It is clearly impossible to outline the whole of this subject matter in a short editorial article; many theses have been written in this field. This article is designed to give an overview to those reasonably familiar with this area of work. Facelift has been a commonly requested procedure for many years in an attempt to allay the effects of facial ageing. There are many adjunctive procedures, and less invasive procedures that have been devised.
Some of these are effective, some are counter-intuitive and some are simply a distraction from the underlying problems; however, these are not part of the remit for this overview article. The aim of this article is an attempt at a practical approach to facelifts in the current UK, and to try and formulate a conclusion that applies to the British public that is contemporaneous and relevant. So I will initially précis the problems seen and then try to cover solutions and outcomes.
Anatomy
Clearly a thorough knowledge of basic facial anatomy is required before embarking on facial aesthetic surgery. That means knowledge of the branches and variations of the facial nerve, facial blood vessels and facial muscles. This knowledge is assumed of the audience reading this article, however, many references and textbooks are available for reviewing this subject matter.
The ageing face shows its age in terms of the lines and sags that develop over time. These are the jowls, marionette lines, nasolabial folds, and malar bags (Figure 1).
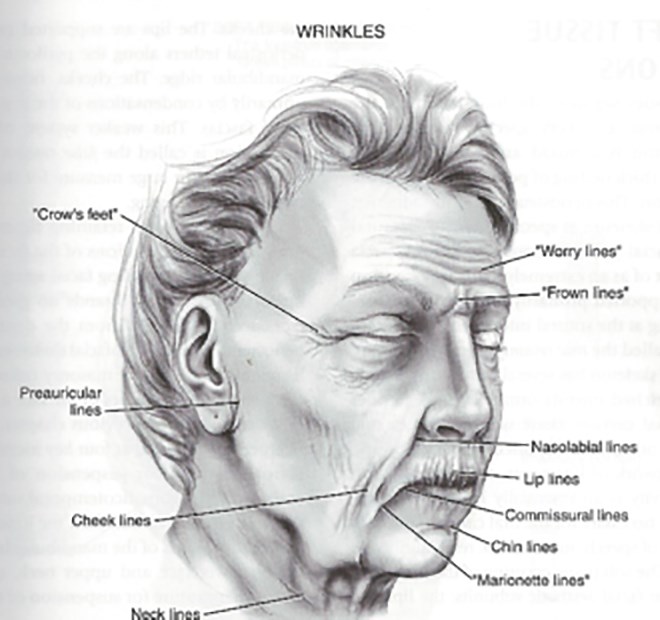
Figure 1.
Naturally the face blends into the neck (covered in a previous article) and the peri-orbital area and forehead are to be covered in the next article in this series. One must be aware of the ‘true’ and ‘false’ ligaments of the face, the five layers of the face as well as the deep spaces described by Bryan Mendelson amongst others [1]. Probably the most important false ligament is the masseteric retaining ligament (Figure 2) which is well known to be near the medial border of the masseter muscle. This separates the true central cheek from the lateral cheek. Anterior to this is the space containing the buccal fat pad.
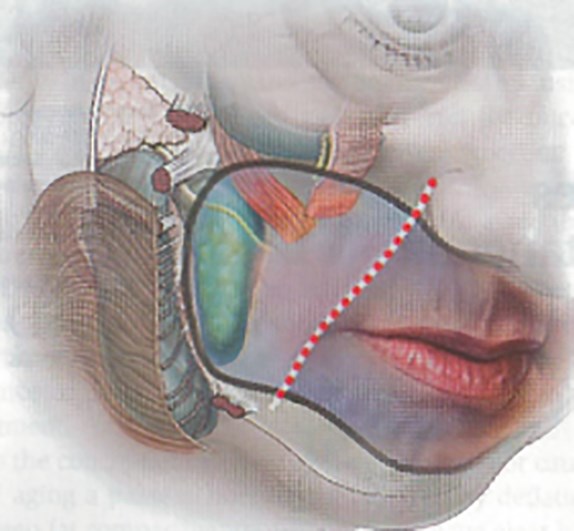
Figure 2a.
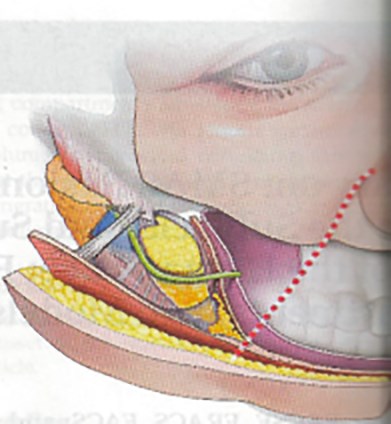
Figure 2b.
The three false retaining ligaments are commonly named the: masseteric ligaments, platysma auricular ligaments, and buccal part of maxillary ligaments. However, the four true retaining ligaments are the orbital, zygomatic, maxillary part of the buccal maxillary ligament, and the mandibular ligaments.
“There are many two-layer options, depending on the patient’s needs and the surgeon’s theory on what the causes of facial ageing are, both in general and in that particular individual”
The excellent article from Joel Pessa describes superficial musculoaponeurotic system (SMAS) fusion zones elegantly in a fresh cadaver study looking at seven specimens (14 sides) [2]. He has essentially worked on from the contribution from Mendelson et al [3]. and that of Kikkawe et al [4].
Fundamentally, Pessa proposes the thesis that facial ageing is predominantly due to de-volumisation of the fat in the facial spaces as opposed to descent and ligamentous attenuation. This, however, remains a hypothesis rather than a proven fact from this work. Pessa’s paper seems to represent a thesis, and is hard to interpret. Essentially, he claims, based on previous anatomical studies, that the retaining ligaments remain static in ageing.
Facial analysis
This can be done in the clinic with an interview with the patient and reviewed with photographs. Three dimensional photography, and laser facial scanning and modeling have their specific indications, particularly in bony alteration where one is considering craniofacial surgery, genioplasty or malar implants. The facial nerve function should be recorded, and an animated video of facial movement can be useful for the record.
Common types of facelift
Broadly, these can be classified as a mini facelift, skin-only facelift, one-layer, two-layer, and deep plane facelifts, with or without midface manipulation.
Mini facelift
There are various short scar facelifts in common usage:
- Thread lifts, of various types, are in widespread use. However, the Dutch Association of Plastic Surgeons has recently advised its members not to offer these treatments due to poor outcomes. These techniques are frequently complicated by tramlining and are limited in direction of pull. They therefore require careful patient selection.
- The one stitch facelift represents a compromise procedure that has limited use in a specific patient group and has limited indications.
Both of the above procedures address only the face; it is rare to see a patient that has facial ageing without neck ageing, although it is something that patients may request.
Minimal scar facelifts
There are various forms of these, currently the most important being the minimal access cranial suspension (MACS) lift. This lift developed from the older S lifts [5], and has become popular due to its simplicity and reduced theatre time. Essentially, the scar is short with a zig zag incision around the sideburn, and the SMAS layer is elevated using two or three looped sutures. This technique can be useful if the neck is not affected, but does lead to visible irregularity in thin patients, and is subject to long-term attenuation.
Classical facelifts
The traditional incision for all standard facelifts is a modification of that shown in Figure 3.
Figure 3.
One-layer facelifts
There are several, very different, one-layer facelift methods possible:
- Thin (skin only) one-layer facelifts are rarely used by experienced surgeons currently, due to poor long-term results. Indications for their use can be after parotidectomy (where the facial nerve is dangerously exposed), in patients who have had silicone based fillers or other permanent fillers where a concrete like scar encases the subcutaneous layers of the face and neck. In most other cases this is a poor approach of limited and short-term value.
- Thick one-layer facelift with a thick layer of fat. This approach can be used in smokers to maintain a better blood supply to the skin, and in youthful patients without deep tissue ptosis. This technique can also be combined with some minimal incision approaches, lipostructure or liposculpture.
- Thick one-layer facelift including SMAS is an approach that can be used in older patients and can help to elevate the anterior face, but is an advanced technique as one is close to the facial nerve, particularly when entering the mid cheek space. This approach can introduce a dog-ear internally, which can supplement the midface and produce midface elevation.
Two-layer facelifts The two-layer facelift is by far the most common approach today. There are many two-layer approaches, however, the main advantage is the ability to elevate tissues in two separate planes, superior and lateral, and vertical. There are many two-layer options, depending on the patient’s needs and the surgeon’s theory on what the causes of facial ageing are, both in general and in that particular individual.
- SMAS plication techniques: in these cases the thin skin flap is elevated, and the SMAS is plicated, either parallel to the nasolabial fold or vertically from modiolus to tragus. The later plication has the advantage of a vertical lift in addition to the lateral lift provided by the skin elevation. Plication is usually carried out with 3/0 French gauge synthetic absorbable suture (e.g. Vicryl) interrupted sutures that are carefully trimmed.
- Low SMAS flap: in these cases the SMAS layer is lifted 1cm below the zygomatic arch well below the zygomatico temporal braches of the facial nerve (ZM/T7). Part of the SMAS flap can be tucked behind the ear to help to elevate the neck.
- High SMAS flap: in these cases the SMAS layer is elevated at the zygomatic arch level. There are two or three branches of the ZM/T7 nerve close by, these should be carefully observed with the help of a nerve stimulator. The advantage of the high SMAS is that the dog ear elevates the midface, thus avoiding a transciliary approach with attendant risk of ectropion.
- All two-layer approaches deal with the lateral face well, but the medial face requires augmentation with fat grafts to the nasolabial folds to improve. If a non-high SMAS method is adopted the midface may need addressing, either using an endoscope from the temple with supplementary intraoral buccal incision for sub orbicularis oculi fat (SOOF) elevation, or via a transciliary approach supporting the SOOF to the orbital periosteum with an anchor to orbital bone.
Composite facelift
The composite facelift with septal reset and arcus marginalis release was devised by Sam Hamra and takes a completely different approach to that described in most of the techniques above [6].
His original concept was to elevate the cheek fat between the zygomaticus major and minor with the skin and kept in continuity with the SMAS. The result, although an improvement, was disharmonious.
Hamra later included the orbicularis oculi muscle in the flap (composite rhytidectomy). Because the orbicularis oculi, cheek fat and platysma were intimately related, the orbit could be transposed in a superiomedial vector. However, the release was incomplete due to tethering at the malar. Hence, release of the arcus marginalis and the septal reset was developed. These manoeuvres created impressive periorbital rejuvenation. So the direction of pull in the classic one-layer facelift as shown in Figure 4a, can result in a windswept look, and does not shorten the infraorbital length, so does not rejuvenate the midface. The composite rhytidectomy, combined with release of the arcus marginalis and septal reset, does not pull in one direction and does rejuvenate the periorbital region (Figure 4b).

Figure 4a.
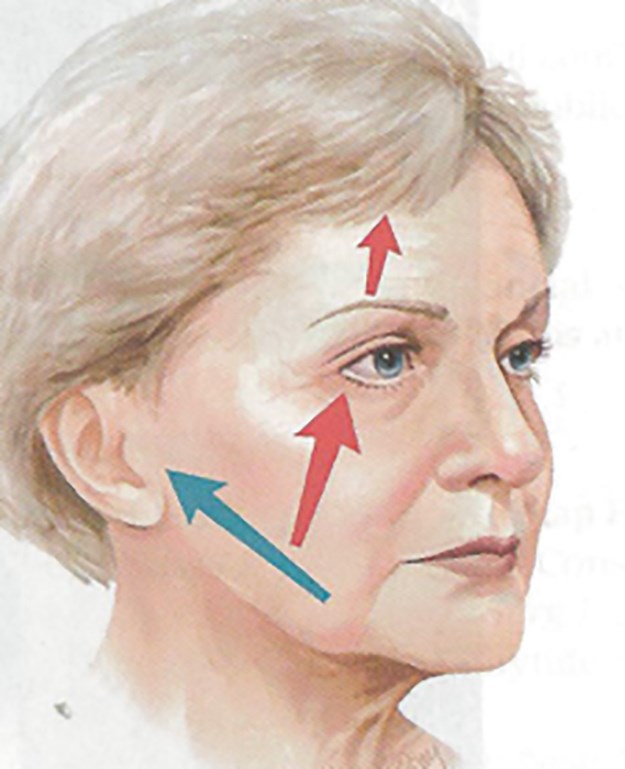
Figure 4b.
Conclusion
Whilst many of the techniques described can be effective, in the modern British setting, choosing the ‘best’ technique is tempered uniquely by the medico-legal environment. Doctors in the UK have for 60 years worked with a population that has come to expect free medicine at every level with the NHS. The financial value of medical care has been long forgotten. In addition, and unlike the US where in many states there is a cap on the value of cosmetic medico-legal settlements, there is no such thing in the UK. When one adds to this the fact that medico-legal reports can often be written for prosecuting lawyers by ‘senior’ plastic surgeons with little specific experience in the procedure under review, and the fact that some experts write overtly negative reports in order to gain further paid medico-legal work from their instructing law firms it is best to learn a few simple workhorse facelift techniques for most instances.
One reason for this is that audit is becoming more important and it is important to demonstrate sufficient volume of activity in any one technique. However, and most importantly, in the UK we currently have the most litigious population in the world, with multimillion pound claims after complications following facelifts becoming successful in the courts over the last few years. Therefore any technique, even if theoretically or actually superior, where there is an increased risk to the integrity of the facial nerve or the skin, must be very carefully approached. Personally, having learned and practised all of the techniques described, I now most commonly practise a two-layer approach with vertical (modiolos to tragus – Figure 5) SMAS plication.
I have always hitched the platysma to Lorre’s fascia to improve the neck and I have found this to require supplementation in the midline with fat transfer. I have usually planned a separate approach to the brow, and midface with fat transfer and elevation with an endoscope or via a transciliary incision. This is a safe method that can be learned by the average practitioner, leading to reduced risk to the patient and maximum effect.

Figure 5.
References
1. Mendelson BC, Wong CH. ‘Chapter 6: Anatomy of the Ageing face’ in Neligan PC, Warren JH (Eds.). Plastic Surgery 3rd Edition, Volume 2, Aesthetic New York, USA; Elsevier; 2012:78-92.
2. Pessa JE. SMAS fusion zones determine the subfascial and subcutaneous anatomy of the human face: fascial spaces, fat compartments, and models of facial aging. Aesth Surg 2016;36(5):515-26.
3. Mendelson BC, Muzzatfat AR, Adams WI. Surgical anatomy of the midcheek and malar mounds, plastic and reconstructive surgery. Plast Reconstr Surg 2002;110(3):900-4.
4. Kikkawe DO, Lemke BN, Dortzbach RK. Relations of the superficial musculoaponeurotic system to the orbit and characterization of the orbitomalar ligament. Ophthalmic Plast Reconstr Surg 1996;12(2):77-88.
5. Tonnard P, Verpaele A. The MACS-lift short scar rhytidectomy. Aesth Surg 2007;27(2):188-98.
6. Hamra ST. Composite Rhytidectomy St Louis, USA: Quality Medical Publishing; 1993.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME








