The authors present a technique that increases the surface area of a temporalis fascia graft when used to provide smooth, dorsal coverage in cases of open tip rhinoplasty.
Numerous graft materials have been developed for use in rhinoplasty procedures in order to give or improve the contour and hide irregularities [1]. These range from autologous grafts, homografts including acellular dermal matrix (ADM), irradiated cartilage and alloplastic materials.
Autologous grafts are generally preferred due to their easy incorporation into the site and a low rate of complications. One such graft is the fascial graft and many studies report the advantages of long-term durability and decreased inflammation, but with the downside of donor site morbidity.
Background
The application of fascia grafts in rhinoplasty was first introduced with the proposal of cartilage wrapped with temporoparietal fascia [2,3]. The combination of fascia and diced cartilage resulted in smooth edges and prevents ski-jump and parrot-beak deformities. These grafts are soft, non-absorbable, abundant and infection resistant. This combination is useful in treating nasal dorsum, as well as tip, augmentations. It provides a smooth and pliable graft that is ideal for improving contour and volume of the dorsum. It also helps obviate any long-term concern with graft visibility [4].

Figure 1: Diced cartilage layered over the tip using a syringe to provide smooth contour.
The technique
The senior author has been using a temporalis fascia graft for over 15 years. This does not require any position change during the rhinoplasty, the donor site is prepared while preparing and draping the face of the patient. The graft is harvested through a 2.5cm zig-zag incision in the hair bearing area on the temple and, with a trichophytic closure commonly used in hair restoration procedures, the resulting scar is hardly visible [5].

Figure 2: Fascia graft inserted into cartilage morselizer and expanded.
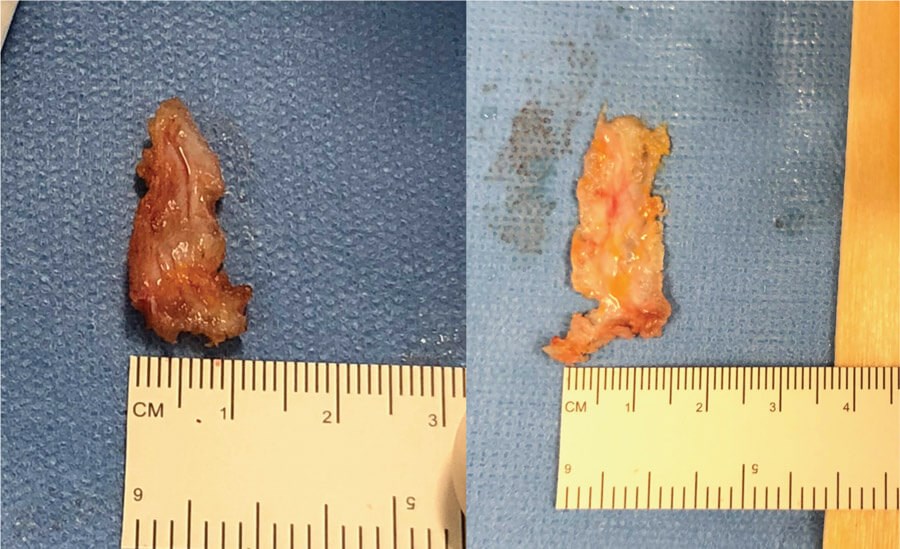
Figure 3: Fascia graft pre and post expansion going from 10mm to 15mm in width.
In a recent description of the anatomy of the temporoparietal fascia it was noted the fascia is approximately 2-3mm thick [6]. When the fascia is freshly harvested it is also a little irregular in contour. In order to flatten / smooth the graft and also increase its surface area the senior author has used a cartilage morselizer and mallet. The technique is illustrated in Figures 2 and 3. In the case shown the width of the graft was increased from 10 to 15mm. The senior author has used this technique in over 2000 cases.

Figure 4: Fascia graft inset over the diced cartilage on the tip and nasal dorsum prior to closure.
One downside reported in the literature when harvesting temporoparietal fascia is transient or permanent alopecia along the temporal incision. However, in the hands of the senior author this has not been a recorded problem. The key is to use a bevelled incision in line with the hair follicles, avoid diathermy in the vicinity of the hair follicles and to use the standard trichophytic closure technique referred to above.
Conclusion
We believe the technique of using a cartilage morselizer to flatten and increase the surface area of the fascial graft is both safe and efficient. It ensures a thin and pliable graft with minimal donor site morbidity. To our knowledge this has not been previously reported in the literature.
References
1. Sajjadian A, Rubinstein R, Naghshineh N. Current status of grafts and implants in rhinoplasty: part I. Autologous grafts. Plast Reconstr Surg 2010;125:40e-49e.
2. Guerrerosantos J. Temporoparietal free fascia grafts in rhinoplasty. Plast Reconstr Surg 1984;74:465-75.
3. Daniel RK, Calvert JW. Diced cartilage grafts in rhinoplasty surgery. Plast Reconstr Surg 2004;113:2156‑71.
4. Guerrerosantos J, Trabanino C, Guerrerosantos F. Multi-fragmented cartilage wrapped with fascia in augmentation rhinoplasty. Plast Reconstr Surg 2006;117:804-12 (discussion 13-16).
5. Vogel JE, Jimenez F, Cole J, et al. Hair restoration surgery: the state of the art. Aesthet Surg J 2013;33(1):128-51.
6. Bohr C, Bajaj J, Soriano RM, et al. Anatomy, Head and Neck, Temporoparietal Fascia. In: StatPearls [Internet] Treasure Island (FL), USA; StatPearls Publishing; 2020 [Available from https://www.ncbi.nlm.nih.gov/books/NBK507912/].
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME







