The harmful effects exerted upon living and injured tissues by free radicals have been explored since the 1980s. Now in 2021 the free radical nitric oxide (NO) is not just a figment of imagination; it is known as one of the most biologically important bioactive chemicals and signalling agents acting within the body’s metabolism [1,2].
Endogenous NO (ENO) is primarily metabolised at cellular level from nitrites ingested as food, especially leafy salads, root vegetables and beetroot and was formerly known as endothelium-derived relaxing factor (EDRF) because it had a role in the control of hypertension [3]. It is one of the nitrogen oxides and is synthesised within all living cells by an enzyme NO synthase (NOS) [4]. This enzyme catalyses the oxidation of L-arginine to L-citrulline, producing NO, which diffuses freely into vascular smooth muscle, activating guanylate cyclase which in turn converts guanosine triphosphate into cyclic guanosine monophosphate (cGMP), causing vascular relaxation (Figure 1).
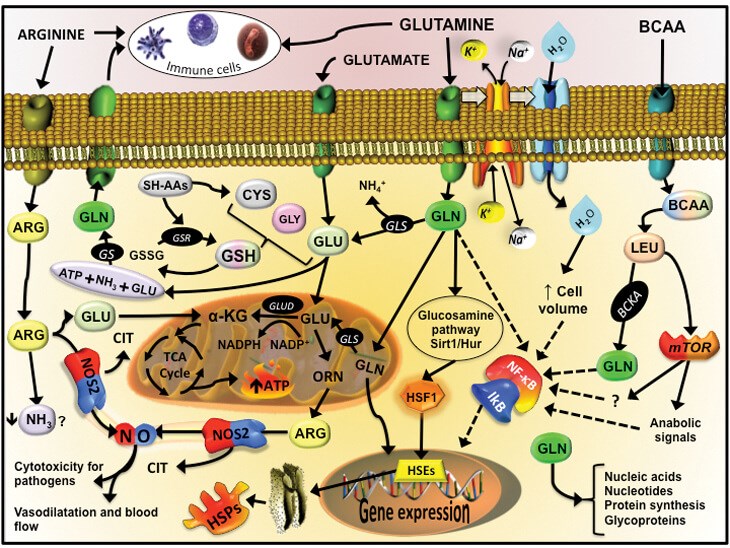
Figure 1: Endogenous plasma production in-vivo. This diagram shows the intracellular pathway
to produce freely diffusible nitric oxide from ingested glutamine, arginine and BCAA.
Courtesy of Dr Vinicius Cruzat, CC BY-SA 4.0
(https://creativecommons.org/licenses/by-sa/4.0 via Wikimedia Commons).
ENO mainly acts to restore and maintain body homeostasis by working as a biological mediator and important chemical transmitter throughout the body, but especially in vascular smooth muscle relaxation and in the brain where it acts as a neurotransmitter. ENO is involved in the aggregation and adhesion of platelets and on macrophages where it is involved in the response to infection. Whilst the bioactivity of NO is largely beneficial to the host there may be potential harmful effects in conditions such as septic shock. In septic shock the overproduction of ENO amongst other bioactive pathways results in profound hypotension and capillary leak. Nitric oxide inhibits hypoxic pulmonary vasoconstriction and preferentially increases blood flow through well-ventilated areas of the lung, thereby improving ventilation: perfusion relationships [5-7].
Atmospheric nitrogen and oxygen react and combine during the formation of hot plasma to form a bio-reactive soup of cold plasmas composed mainly of ozone and nitric oxide. These bio-reactive plasmas and their electrons are not bound to protons so are highly responsive to electromagnetic fields.
“For over 10 years NO has been studied for its potential as an antiviral, antimicrobial and antifungal agent”
The charge is always looking for a way to gain a proton from a nearby object, gas or organism and at this point it deactivates to a less active by-product. Ozone is a fairly toxic plasma derivative and can be harmful to lungs if inhaled, but it can have important antimicrobial properties. NO is significantly safer and like all charged free radicals will very quickly deactivate in air (less than five seconds), to form nitrogen dioxide (2NO + O2 = 2NO2) and to a much lesser amount its dimer, dinitrogen tetroxide (N2O4). It is bioactive during this time and in small quantities is non-toxic, but will kill microbes. If the air is humidified, NO2 can be converted into nitric acid (HNO3) at trace levels and this itself can be bioactive.
Cold plasma NO is manufactured for use in the NHS on an expensive industrial scale as a by-product during the generation of thermal plasma in air [8]. The NO gas is extracted then stored in large aluminium or stainless steel cylinders which are typically in volumes of 40 litres. These will contain 100/1000 or 2000ppm of nitric oxide in nitrogen. Pure NO is corrosive and toxic and is clearly not for clinical use. In medical practice the NO gas is injected via the patient limb of the inspiratory circuit of a ventilator and the delivery system is designed to minimise the oxidation of nitric oxide to nitrogen dioxide. In neonatal, paediatric or adult pulmonary hypertension, exogenous inhaled NO (1-150ppm) is used to produce selective pulmonary vasodilatation. Its use in acute respiratory distress syndrome (ARDS) is increasing, although clear effects on survival have not been conclusively demonstrated. In advanced pulmonary disease the effects of exogenous NO are limited by the delivery to target and the ability of host cells to respond. On a lighter note, it is also possible that higher tissue levels of NO exhibit anti-ageing activity [9], but more importantly there may be a role for nitric oxide in the treatment of malignancy, yet this is very difficult to prove in-vivo [10-12].
Inhaled NO readily reacts with oxidised haemoglobin to yield methaemoglobin and with longer-term care in neonates and these levels must be monitored regularly using electrochemical analysers. Exposure to 500-2000ppm of NO can result in methaemoglobinaemia and pulmonary oedema, but this is rarely seen and is more common in paediatric patients or those with methaemoglobinaemia reductase deficiency. Environmental levels should not exceed 25ppm for eight hours (time-weighted). NO at monitored levels below 80ppm can be safely inhaled by patients with clinical need and even without scavenging, the expiratory effluent gases are still well below levels of concern in the longer-term exposure to NO by attending staff [13]. These cylinders are, however, expensive, impractical and bulky and need to be stored and transported. It is now possible to generate nitric oxide from air both cheaply and environmentally safe.
Nitric oxide is known as a cold plasma and at environmental temperature will kill viruses, pathogenic antibiotic resistant bacteria and fungi [14-17]. At room temperature and in monitored levels it is non-toxic in the environment and to living cells; in fact it is stimulatory to re-epithelialisation, promotes wound healing and removal of biofilm and even antibiotic resistant organisms [18-20]. There are many references to the medical efficacy of using nitric oxide in clinical situations other than cardio-pulmonary medicine, especially in wound healing where nitric oxide will penetrate deeply into chronic wound biofilm to kill established bacteria that will otherwise not respond to topical or systemic antibiotics. There are now clear advantages to the use of exogenous NO for disinfection and sterilisation over conventional methods such as ultraviolet C light (UVC) (because of carcinogenic risk, time to sterilise and need for close proximity and direct view to target), hypochlorous acid (because of liquid state and storage), alcohol and ethane (highly flammable), chlorine dioxide and ozone (harmful to lungs and mucosa), radiation (mutagenic and carcinogenic) and steam (liquid state and impractical) [21-24].
“There is evidence that NO can kill viruses and in particular coronavirus”
Avoiding infection or contamination with COVID-19 is vitally important because it is easily transmitted and lives for many hours on almost all surfaces, except perhaps copper [25]. COVID-19 illness is caused by a novel coronavirus that is transmitted through the air and by bodily contact with contaminated surfaces or individual carriers and affects everyone differently; to date the total UK deaths stand at over 100,000. There is also an unknown, but likely long-term, serious morbidity associated with the disease, especially where there has been significant lung injury. The virus thrives in moist conditions and is droplet spread through coughing and contact with surfaces, including handrails, masks, coins and furnishings. Social distancing, isolation and hand washing have been the mainstay plan for controlling the virus thus far, however sterilising all potential areas of contact should be an important avenue of avoiding infection and onward transmission. There is evidence that NO can kill viruses and in particular coronavirus [26].
For over 10 years NO has been studied for its potential as an antiviral, antimicrobial and antifungal agent. It may work well alone or in combination with other plasma generated gases such as ozone. NO is already used to effectively sterilise sensitive medical equipment and has many advantages over its alternatives. ENO has been demonstrated in laboratory studies to promote epithelial growth and speed up wound healing and also kills at least 99.9% of enveloped and non-enveloped viruses, common bacteria, antibiotic resistant bacteria and fungi. NO is used in the European food industry and there is some evidence that there is a reduction in the rate of putrefaction. A European Commission circular states that there is no restriction in the use of dry plasma as a preservative for organic foods. NO particles have a neutral static electric charge and are known to kill dangerous airborne viruses like MERS-CoV or SARS-CoV and antibiotic resistant strains of bacteria. By the law of static charge a neutral charged particle is attracted to a negative charge. The outer shell of a coronavirus is composed of a negatively charged phospholipid, so attracts the NO [27]. The exact mechanism of viral kill is not clearly understood but there is a disruption of the outer shell, a disruption of the normal intracellular enzymatic pathways, formation of reactive chemical species and interference of RNA / DNA metabolism and replication [28-30].
Summary
NO is a highly reactive gas formed by natural chemical and physical reactions in the atmosphere and is also produced by metabolism in animal and plant cells from the amino acid L-arginine. It can also be produced exogenously and purified or mixed with other plasma reactive gases to suit purpose. The NO particle has a very small mass and is readily diffusible so can easily pass through cell membranes to exert its effect on biological targets. As a gas it is freely diffusible within a space and has numerous potential applications in plastic surgery and burn care, in addition to applications in other specialties such as oral medicine, dermatology, ophthalmology and anaesthesia. NO also has a role in sterilising and disinfection within the community and in this COVID-19 pandemic there appears to be an immediate application for this highly important particle.
References
1. Fang FC. Antimicrobial reactive oxygen and nitrogen species: concepts and controversies. Nature Reviews Microbiology 2004;2(10):820-32.
2. Graves DB. The emerging role of reactive oxygen and nitrogen species in redox biology and some implications for plasma applications to medicine and biology. J Phys D Appl Phys 2012;45:263001.
3. Chowdhary S, Townend JN. Nitric oxide and hypertension: not just an endothelium derived relaxing factor! Journal of Human Hypertension 2001;15:219-27.
4. Lundberg JO, Weitzburg E, Gladwin MT. The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Disc 2008;7:156-67.
5. Lee A, Butt W. Nitric oxide: a new role in intensive care. Crit Care Resusc 2020;22(1):72-9.
6. Martel J, Ko Y-F, Young J, Ojcius DM. Could nasal nitric oxide help to mitigate the severity of COVID-19? Microbes Infect 2020;2:168-71.
7. Alvarez RA, Berra L, Gladwin MT. Home Nitric Oxide Therapy for COVID 19. American Journal of Respiratory and Critical Care Medicine 2020;202(1):16-20.
8. Malik MA. Nitric Oxide Production by High Voltage Electrical Discharges for Medical Uses: A Review. Plasma Chem Plasma Process 2016;36:737-66.
9. Valcarcel-Ares MN, Gautam T, Warrington JP, et al. Disruption of Nrf2 signaling impairs angiogenic capacity of endothelial cells: implications for microvascular aging. J Gerontol A Biol Sci Med Sci 2012;67:821-9.
10. Hirst AM, Frame FM, Arya M, et al. Low temperature plasmas as emerging cancer therapeutics: the state of play and thoughts for the future. Tumor Biol 2016;37:7021-31.
11. Ratovitski EA, Cheng X, Yan D, et al. Anti-cancer therapies of 21st century: Novel approach to treat human cancers using cold atmospheric plasma. Plasma Process Polym 2014;11:1128-37.
12. Trachootham D, Alexandre J, Huang P. Targeting cancer cells by ROS-mediated mechanisms: a radical therapeutic approach. Nature Rev Drug Discov 2009;8:579-91.
13. Qureshi MA, Shah NJ, Hemmen CW, et al. Exposure of intensive care unit nurses to nitric oxide and nitrogen dioxide during therapeutic use of inhaled nitric oxide in adults with acute respiratory distress syndrome. Am J Crit Care 2003;12(2):147-53.
14. Sakudo A, Yagyu Y, Onodera T. Disinfection and Sterilization Using Plasma Technology: Fundamentals and Future Perspectives for Biological Applications. Int J Mol Sci 2019;20:5216.
15. Mannick JB. Immunoregulatory and Antimicrobial Effects of Nitrogen Oxides. Proceedings of the American Thoracic Society 2006;3:161-5.
16. Akaike T, Maeda H. Nitric Oxide and Virus Infection. Immunology 2000;101:300-8.
17. Long R, Light B, Talbot JA. Mycobacteriocidal Action of Exogenous Nitric Oxide. Antimicrobial Agents and Chemotherapy 1999;43:403-5.
18. Gilmore BF, Flynn PB, O’Brien S, et al. Cold plasmas for biofilm control: opportunities and challenges. Trends Biotechnol 2018;36:627-38.
19. Brun P, Bernabè G, Marchiori C, et al. Antibacterial efficacy and mechanisms of action of low power atmospheric pressure cold plasma: membrane permeability, biofilm penetration and antimicrobial sensitization. J Appl Microbiol 2018;125:398-408.
20. Maisch T, Shimizu T, Li Y-F, et al. Decolonisation of MRSA, S. aureus and E. coli by Cold-Atmospheric Plasma Using a Porcine Skin Model In Vitro. PLoS ONE 2012;7:e34610.
21. Laroussi M. Sterilization of contaminated matter with an atmospheric pressure plasma. IEEE Trans Plasma Sci 1996;24:1188-91.
22. Ehlbeck J, Schnabel U, Polak M, et al. Low Temperature Atmospheric Pressure Plasma Sources for Microbial Decontamination. J Phys D Appl Phys 2011;44:013002.
23. Moisan M, Barbeau J, Crevier M-C, et al. Plasma sterilization. Methods and mechanisms. Pure Appl Chem 2002;74:349-58.
24. Laroussi M. Low temperature plasma-based sterilization: overview and state-of-the-art. Plasma Process Polym 2005;2:391-400.
25. Van Doremalen N, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. Letter to the Editor. N Engl J Med 2020;382:1564-7.
26. Guo L, Xu R, Gou L, et al. Mechanism of virus inactivation by cold atmospheric-pressure plasma and plasma-activated water. Appl Environ Microbiol 2018;84:e00726-e18.
27. Alekseev O, Donovan K, Limonnik V, Azizkhan Clifford J. Nonthermal dielectric barrier discharge (DBD) plasma suppresses herpes simplex virus type 1 (HSV-1) replication in corneal epithelium. Trans Vis Sci Tech 2014;3:2.
28. Guo L, Xu R, Gou L, et al. Mechanism of virus inactivation by cold atmospheric-pressure plasma and plasma-activated water. Appl Environ Microbiol 2018;84:e00726-e18.
29. Genest PC, Setlow B, Melly E, et al. Killing of Spores by Bacillus subtilis by Peroxynitrite Appears to Be Caused by Membrane Damage. Microbiology 2002;148:307-14.
30. Liao X, Liu D, Xiang Q, et al. Inactivation mechanisms of non-thermal plasma on microbes: a review. Food Control 2017;75:83-91.
Declaration of competing interests: James Frame advised and help establish Fourth State Medicine in developing Nebulaskin, a hot plasma dermal resurfacing tool. He has also researched and co-founded NOxWorldwide. This company is developing commercial applications for nitric oxide especially to use as a disinfecting tool against COVID and other pathogenic organisms.
COMMENTS ARE WELCOME







