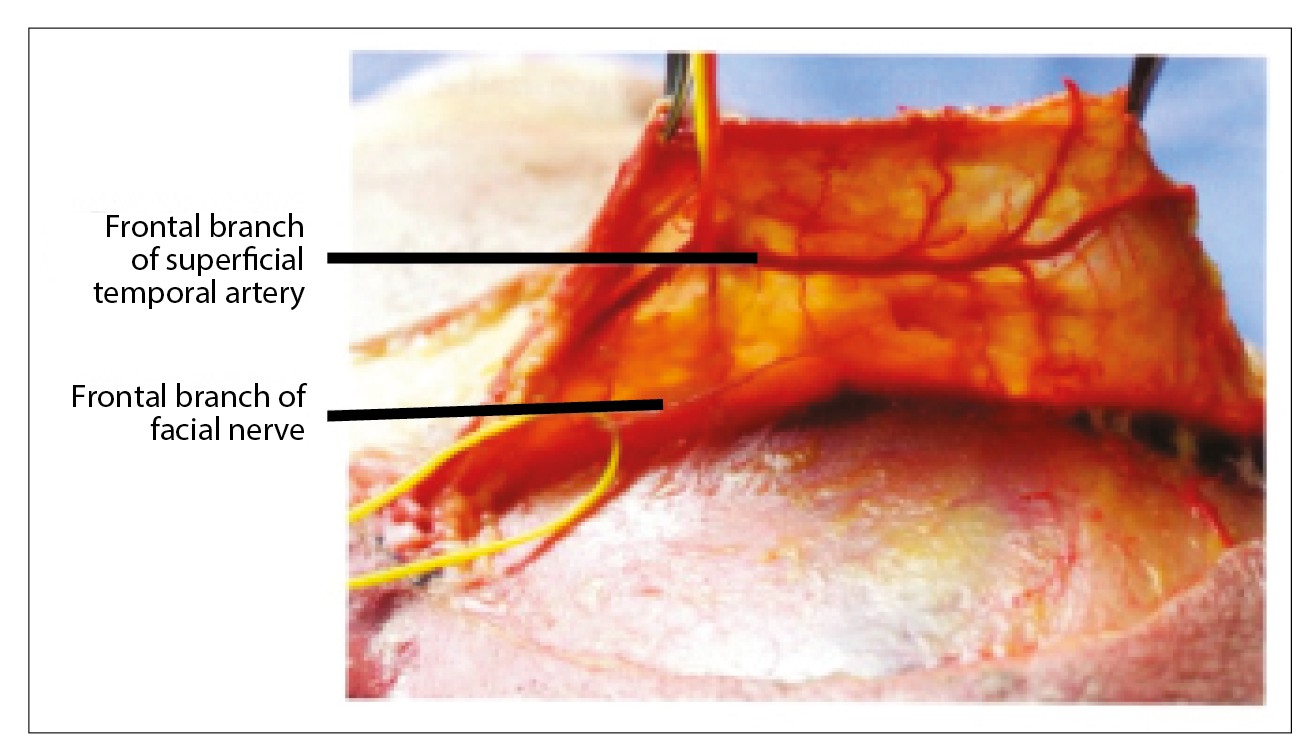
It is essential that practitioners have a clear understanding of the relationship between the temple structures and the boundaries of the temporal fossa to enhance safety when injecting in this region. Practitioners need to put tissue planes in the temporal region into context to be able to understand and appreciate the minute depths between each layer. The temporal fossa is a shallow depression on the side of the skull bounded by the temporal lines and terminates below the level of the zygomatic arch. The anatomical journey through the temporal fossa region begins with the layers of skin, followed by subcutaneous fat, which is loosely adherent to the superficial temperopariatal fascia (STPF) where both the superficial temporal artery and the temporal branch of the facial nerve are located (Figure 1). This is a treacherous area to be with a sharp needle. Loose areolar tissue precedes the temporalis muscle fascia and the middle temporal artery followed by the large temporalis muscle, progressing on to the deep temperopariatal fascia (DTPF), the deep temporal artery and terminating at the pericranium and bone. There are many considerations to be made by the injector as the needle or cannula passes through each of these territories (Figure 2).
Figure 1: Superficial tempoparietal fascia. Pessa JA, Rodrich RJ.
Facial Topography: Clinical Anatomy of the Face. CRC Press; 2012.
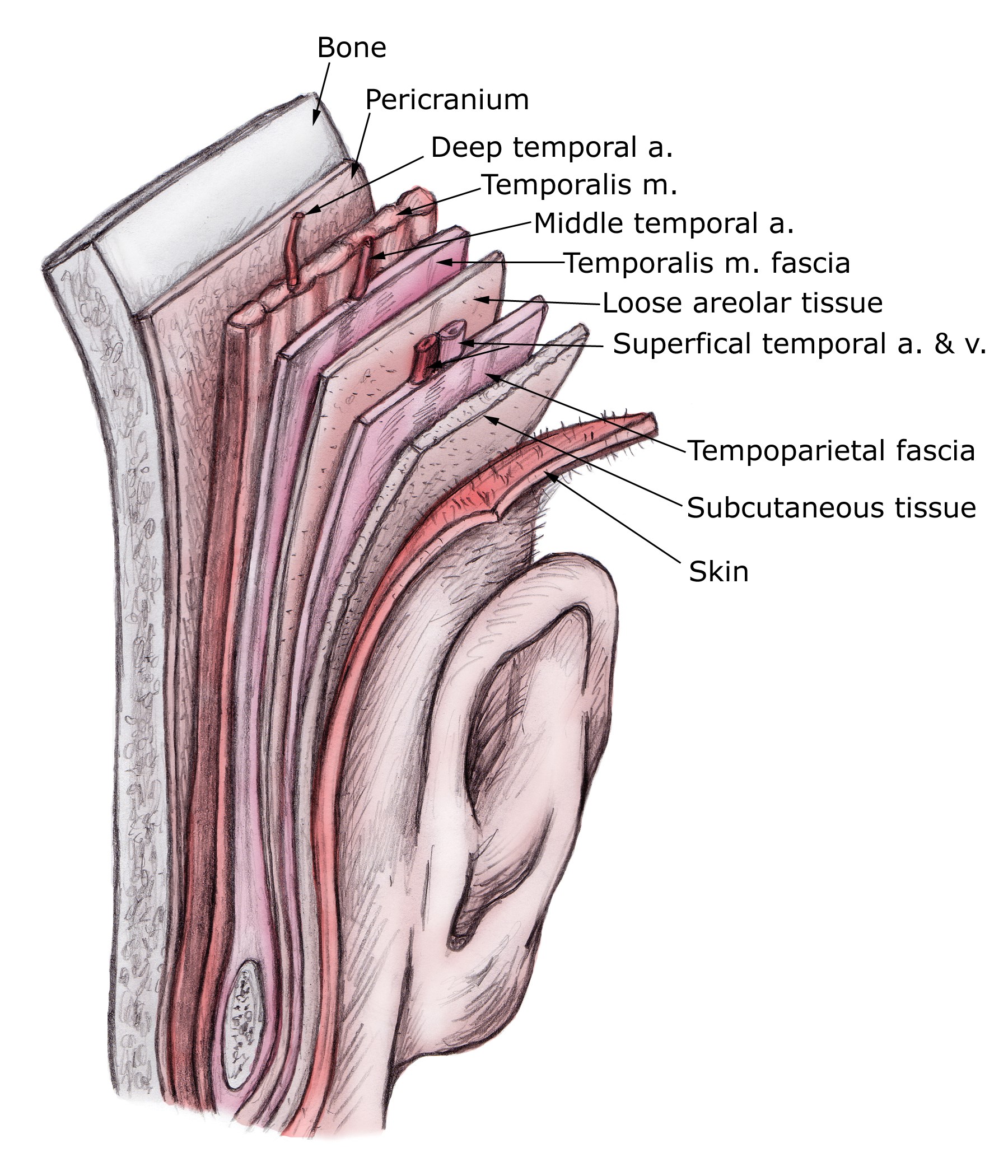
Figure 2: The temporoparietal fascia flap.
Product selection
The benefits, longevity and details of the techniques of autologous fat injections to the temples are well established [6]. However, there are cases reported in the literature of iatrogenic blindness follwing dermal filler procedures; autologous fat transfer has the highest incidence, yielding significantly worse outcomes and with a worse prognosis than other materials [5,7,8].
The author surmises that the globular nature of fat in comparison to HA decreases the potential to resolve an embolus in the event of a vascular compromise. This opinion is based on the incidence of embolic events in the literature being much higher with fat transfer than HA dermal filler. Additionally, we can use hyaluronidase to break down an embolus of HA in a vessel but it is more challenging to break down globular fat in a vessel. Furthermore, there have been three cases reported in the literature about a newly identified potentially fatal complication that has been seen post temporal augmentation with autologous fat. The complication is described as a non-thrombotic pulmonary embolism, which manifests as acute respiratory failure and has proved to be fatal in one of the reported cases [3]. Although there are other products of choice to consider, such as poly L lactic acid and calcium hydroxylapatite, the author’s preference when performing temporal restoration is Belotero® Volume with Lidocaine, which is a HA-based gel, completely homogenous with low viscosity but high cohesivity and elasticity and moreover, reversible. Loss of temporal support to the lateral brow, coupled with loss of fullness in the upper eyelid, create the impression of brow ptosis, with the eyebrow seemingly descending to a position at or below the superior orbital rim [1]. The technique involves restoration of temple harmony and balance with injection of the superior aspect of the temple with a concomitant lift of the lateral brow.
Cannula
Treating the temporal region with a blunt cannula is currently on a rising trend. The benefit of injecting with a cannula is the reduced risk of an intravascular event whilst working at a more superficial depth. There is also the potential to require less product to achieve a correction of the concavity. The STPF is thin but fairly strong (it is a structure not likely to be penetrated accidently) and it requires significant force to breach the tissue. Some practitioners prefer to inject onto the STPF with product and massage to create a smooth surface. Product selection is key if working at this depth to avoid the creation of contour irregularities. It is crucial to be aware of the superficial temporal artery and vein and the temporal branch of the facial nerve, each located at this depth. Some practitioners prefer to penetrate the STPF with a cannula and inject product between the STPF and the DTPF. Respect must be given to the middle temporal vessels at this depth. There is the potential for significant anatomical variations in the pathway of temporal vessels, therefore caution is always advised. If the concavity is severe, placement of product deeper in the fossa may be required first before completing the restoration with cannula work in the more superficial planes. The depression created by temporal wasting in the female face does not usually require a full correction; the concavity should typically be improved, however the creation of convexity may produce a negative and rather masculine feature. Hence disrupting the natural female facial silhouette. The author considers injecting with a sharp needle at the level of the STPF and the DTPF as a higher risk procedure and would advocate adopting a cannula approach in each of these planes.
Figure 3: There is no physical barrier present sub muscularly at the
inferior boundary of the temporal fossa.© Dr Samuel Webster
Supraperiosteal small bolus injection technique to the superior temple
Anatomically there is no physical barrier present sub muscularly at the inferior boundary of the temporal fossa and similarly under the DTPF (Figure 3).
The implications of these findings are that there is the potential for inferior migration of product into the premasseteric space beneath the zygomatic arch if injections are placed deep sub muscularly. However, with the cohesivity of the new generation HA products available, migration of product is becoming less prevalent. The author’s rationale for a superior temporal approach is to avoid injecting into the central depression of the deep cavity of the temporal fossa, where the passage of a needle would encounter several treacherous landmarks (as described previously in the article). Injecting superiorly can reduce the risk of embolic phenomenon, as discussed by leading experts in the field at recent conferences.
The procedure
The temporal fusion lines are a visible and palpable zone of fixation that separates the frontalis muscle and the temporalis muscle. The correct point for the superior temporal injection is identified by marking 1cm above the brow on the temporal fusion line and 1cm lateral to this point. There is very little depth to this injection technique and bone will be felt by the tip of the needle almost immediately. In comparison, when injecting into the central depression of the temporal fossa it feels completely different as the needle passes through a very deep space. Many practitioners are of the opinion that if a needle is touching bone, then it can be considered a safe place to inject. However, the author advocates aspirating at every possible opportunity when injecting in any region of the face. Although aspirating may not eliminate the risk of a vascular event, it is the consensus of opinion amongst experts that it is better to aspirate than not to [9]. Practitioners have a duty of care to patients and must do all that they can to minimise risks. A protective finger is placed anterior to the hairline to prevent the injected product from tracking laterally. The rationale behind superior temple injection is to allow the dermal filler to flood downwards into the tissue and to fill the cavity from above rather than injecting directly into it. The author’s preference is to inject no more than 0.5ml bilaterally at this first appointment, believing that adopting a sessional approach is safer practice. There is growing research to support that it is safer to inject small aliquots of 0.1ml at each injection point, redirect the needle without withdrawing, aspirate, then inject again, rather than depositing larger volumes / boluses in fewer injection sites [10]. Furthermore, recent findings have identified that in the event of injecting directly into a vessel, the outcome is far more likely to be favourable with immediate intervention than had a large bolus of product been injected causing an embolic event [10]. These findings are widely supported [7,8]. Experts advise that low pressure injections with the release of the least amount of substance possible should be considered safer than larger bolus injections [7,10]. Respecting these recommendations could avoid a serious vascular compromise.
Serious complications
There is now heightened awareness of the possibility of iatrogenic blindness following facial cosmetic injections. The literature describes around 60 cases globally [5,7,8]. It is highly probable that this number will continue to increase. There are currently four documented cases of blindness post temporal augmentation, one discussed by Lazzeri, a case from Thailand, whereby blindness resulted after the injection of silicone into the temple region [7]. The second case was reported in the UK, whereby an injection of poly L lactic acid into the temporal region resulted in unilateral iatrogenic blindness and two further reports from China when autologous fat was injected into the temporal fossa [5]. To date there has been no safe, feasible and reliable treatment for iatrogenic retinal embolism, however, immediate treatment should be directed to lowering intraocular pressure to dislodge the embolus into more peripheral vessels of the retinal circulation, increasing retinal perfusion and oxygen to hypoxic tissue [7]. A recent paper discussed the use of hyaluronidase medication as an emergency treatment of retinal artery occlusion (RAO) caused by HA filler [11]. The cadaver study discusses a potentially reliable access route for hyaluronidase medication to be injected into the ophthalmic artery to salvage central retinal occlusion post HA filler [11]. The findings support that a transorbital approach is more practical than a supraorbital approach for retrograde cannulation of the ophthalmic artery with hyaluronidase medication. The literature proposes that RAO post dermal filler results from a retrograde embolic mechanism, whereby arterial displacement of the injected product from the peripheral vessels into the ophthalmic arterial system blocks the ophthalmic artery and central retinal artery when the subsequent anterior movement of the injected product begins [7,8,10]. The author would advocate that in the event of a potential RAO that an immediate emergency referral is made to an ophthalmologist. Despite early findings being optimistic regarding the use of hyaluronidase medication in the event of RAO, further research is crucial in this area to provide a more robust evidence base on the safest route of administration. Hyaluronidase medication must not be injected directly into the globe (listed as a contraindication in the British National Formulary and MIMS)[11].
Conclusion
Loss of volume in the temporal region is consistently overlooked, neglected and under appreciated by both patient and practitioner. Temporal restoration with dermal filler can have an extremely positive and rejuvenating treatment outcome. Although it is an area deserving of respect and consideration by the injector, it is no more challenging than any other area of the face. The author advocates that there is no safe area and no safe depth, just safer practice to reduce risks. A sound anatomical understanding of the region is key to minimising patient risk. Research strongly advocates that when treating the temporal region the practitioner aspirates before injecting, injects only/Users/creative5/Desktop/EYE NEWS web content small aliquots of 0.1ml then redirects the needle, injects slowly and with minimum pressure with a small gauge needle [7]. As outlined the use of blunt cannula (25G or 27G is appropriate in the region) can be adopted to enhance patient safety and outcome [1]. Practitioners should be appropriately experienced to perform the procedure of temporal augmentation and have a sound understanding of how to respond in the event of a vascular compromise. Following this stepwise approach to performing temporal augmentation will minimise the risks of complications. Adopting a superior temple, supraperiosteal approach to injecting may further enhance patient safety.
References
1. Coleman S, Grover R. The anatomy of the ageing face: volume loss and changes in 3-dimensional topography. Aesthet Surg J 2006;26(Suppl):S4-9.
2. Moradi A, Shirazi A, Perez V. A guide to temporal fossa augmentation with small gel particle hyaluronic acid dermal filler. J Drugs Dermatol 2011;10(6):673-6.
3. Jiang X, Liu D, Chen B. Middle temporal vein: a fatal hazard in injection cosmetic surgery for temple augmentation. JAMA Facial Plast Surg 2014;16(3):227-9.
4. Coleman S. Avoidance of arterial occlusion from injection of soft tissue fillers. Aesthet Surg J 2002;22:555-7.
5. Yanyun C, Wenying W, Jipeng Li, et al. Fundus artery occlusion caused by cosmetic facial injections. Chinese Medical Journal 2014;127(8):1434-7.
6. Newman J. Review of soft tissue augmentation in the face. Clinic Cosmet Invest Dermatol 2009;2:141-50.
7. Lazzeri D, Agostini T, Figus M, et al. Blindness following cosmetic injections of the face. Plast Reconstr Surg 2012;129:995-1012.
8. Park SW, Woo SJ, Park KH, et al. Iatrogenic retinal artery occlusion caused by cosmetic facial filler injections. Am J Ophthalmol 2012;154:653-62.
9. de Maio M, Rzany B. Injectable Fillers in Aesthetic Medicine. Berlin, Germany, Springer; 2014:75.
10. DeLorenzi C. Complications of injectable fillers, Part 2: Vascular complications. Aesthet Surg J 2014;34(4):584-600.
11. Tansatit T, Apinuntrum P, Phetudom T. An anatomic basis for treatment of retinal artery occlusions caused by hyaluronic acid injections: a cadaveric study. Aesthet Plast Surg 2014;38:1131-7.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME