Countries along the coast of West Africa are amongst the poorest in the world. Extreme levels of poverty often lead to poor outcomes or fatalities in many medical conditions that would be eminently treatable, with good outcomes in more developed parts of the world.
Liberia, Guinea and Sierra Leone are amongst the poorest of these West Africa countries with no more than one doctor for every 30,000 people (compared with the UK: 1 in 400) and one in five children do not live past five years of age. Basic health care in the capitals or major cities is a luxury and it is non-existent in rural areas. In these sub-Saharan countries, land-based transport systems are not reliable, if in place at all, but most of them have port cities, which allows the delivery of world-class surgical missions via the charity Mercy Ships, an international Christian charity which brings world-class medical assistance and long-term sustainable development to some of the world’s poorest regions, through hospital ships and land-based programmes.
The current Mercy Ships vessel is the Africa Mercy (Figure 1), converted from a Danish rail ferry and deployed in 2007. It is the world’s largest non-governmental hospital ship, with five modern operating theatres, x-ray facilities including computed tomography (CT) scanner and cone beam CT, a pharmacy and laboratory. There is capacity for 82 in-patients with five wards and a small three-bed intensive care unit, as well as accommodation for 450 volunteers.

Figure 1: The Africa Mercy.
Logistics of a Mercy Ships mission
Screening
For several weeks leading up to the arrival of the Africa Mercy, details of the free surgeries available on the ship are spread to the people of the respective countries by radio, printed leaflets and word of mouth. To allow for the generally low levels of literacy, the printed leaflets are primarily photographs of the type of conditions the ship can treat while radio announcements are used to verbally explain the conditions.
More than 7000 people turned up to this year’s Screening Day in the Republic of Congo at the port of Brazzavile. This is the day when the ship first arrives and screening usually takes place in a football stadium or a large governmental building. Despite the huge number of people, the system of screening is very efficient and people will wait very patiently for their turn to be seen. Initially, nurses walk the line to primarily bring out any urgent cases (where someone is having severe breathing difficulties because of their tumour, for example) but also to do the very difficult job of turning away the many people who have turned up with conditions the ship cannot treat.
Patients triaged by the experienced nursing staff will be invited to go through registration and consultation by the surgical teams, including history-taking and clinical examination followed by appropriate investigations such as ultrasound and fine needle aspiration cytology. During screening, surgeons, radiologists and histopathologists assist in clinical assessment and booking dock-side pre-admission clinics and a date for surgery on the ship for appropriate patients.
Patient selection
One of the policy decisions with the missions has been to refrain from offering cancer surgery. This is due to the lack of basic health care in the communities from which the patients generally come and also the lack of local health care professionals such as doctors, dentists, pharmacists and midwives. There is no provision for the continuing care of patients with radiotherapy, chemotherapy or other modes of adjuvant therapy after surgery. There is one exception, however, and that is for patients with suspected Burkitt’s lymphoma.
This is a cancer of the lymphatic system that was first described in 1958 by Dennis Burkitt, an Irish surgeon who worked in equatorial Africa. A common presentation is a tumour of the jaw found in children. The diagnosis can be made using an on-board Coolscope®, a real time telepathology system that allows instant diagnosis of fine needle aspirate cytology by a volunteer histopathologist in the UK thousands of miles from the ship.
Notwithstanding the limitation of cancer surgery, there are many life-transforming and indeed, life-saving surgeries performed on the Africa Mercy. Such procedures range from simple cataract surgery to complex facial reconstructions; from the release of post-burn contractures to the correction of obstetric related fistulas. Both acquired and congenital orthopaedic problems are also treated.
Benign conditions of the head and neck region can develop into extensive tumours, causing not only grotesque deformities but also functional disabilities, ranging from dysphagia, dysarthria and dyspnoea with a slow lingering death caused by airway obstruction. Additionally, people with these kinds of conditions are often completely ostracised by their family and friends, with many only able to venture out in the dark to forage for food. These conditions can also be treated on board. The following are a selection of cases, which illustrate some of the surgical services offered.
Paediatric benign maxillary tumour (Figures 2a-b)
Nine-year-old Edoh had an extensive ameloblastoma, a rare, benign, tumour of her left maxilla which displaced her left eye and stretched her lip. She became malnourished due to difficulty in eating and the relentless growth of the tumour threatened a slow and horrible death from suffocation. Edoh’s parents, having exhausted every possible avenue of hope, finally gave up and prepared for her death.

Figure 2a: Edoh, before surgery, being examined by Gary Parker and Lou Koeper.

Figure 2b: Edoh after her facial surgery.
Edoh came to the screening day with more than 3000 other hopeful patients and their carers. As the crowd saw the desperate need of Edoh, who was now severely breathless with blood coming from the stretched and inflamed mucosa of her mouth, there was an instinctive outpouring of compassion. She was lifted up, passed hand to hand and tossed, screaming, over a steel gate. She landed in the arms of a Mercy Ships volunteer.
The Chief Medical Officer and Maxillofacial Surgeon, Gary Parker, performed an emergency tracheostomy for her upper airway obstruction under local anaesthetic before the resection of her extensive maxillary tumour.
Edoh returned to the Africa Mercy for minor reconstructive surgery to her left lower eyelid and cheek. As she had met many selfless and caring health professionals on the ship, Edoh is now training to become a nurse so that she can give back what has been given to her.
Goitre (Figures 3a-b)
Extensive multi-nodular goitres are not uncommon in West Africa due to the lack of access to health care. Many goitres are already causing compressive symptoms before patients seek medical help from Mercy Ships. Patients will very often seek initial help from traditional healers in the local community in order to release the evil spirit from their neck mass. Sometimes treatment consists of inflicting small stab wounds and rubbing black tar into the wounds or penetrating injuries to the goitre with hot sharp objects.

Figure 3a: Odi, before surgery, with extensive goitre.

Figure 3b: Odi just before discharge. Most West African patients put on new clothes
and a head scarf provided by Mercy Ships as a symbol of the start of a new life.
A 55-year-old grandmother (Odi), who had an extensive slow growing goitre for 15 years was isolated by her suspicious family and friends and labelled as a witch. Her grandchildren were forbidden from approaching her and sitting on her lap. An extensive goitre with retrosternal extension was excised by ship surgeons, Leo Cheng and AJ Collins. In addition to a total thyroidectomy, she had two separate retrosternal extensions removed with the preservation of her recurrent laryngeal nerves and parathyroid glands, and transplantation of a superior parathyroid gland identified at the surface of her thyroid mass. Her goitre weighed over 1kg. Odi was looking forward to reintegrating with her family and community, especially her loving grandchildren.
Benign mandibular tumour (Figures 4a-b)
Thirty-five year-old Kokou had an extensive mandibular ameloblastoma which first appeared as a small bony expansion on the right body of the mandible seven years before. Apart from difficulties in chewing and swallowing, the tumour slowly reduced his oral airway and he was at risk of upper airway obstruction. His family and friends disowned him accusing him of being ‘demon possessed’.
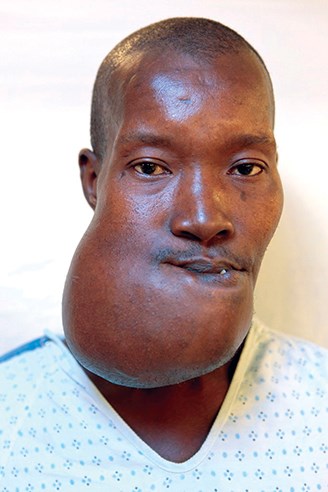
Figure 4a: Kokou, before surgery, with seven years of jaw growth.

Figure 4b: Kokou, nine days after surgery, can eat normally again.
He underwent subtotal mandibulectomy including right condyle and reconstruction with a mandibular titanium reconstruction plate. His jaw tumour weighed 776g. In the early recovery period, Kokou was so astonished by his surgery that he kept using a ship-provided hand mirror to check that his jaw tumour had truly been removed. He was kept nil-by-mouth for a week with nasogastric feeding to ensure good mucosal healing. A second surgery was planned for him in six to nine months’ time to have a cortico-cancellous bone graft from his iliac crest for the reconstruction of his mandible in order to prevent the possible exposure of the reconstruction plate through his skin and to provide a firm wide alveolar base for future oral rehabilitation with partial denture.
Benign parotid tumour (Figures 5a-b)
Raoufou (41 years old) had a slow growing left parotid mass for two years. The mass grew so big and so rapidly that the overlying skin broke down and an oozing fungating ulcer developed. He went around with his head covered to avoid criticism and ridicule from others. Raoufou’s haemoglobin was 5.4g/dl from chronic oozing from his wound and he required a transfusion of whole blood donated by one of the volunteer crew members (the ship effectively has 450 walking blood banks). A mass weighing over 1kg was removed by three ship surgeons (Steuart Heaton, Gary Parker and Leo Cheng) with preservation of the facial nerve. The defect was repaired with multiple local flaps. Again Raoufou could not believe that his facial tumour was removed and kept checking with mirrors and his hand to confirm that the tumour had really gone. This is a common reaction from many of our patients with severe facial deformities as these patients have got used to their extensive facial tumour slowly growing for years, despite the negative effects on their quality of life.

Figure 5a: Raoufou, before surgery, with desperately low haemoglobin
due to constant slow bleeding from the parotid tumour.

Figure 5b: Raoufou, after removal of his extensive facial and neck tumour, with Leo Cheng.
Bilateral benign maxillary tumour (Figures 6a-b)
A 49-year-old patient had a four-year history of a slow growing bilateral maxillary fibrous dysplasia which had started to inhibit his breathing, eating and speech and eventually his ability to work. Lawson, who was once the most prominent football player in Ghana, was now hiding in his house as the people in his village would not sell him food because they said that he was a devil. His wife left him, leaving behind their three children and without work or food, he could not provide for his family. Following a radio announcement about the arrival of the Africa Mercy, Lawson dared to hope and left his children in his mother’s care to attend patient screening. By this time, his maxillary tumour was slowly suffocating him and Lawson was literally on the brink of death.
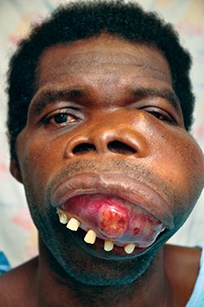
Figure 6a: Lawson, before surgery, with upper
jaw tumour slowly suffocating him.
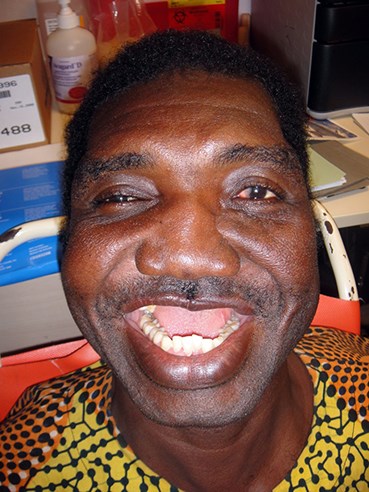
Figure 6b: Lawson, after three surgeons work for
eight hours to remove and reconstruct his maxilla.
Three ship surgeons (Gary Parker, Peter MacDermott and Lou Koeper) removed his maxillary mass and repaired his nose, upper lip and cheek in an eight-hour operation the following day. He lost two and a half litres of blood during surgery and required several blood transfusions, donated by the volunteer crew members. After bilateral zygomatic, orbital and pterygoid plate osteotomy, the maxillary tumour was resected and the defect was reconstructed with a left temporalis muscle flap and the left lacrimal ductal system was maintained using a Crawford tube. Lawson was overjoyed when he touched the bandages of his cheek as the tumour was completely gone. He had two further minor surgeries by Gary Parker and Leo Cheng to repair his oronasal fistula using an advancement nasal and palatal mucosal flaps.
Encephalocele (Figures 7a-b)
It is very rare to see patients with persistent encephalocele at Mercy Ships screenings, which indicates that patients do not survive past childhood. The herniation of meninges and sometimes redundant brain tissue, through a cranial defect, is prone to fatal trauma-induced meningitis.

Figure 7a: Moses, before surgery, with a
frontonasal encephalocele (with his mother).

Figure 7b: Moses, after surgery.
Baby Moses (one-year-old) was born with a significant frontonasal encephalocele and his mother was accused of being involved in witchcraft. After gaining some weight with our feeding programme, Moses had his encephalocele removed and dura repair with a coronal flap, frontal craniotomy and calvarial bone graft by two ship surgeons (Gary Parker and Leo Cheng). Moses required subsequent lumbar punctures to reduce intracranial pressure during the first few days of recovery.
Please visit www.mercyships.org.uk for further information.
Acknowledgement:
All photos are courtesy of Mercy Ships.
Declaration of competing interests: None declared.
Mercy Ships
These are the stories of just a few of the tens of thousands of patients that Mercy Ships has helped over the last 35 years. Each year, the Africa Mercy is staffed by up to 900 volunteers from 35 nations, including many from the UK, that give up their time to help others. Volunteers range from surgeons and nurses, to cooks and engineers. Founded in 1978, Mercy Ships has worked in more than 70 countries providing services valued at more than £630 million, helping in excess of two million people. The charity’s volunteers have treated more than 520,000 people in village medical and dental clinics, performed more than 56,000 surgeries and completed more than 1,000 community development projects focusing on water and sanitation, education, infrastructure development and agriculture.









