The first use of silicone implants for buttock augmentation was by Bartels et al. in 1969 [1]. We must acknowledge the innovative and imaginative brilliance of the Brazilians and the descriptive detail of other surgeons, but especially Mendietta for the significant advances in the understanding of how to successfully augment the buttocks thereafter [2,3].
This has become ever more important with the advent of weight loss programmes which cause an almost pathological loss of buttock tissue often leading to undesirable aesthetic appearance and functional difficulties.
The key to understanding buttock augmentation is to understand the surface anatomy and what constitutes an attractive buttock [4]. The surgical options for buttock enhancement, and gluteal ptosis correction, include autologous fat transfer, major tissue flap / reconstructive techniques or the use of silicone buttock implants. The intention should be to use the least invasive technique that gives the best possible result with the least risk of complications. Often this will be achieved by using a combination of techniques according to cosmetic requirements and reasons for surgery.
In Brazil it is estimated that one in two women want or have had cosmetic surgery and it is perfectly acceptable to consider buttock augmentation in the presence of ‘normal’ buttocks. In the USA perhaps there is less demand, but the ‘J-Lo’ effect is real. In the UK there is the ‘Pippa’ effect and there is a general acceptance that enhancement can help aesthetic appearance, but few actually proceed to surgery. Those that do are most likely to present with buttock flatness and droopy buttock ptosis as occurs after massive weight loss (MWL) [5]. It is important to also recognise the different structural shapes or ‘frames’ around the gluteal region when selecting the technique for enhancement.
Figure 1: ‘A’ frame.
Figure 2: ‘V’ frame.
Figure 3: Round frame.
Figure 4: Square or oblong frame.
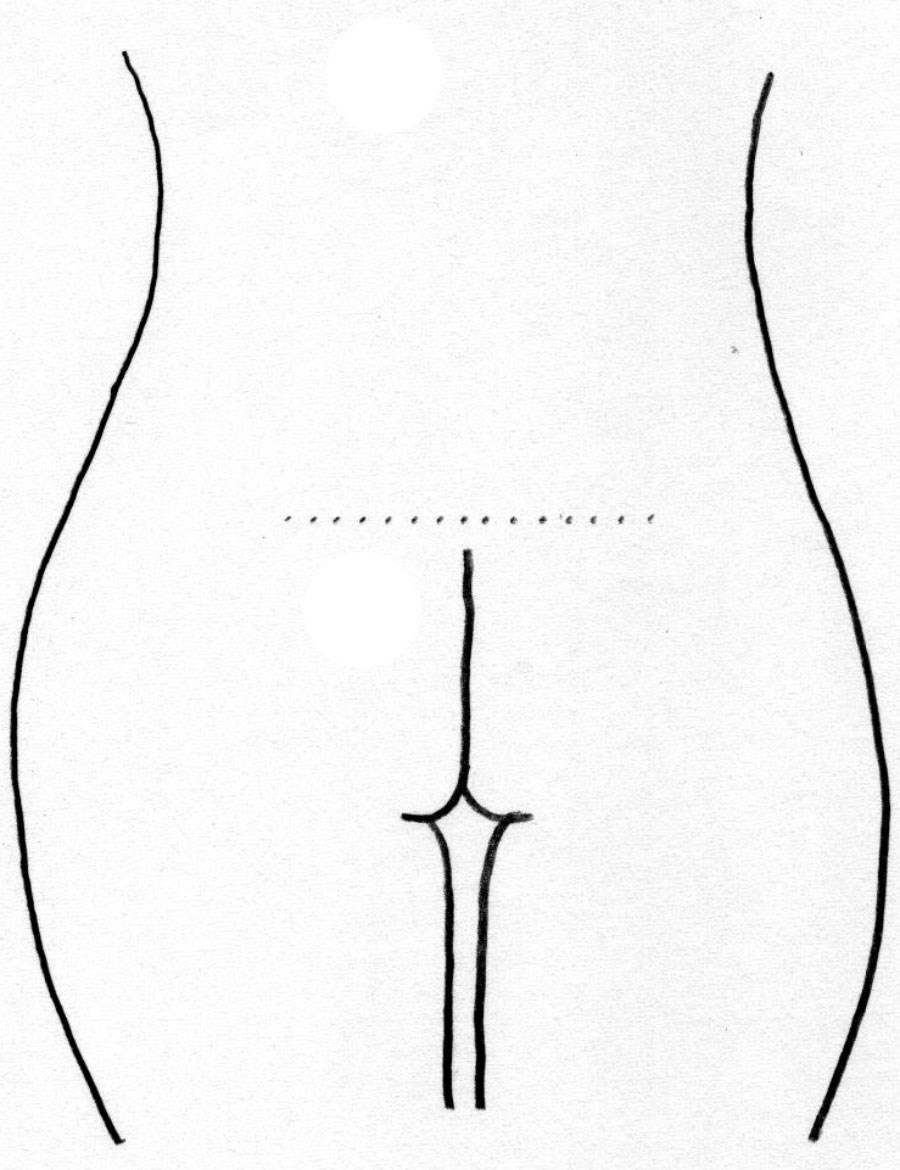
Figure 5: ‘J’ frame.
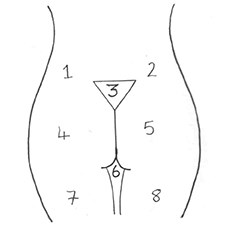
Figure 6: The centeno units.
Buttock shapes
As described by Mendietta, there are the ‘V’ frame, ‘A’ frame, ‘round’ frame and ‘square’ or ‘oblong’ frame buttock shapes currently described. To this we can add the ‘J-frame’ buttock appearance (Figures 1, 2, 3, 4 and 5).
Gluteal ptosis
A simple and logical classification of gluteal ptosis is that adapted from Salcedo et al [6].
- No ptosis - The ideal buttock, where the visible infragluteal fold extends only one third the medial to lateral distance from Zone 6. The ‘J-frame’ buttock.
- Grade 1 - Evident laxity of the skin with the infragluteal fold extending more than one third of the ‘available’ buttock crease.
- Grade 2 - Lax tissue and a prominent gluteal fold extending completely across the ‘available’ infragluteal fold. Early vertical descent of the fibro-fatty buttock tissue.
- Grade 3 - Infragluteal fold hidden by markedly sublaxing gluteal tissue. Gluteus maximus remains in position.
Understanding gluteal ptosis enables the surgeon to consider fat grafting or gluteal implants as options for enhancing and variably correcting the ptotic buttock. Grades 1 and 2 invariably can be improved with fat grafting. Buttock implants are used for volume loss and buttock flattening where a degree of firmness and shape is required. Augmenting buttock tissue using local flaps should be avoided due to risk and excessive, often unnecessary, scarring, but this may be necessary in Grade 3 ptosis patients. The gluteus maximus is not itself ptotic, it is the loss of volume and elasticity of the subcutaneous tissue, within the fibro-fatty buttock tissue, that produces the ptotic appearance.
The zones of the buttock
There are a number of anatomical subdivisions or units that can be described around the buttocks. In simplistic terms the best is that described by Centeno [7]. It becomes descriptive when considering zonal defining using liposuction, and autologous fat transfer techniques (Mendietta [8]).
Buttock augmentation with implants
Buttock augmentation with implants is not difficult and can usually be completed within one hour. It is, therefore, comparatively faster than breast augmentation. However, certain principles must be adhered to and special instrumentation permits safer and more precise surgery. By assimilating the available data [9], it is clear that the intramuscular pocket provides the safest and easiest options with longevity. A specialist dissector is required (Figure 7).

Figure 7: Blunt Gonzalez dissector (Richter Surgical ®, Brazil)
used to create intra-gluteal pocket prior to implant insertion.

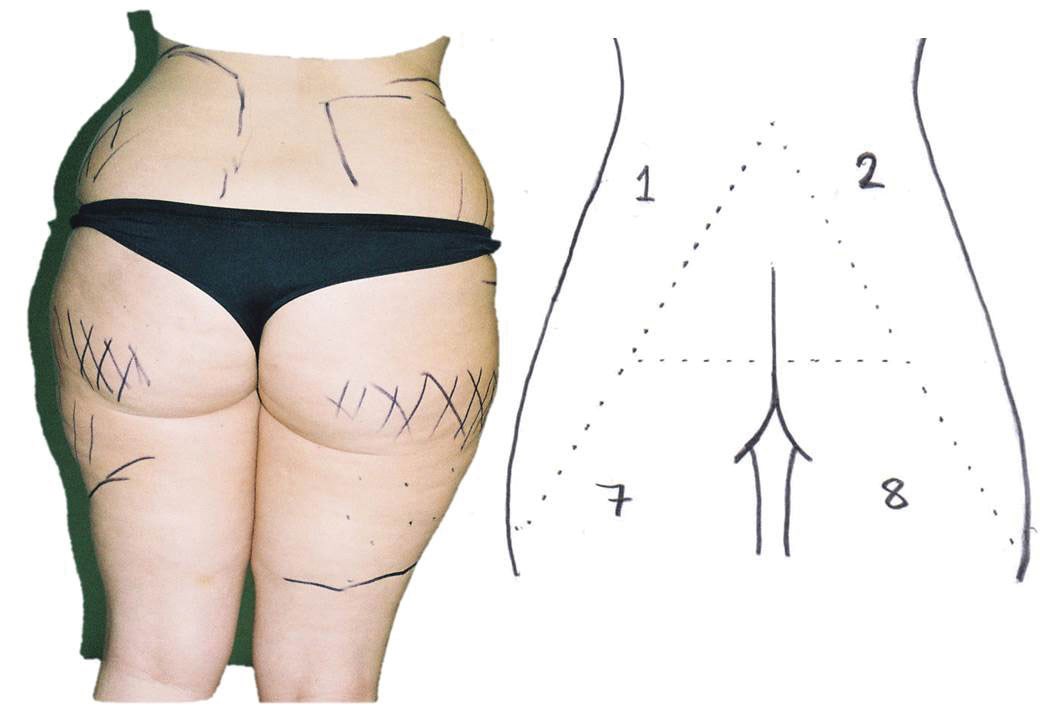
Figure 8: ‘V’ frame: Aquavage® Fat Transfer System.
Zones one / two (waist) to zones four / five (buttocks).

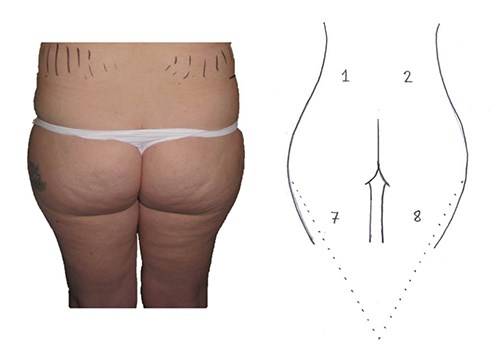
Figure 9: Round frame: Aquavage® Fat Transfer System.
Zones one / two (waist) to zones four / five (buttocks).
The patient is marked in the upright position (Figures 8 and 9). Under general anaesthetic the patient is placed prone in a slight ‘jack-knife’ position. The anus is covered. Two vertical skin incision markings are carefully positioned to be hidden, whilst in the erect position. About 1cm from the midline natal cleft, incisions are made into each medial buttock. Both incisions are, therefore, separated by at least 2cm and intervening necrosis is unlikely. Other surgeons prefer a midline incision. Wound dehiscence and infection risks are considered higher and are best avoided using the 2cm separated wounds as described. Using diathermy the wounds are deepened laterally until the fascia covering the buttock fibres is identified. Incisions are made into the fascia and the gluteal muscle fibres are dissected / separated in a bloodless field to a depth of 2cm.
The specialist blunt dissector is then inserted and easily creates a pocket using sweeping movements. Care must be taken laterally to avoid opening fascia over the lateral border of gluteus maximus and potentially creating a space into which the implant could displace. If carried out within the gluteus maximus at a 2-3cm depth, there is no risk of damage to the sciatic nerve and no loss of neurovascular supply to the muscle. Provided that the pocket size is correct for the selected implant, there is no requirement for drain insertion. The gluteal fascia is closed after implant insertion, and the rest of the wounds are closed in two layers.
The patient is nursed prone or laterally for the first few days, but can be immediately mobilised (pain permitting). TED stocking and flowtrons are used peri- and postoperatively until the patient is mobile. Results are satisfactory (Figure10) and with high patient satisfaction.

Figure 10: Intramuscular buttock implants and fat transfer.
Sub-gluteal and sub-fascial pockets can also be utilised. The former always results in a high-positioned implant and unsightly result. The latter may cause capsular problems, skin thinning and trans-illumination. The intramuscular pocket is, therefore, preferred.
Peri-buttock liposuction and inter-zonal fat transfer
Preoperative marking is essential and liposuction using the Aquavage® system (Eurosurgical, UK) gives good volume of fat in a state ready for immediate transfer. Care must be taken when defining the lateral contour of zones four and five to preserve the mid lateral buttock ‘dimple’. The patient will need to be positioned in lateral and prone positions for harvesting the fat, particularly in zones one, two, seven and eight. Liposuction to zone three and defining the supra-gluteal contour obviously requires the patient to be prone.
The depth of fat harvest is from sub-scarpa fascia to avoid depressed contour defects. Large volumes of fat in excess of 500ml can be relocated by injecting into the gluteus maximus muscle and perimuscular tissues. Grade two or lesser ptosis will be immediately improved. Fat graft though is unpredictable and repeat grafts may be required. In massive weight loss patients ‘diced’ composite fat graft can be obtained from the pannus of the apronectomy and inserted using low volume syringes with large bore compliant catheters. MWL patients often have very little fat to harvest and this structured fat graft technique is a very good option for buttock augmentation (Figure 11).

Figure 11: Buttock augmentation with fat graft.
Summary
Buttock augmentation, particularly after weight loss, can improve ‘well-being’, confidence and help functionally to support clothing. Aggressive local tissue flap reconstructions are available but are largely unnecessary, are associated with considerable risk and invariably leave very poor visible scars.
Fat transfer to the buttock region is a safe and reasonable option in patients with mild buttock ptosis and zonal imbalance. Massive weight loss patients having large pannus excision can get quite acceptable results using structured fat graft techniques.
In naturally slim patients with very little body fat but no buttock shape the use of implants inserted intramuscularly offers a very reasonable chance of improvement and a satisfactory patient outcome.
References
1. Bartels R, O’Malley J, Douglas W, et al. An unusual use of Cronin breast prosthesis. Case report. Plast Reconstr Surg 1969;44:500.
2. Mendietta C. Classification system for gluteal evaluation. Clin Plastic Surg 2006;33:333-46.
3. Mendietta C. Intramuscular gluteal augmentation technique. Clin Plast Surg 2006;33:423-34.
4. Cuenca-Guerra R, Lugo-Beltran I. Beautiful buttocks: characteristics and surgical techniques. Clin Plast Surg 2006;33:321-32.
5. Centeno RF, Mendietta CG, Yaing VL.Gluteal contouring surgery in the massive weight loss patient. Clin Plast Surg 2008;35:73-91.
6. Salcedo JA de la P, Lopez-Salguero JF, Soto-Miranda MA. Buttock implants: gluteal implant augmentation. In Body Contouring and Liposuction. Edited by Rubin JP, et al. Elsevier Saunders; 2013:418-31.
7. Centeno R. Gluteal aesthetic unit classification: a tool to improve outcomes in body contouring.
Aes Surg J 2006;26:200-8.
8. Mendietta C. Buttock contouring with liposuction and fat injection. In Body Contouring and Liposuction. Edited by Rubin JP, et al. Elsevier Saunders; 2013:447-60.
9. Aboubib JH, Serra F, De Castro CC. Gluteal augmentation – technique, indications and implant selection. Plast Recontr Surg 2012;130(4):933-5.
Declaration of competing interests: None declared.