World renowned dermatologist, Michael H Gold, explains new treatments available in the challenging field of hypertrophic scar and keloid management.
The treatment of hypertrophic scars and keloids remains one of the most challenging conditions that dermatologists face on a regular basis. What is new that we can offer our patients and what should we do when confronted with patients who have these lesions? We have been asking these questions for many years now and it is nice to report in 2018 that we do have several new and evolving therapies that are relevant and important as we explore how we can best treat these difficult lesions.
In 2002, we reported the first international guidelines on care for the treatment of hypertrophic scars and keloids [1]. In the article, where treatment options were provided, it was determined that the use of topical silicone gel or sheets was one of the most important modalities available for these lesions. It was also determined that intralesional (IL) corticosteroids were a mainstay of treatment for hypertrophic scars and keloids and, where they could be easily used, that IL corticosteroids, either alone or in combination with silicone gel, was one of the best modalities for these skin concerns. Surgical procedures, with IL corticosteroids and with topical silicone gel, were found to be important as well. Other therapies, covered in the review, were associated with a higher incidence of recurrences and were not considered as first-line therapies.
In 2014, the second review on the international guidelines appeared [2,3]. Once again, the authors performed an extensive literature search and reviewed the various treatment options that had either appeared earlier or were new to the treatment modalities that could help these lesions. Topical silicone gel, IL corticosteroids, as well as certain newer laser systems and radiation therapy seemed to be prominent choices amongst the group for inclusion in what may be deemed best for our patients with hypertrophic scars and keloids. In addition, the authors reviewed the time when it would be appropriate to treat these lesions. Most of the reported articles in the past had dealt with ‘old’ lesions and when it was looked at comparing new and old scars, the authors concluded that with the use of any of the modalities, that treating these lesions early is superior to waiting an extended period of time. This has been documented in other reports [4].
So what is new? Let’s break this down into some of the new treatment modalities that are now being used regularly for these lesions.
Topical silicone gel
Topical silicone gel has evolved in recent years. We first reported on the use of topical silicone gel in 1993 [5]. In our original article, we showed that when topical silicone gel sheets were applied to an old hypertrophic scar or keloid, we could flatten them over time, reduce any of the associated symptoms that might be associated with the lesions, and take the colour back towards normal. In studies that followed we showed that in a side by side comparison where one half of the hypertrophic scar or keloid was treated with topical silicone gel sheeting, that the side treated with the silicone flattened significantly as compared to the untreated side [6]. We then followed that with a ‘preventative’ study looking at closed surgical wounds where patients had standard dermatologic lesions excised in a standard surgical setting. One scar was treated at the time of suture removal with topical silicone gel and one via conventional wound healing means. The silicone gel sheeting scars healed without recurrences in a statistically meaningful fashion as compared to those with traditional wound healing and was more pronounced in what we called high-risk groups, those that had a history of poor scar formation in the past [7]. These studies and many that followed demonstrated the effectiveness of silicone gel and silicone gel sheeting in treating hypertrophic scars and keloids [8-10].
Over the past year or so, we have been introduced to a new silicone gel formulation, the first one that allows us to apply the silicone gel on closed surgical wounds at the time of surgery or on open wounds, such as those we ‘make’ following a laser or chemical peel procedure. These film-forming silicone gel formulations have been very impressive in their use and in how we now can use them. We know silicone gel can improve scars so if we can use silicone gels at the time of surgery or after a procedure where a wound is formed, we may have an ideal situation where hypertrophic scars or keloids can be prevented or minimised (Figures 1 and 2).
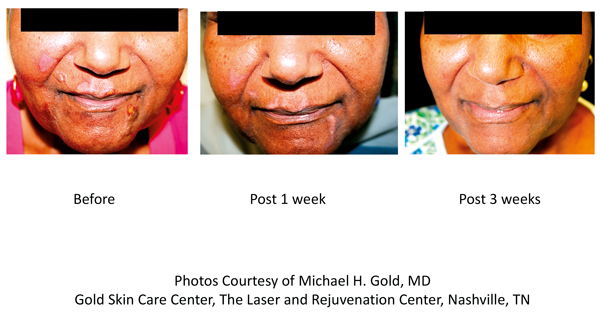
Figure 1. Patient treated with Stratamed® (film-forming silicone gel used
as wound dressing for open wounds, de-epithelised skin).
Laser resurfacing
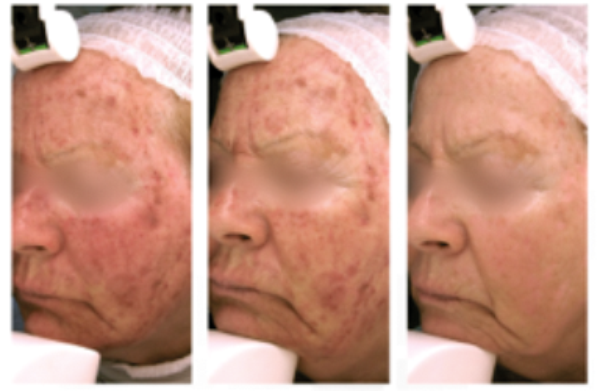
Left: Immediate post procedure Middle: Day 2 Right: Day 3
Figure 2. Patient treated with Stratacel® (film-forming silicone gel used as wound dressing for fractionated skin).
Another interesting product in the ‘silicone’ family involves the use of silicone oil with a stabilised hypochlorous acid formulation. Hypochlorous acid has many incredible attributes and reports have shown that it can interfere with all the phases of wound healing. Adding silicone oil has an added benefit since we know how well silicone works on hypertrophic scars and keloids. Studies have shown that with this formulation, hypertrophic scars and keloids can be reduced and this has become one of the more interesting ‘silicones’ on the market [11].
“We now have new methods and new treatment options at our disposal which can help clinicians offer treatments and procedures to help change the lives of many.”
Fractional CO2 lasers
One of the more fascinating treatment options for hypertrophic scars and keloids, which has become more and more routine amongst laser physicians, is the use of fractional CO2 lasers to reduce and minimise hypertrophic scars and keloids. Through the development of heat-shock proteins, one can use the fractional capabilities of the CO2 laser to interact with the scarred collagen and help to develop new collagen in its place [12]. Raised scars can be flattened over time and scars can be virtually eliminated.
With laser therapy, we have learned that the earlier we treat these lesions, the better the result. Newer scars responded very well to CO2 fractional lasers and this has been shown in several review articles dealing with fractional CO2 lasers and treating hypertrophic scars and keloids [2-4]. Recent work with colleagues in Changsha, China has also shown the effectiveness of the fractional CO2 laser, alone or in combination with the pulsed dye laser (PDL) [13,14]. Clinical examples are shown in Figures 3 and 4.
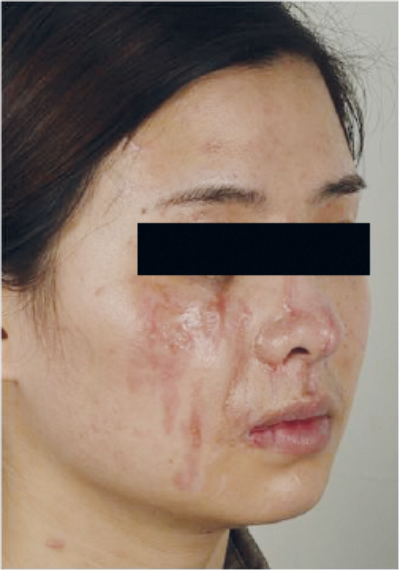
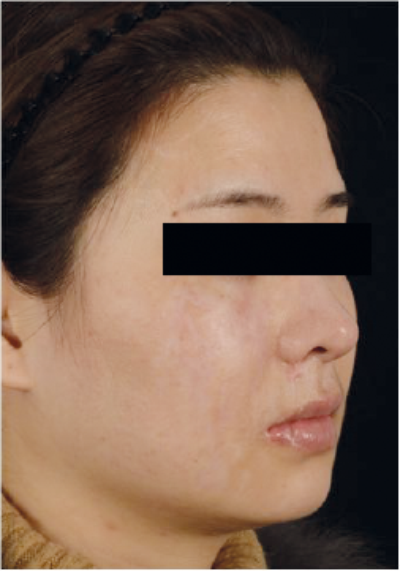
Figure 3. Pre- and post-fractional CO2 for hypertrophic scar
(compliments of Dr Tan Jun, Changsha, China).

Figure 4. Pre- and post-fractional CO2 for hypertrophic scar
(compliments of Dr Tan Jun, Changsha, China).
Superficial radiation therapy
Finally, the use of superficial radiation therapy, (SRT), has been found to be a novel, yet game-changing procedure for many patients with keloids who have lesions that may have, in the past, been difficult to treat and in those lesions where high recurrence rates were expected, based on size and location of the keloid. SRT is a US FDA approved procedure for the treatment of keloids and results to date have shown that when performed following a surgical procedure, recurrence rates at one year are under 10% [15].
SRT is performed in one’s clinical office, so there is no need to ‘refer’ a patient to a specialised clinic for the procedure. We have one ‘dedicated’ SRT clinic room in the practice which has been lead-lined and detailed so that we can monitor the patient from the outside of the room and be able to make sure that everything is working appropriately during the treatment.
When we are confronted with a patient with a keloid we think is amenable to SRT treatments, we excise the keloid or work with a plastic surgeon who can do that excision for us. For three consecutive days, we perform SRT treatments on that excised keloid area. The radiation dose is calculated and delivered in three doses, or fractions, so as to limit the potential for any adverse effects, or radiation dermatitis that may be seen when giving large doses of radiation in one setting. Clinical trials have shown how effective this therapy can be and we have used this in numerous patients with, at times, amazing results. An example of SRT treatment on a keloid lesion is shown in Figure 5.
Left: Before Middle: During Right: Immediate Post Surgery

Left: Post SRT Middle: 1 Month Post SRT Right: 2 Month Post SRT
Photos Courtesy of Michael H. Gold, MD, Gold Skin Carer Center, The Laser and Rejuvenation Center, Nashville, TN.
Figure 5. Keloid treatment pre-and post-SRT.
Discussion and conclusion
The treatment of hypertrophic scars and keloids is not easy. There are many appropriate therapies out there where we can reduce these scars, although recurrences are always something that one must be aware of and patients must be kept informed of the risk of recurrence. In 2018, we are looking at new modalities to treat these lesions and to minimise potential recurrence rates. We may have now found new answers to this problem and we are now using these new therapies daily to help patients with these difficult to treat lesions.
Something that we have been doing more and more is using combination therapy when we deal with hypertrophic scars and keloids. As noted earlier, we will use IL corticosteroids in treating many lesions, especially small scars that we think will respond to this kind of therapy. When we do IL corticosteroids, we also routinely use topical silicone gel on the lesions at the same time. We have found that this helps in most instances.
When we use fractional CO2 lasers, we now use our topical silicone form-filming gel immediately after the procedure and during the healing process. Not only do we think that this helps prevent potential reforming of the scar, there is some data emerging that with the topical silicone form-filming gel that we can heal the fractional wound faster than when we use traditional wound healing. Clinical trials showing this effect and the positive nature of this work will be published shortly [16].
When we use SRT, we will also use silicone gel in the post-treatment phase, again to prevent potential recurrences from occurring. More studies into this combination are needed but potentially this may be another useful combination therapy.
Treating hypertrophic scars and keloids is sometimes a daunting task for dermatologists and plastic surgeons who see patients with these lesions. We now have new methods and new treatment options at our disposal which can help clinicians offer treatments and procedures to help change the lives of many.
References
1. Mustoe TA, Cooter RD, Gold MH, et al. International clinical guidelines for scar management. Plastic Reconstruct Surg 2002;110:560-71.
2. Gold MH, Berman B, Clementoni MT, et al. Updated International Clinical Recommendations on Scar Management: Part 1 – Evaluating the Evidence. Dermatol Surg 2014;40:817-24.
3. Gold MH, McGuire M, Mustoe TA, et al. Updated international clinical recommendations on scar management: Part 2 – algorithms for scar prevention and treatment. Dermatol Surg 2014;40:825-31.
4. Anderson RR, Donelan MB, Hivnor C, et al. Laser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing - consensus report. JAMA Dermatol 2014;150(2):187-93.
5. Gold MH. Topical silicone gel sheeting in the treatment of hypertrophic scars and keloids. A dermatologic experience. J Dermatol Surg Oncol 1993;19(10):912-6.
6. Gold MH. A controlled clinical trial of topical silicone gel sheeting in the treatment of hypertrophic scars and keloids. J Am Acad Dermatol 1994;30:506-7.
7. Gold MH, Foster TD, Adair MA, et al. Prevention of hypertrophic scars and keloids by the prophylactic use of topical silicone gel sheets following a surgical procedure in an office setting. Dermatol Surg 2001;27:641-4.
8. Quinn KJ, Evans JH, Courtney JM, et al. Non-pressure treatment of hypertrophic scars. Burns Incl Therm Inj 1985;12:102-8.
9. Berman B, Flores F. Comparison of a silicone gel-filled cushion and silicon gel sheeting for the treatment of hypertrophic or keloid scars. Dermatol Surg 1999;25:484‑6.
10. Berman B, Perez OA, Konda S, et al. A review of the biologic effects, clinical efficacy, and safety of silicone elastomer sheeting for hypertrophic and keloid scar treatment and management. Dermatol Surg 2007;33:1291-302.
11. Gold MH, Andriessen A, Dayan SH, et al. Hypochlorous acid gel technology–its impact on post procedure treatment and scar prevention. J Cosmet Dermatol 2017;16(2):162-7.
12. Capon A, Iarmarcovai G, Gonnelli D, et al. Scar prevention using Laser-Assisted Skin Healing (LASH) in plastic surgery. Aesthetic Plast Surg 2010;34(4):438-46.
13. Lei Y, Li SF, Yu YL, et al. Clinical efficacy of utilizing Ultrapulse CO2 combined with fractional CO2 laser for the treatment of hypertrophic scars in Asians-A prospective clinical evaluation. J Cosmet Dermatol 2017;16(2):210-6.
14. Ouyang HW, Li GF, Lei Y, et al. Comparison of the effectiveness of pulsed dye laser vs pulsed dye laser combined with ultrapulse fractional CO2 laser in the treatment of immature red hypertrophic scars. J Cosmet Dermatol 2018;17(1):54-60.
15. Berman B, Nestor M. Low rate of keloid recurrences following treatment of keloidectomy sites with a biological effective dose 30 of superficial radiation. Abstract presented at the American Society for Dermatologic Surgery Annual Meeting, October 2017.
16. Gold MH. Personal Communication. 2018.
TAKE HOME MESSAGE
-
Treating hypertrophic scars and keloids in today’s environment has some new and exciting therapies available
-
These include new topical silicone gels and silicone products, new laser systems including the fractional CO2 laser, and when needed, superficial radiation therapy
-
Combination therapy is very important and we use combinations of all the modalities to achieve the best outcomes in our patients
Declaration of competing interests:
Dr Gold is a consultant and performs clinical research for Stratpharma. He is also performing clinical research for Biofrontera and is a consultant to Sensus Healthcare. He has been a consultant to Dusa Pharmaceuticals and performed clinical research for them in the past.
COMMENTS ARE WELCOME