Rhinoplasty has changed considerably over the past one hundred years, not only in terms of the surgical techniques used, but also in the outcome desired by patients. There are now a large number of surgical techniques used which deal with the same or similar problems. Typically, the surgeon will choose a technique or techniques that they have been taught in their surgical education and possibly modified with subsequent experience.
As the popularity of facial plastic surgery operations in general, and rhinoplasty in particular, have increased, patients have also become much more aware of the possible benefits and undesired side-effects of the various surgical techniques. The free flow of information between patients allows for rapid reporting and comparison of results but at the same time there is unfortunately an increasing number of unsubstantiated or inappropriate claims against individual surgeons.
In this atmosphere of constant technical progress and increasing patient awareness, the provision of patient-specific surgery based on a tailor-made and unique set of surgical techniques has gained a position of primary importance. Repeating the same standard technique for every patient does not satisfy current patient needs, and sets the background for increased levels of revision surgery and unhappy patients.
The large numbers of variables that can affect the ultimate result need to be carefully considered in a systematic manner in order to achieve the outcome desired by each patient. As rhinoplasty involves a complex series of physical and psychological factors, a single consultation is rarely enough. The evolution of a tailor-made result depends on a gradual process of consultation and analysis of the individual situation, always keeping the risk benefit analysis in mind.


Figure 1: Preoperative (1a) and postoperative (1b) views of a young adult female patient. The patient requested a straight ‘aristocratic’ dorsum, well-defined radix and strong tip projection.


Figure 2: Preoperative (2a) and two-year postoperative (2b) views of a teenage female patient. The patient requested a slightly concave profile line (‘more feminine’). Radix and tip position were adjusted to aesthetically match the requested profile line, and the columellar-lip junction was subtly re-fashioned.
Patient-specific factors
A full and comprehensive ENT history and examination with a particular emphasis on rhinological problems is a mandatory first step in preparing the patient for surgery. However, specific points in the history are vital to the overall result. A detailed account of the patient’s wish list for change is noted. An unsatisfied patient with a history of previous rhinoplasty poses significant challenges for the surgeon: in these cases, extra attention to the patient’s physical and psychological factors is essential. The past medical history may reveal other diseases, such as diabetes and alternative medicines that may have an important impact on surgical planning.

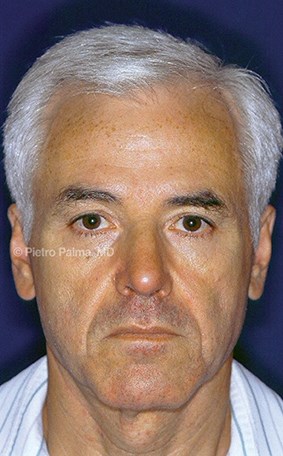
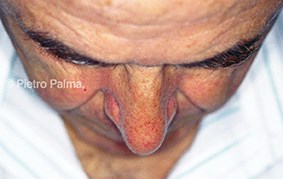
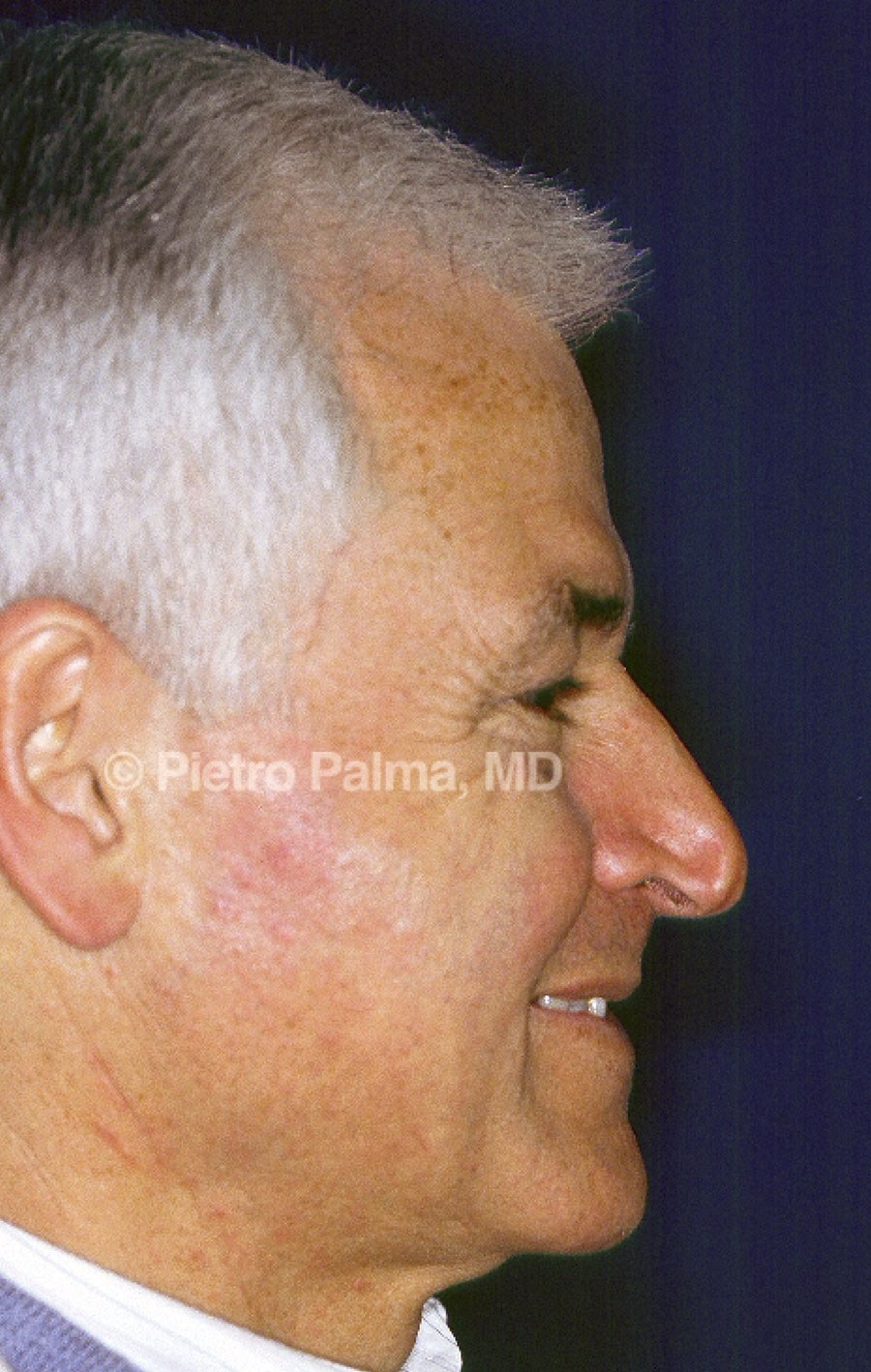
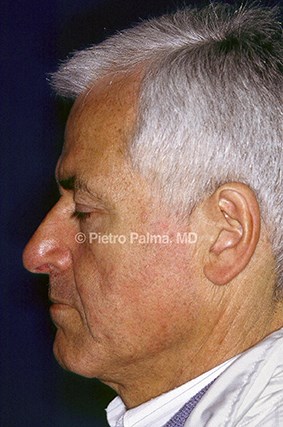
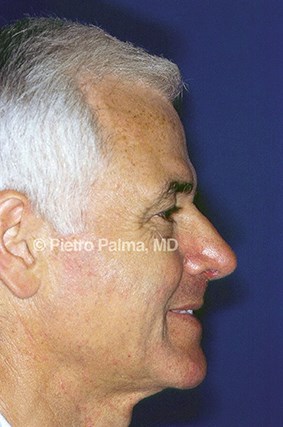
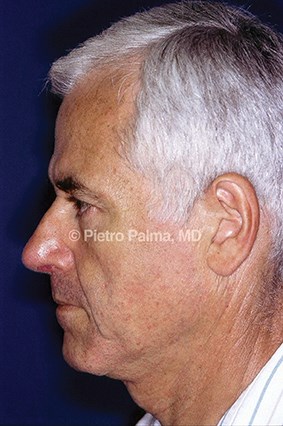
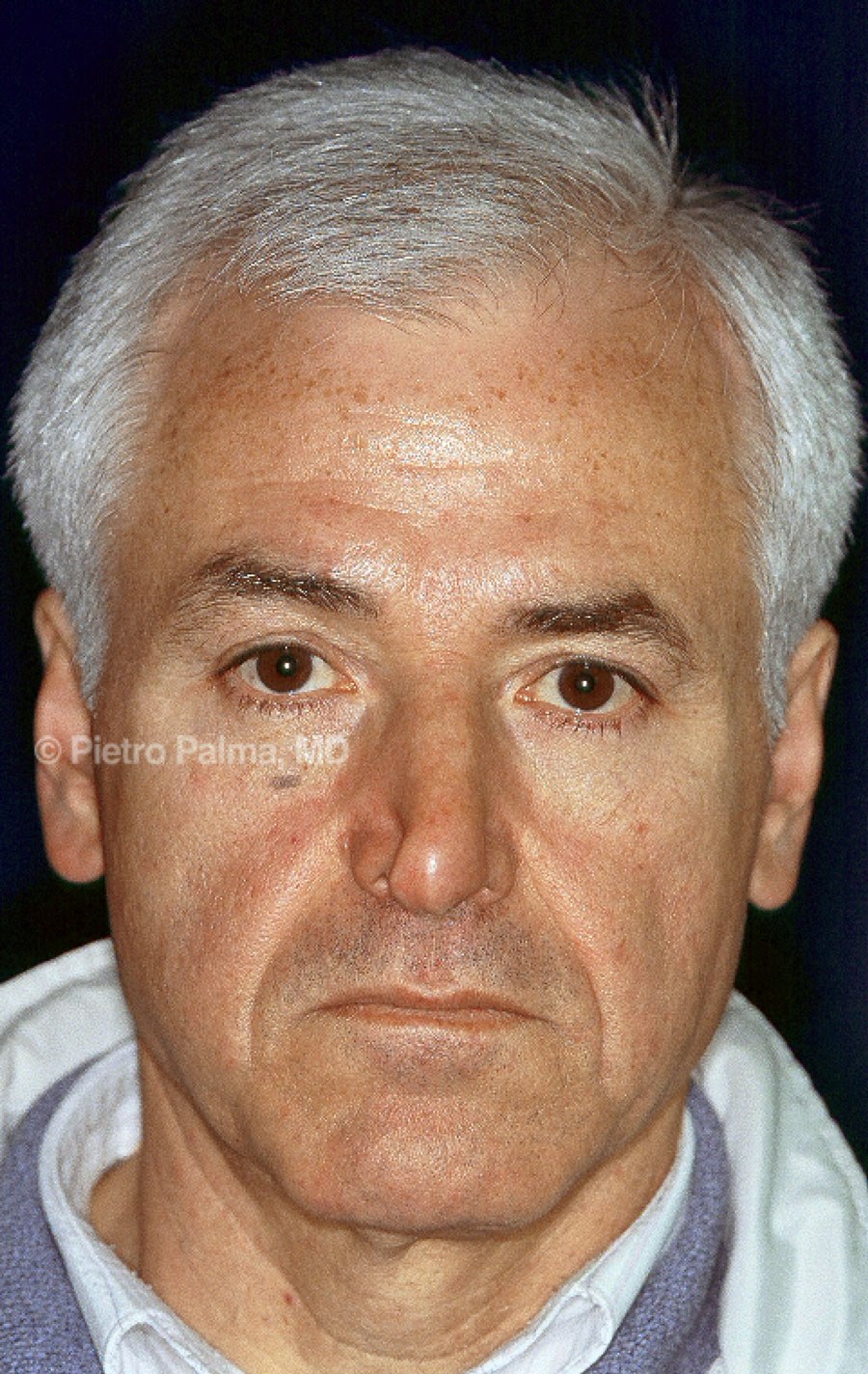
Figure 3: Preoperative (above) and one year postoperative (below) views of an elderly male patient. The support of lateral and middle crura was extensively rebuilt through an endonasal hybrid approach. Minimal changes to the dorsum height were accomplished. Tip position and nose-labial angle represent key elements in restoring nasal aerodynamics.
The technical aspect of endonasal surgery
The vast majority of patients presenting for cosmetic rhinoplasty neither desire nor require major reconstruction of the nose. Endonasal surgery implements major functional and aesthetic changes unique to each case. The major aims of the endonasal approach include: maintaining the structural integrity of the nose, preserving valvular function, and restoring or altering surface aesthetics. The emphasis rests on tissue preservation rather than excision, judicious use of grafts, and keeping the number of sutures to a minimum [8,9].
1. Age
1a. Children and teenagers
For many years performing rhinoplasty on children and teenagers has been considered unwise, as surgery on the growing nose has been considered to possibly interfere with long-term facial growth. While children are more prone to nasal injuries than adults, severe septal deformity leading to nasal obstruction is not very common. Current scientific evidence points to the safety of septoplasty in select cases where severe deformity is interfering with airflow. All cartilage that is removed should be returned to its appropriate position. Specific techniques have been developed in paediatric patients in order to increase success and safety rates of the procedure [1]. Indeed, leaving a severe septal deformity in a paediatric patient may have deleterious effects on the development of face and teeth later in life [2-5].
1b. Mature patients
As the average age of the population has been increasing with time, the number of requests for rhinoplasty from this age group has followed suit. Mature patients provide a unique set of specific physical and psychological challenges for the rhinoplasty surgeon. Although subtle signs of an ageing nose start in the second decade of life, most patients do not notice them until they are middle-aged [6]. With advancing years, the thinning of the nasal skin, and the decrease in volume of muscle, cartilage and bone, result in loss of tip support, tip ptosis, pseudohump, bony absorption of the maxilla and mandible, a relative increase in nasal size compared to the face. There is also diversion of airflow into the superior vestibule with subsequent valve problems [8-12].
These problems are usually of greater significance in men [7]. In female patients, thinner bones may already be involved by osteoporosis, making osteotomies more hazardous and requiring a much lighter touch. The bony vault regresses with age and becomes more fragile [13,14]. For these reasons, at times, it may be wisest not to perform osteotomies. Restoration of the nose to a more youthful appearance does not immediately translate into facial rejuvenation, as age estimation relies on several visual cues other than the nose, such as altered facial proportions due to loss of the hair line, and general loss in soft tissue volume. Nevertheless, correction of a ptotic tip, enhancement of the position / depth of the subnasal area through plumping grafts, combined with other subtle changes such as the use of neuromodulators and fillers can greatly improve the aesthetic balance of the face.
The requirements of rhinoplasty for the ageing nose include a wider subcutaneous elevation to compensate for the increased skin elastosis, more conservative excision – if any – of the tip cartilages, restoration of the columellar-labial angle with techniques such as tongue-in-groove, avoidance of removing too much cartilage from the pseudohump, and very conservative or no osteotomies [15]. With advancing years, the numbers of medical problems may accumulate, making an anaesthetic consultation for these patients obligatory.
An important psychological factor that sets the ageing rhinoplasty patient apart from younger patients consists of their emotional bonds to their parents and family through common and often valued facial features. Although a rhinoplasty may create a more youthful appearance it can also erase resemblance to the patient’s parents and create a source of significant emotional upset [16]. Furthermore, while most ageing rhinoplasty patients ask for a rhinoplasty after a positive life event, there are a significant number who seek to improve their life after a serious negative event, such as divorce, or death of a spouse. Clearly, the surgeon needs to clarify these points with sensitive counselling in order to avoid a very unhappy patient [17].
2. Sex
The sex of the patient may have a significant effect on the consultation process. For many years, surgeons have been warned about the MOSES (Male, Over expectant, Single, Eccentric, Self-lover) patient. Many patients with psychiatric conditions do not present in an obvious manner and recognising their problem requires experience and insight. However, if the doctor feels any sense of discomfort about a particular patient, the current advice is to defer / avoid surgery pending further clarification of the patient’s psychological state. Referring a patient to a psychiatric specialist is not common in our practice, but it is highly advisable in the obvious presence of warning signs.
It has also been suggested that male patients have a very ‘mechanical’ view of rhinoplasty, in that, very much like fixing a broken car, rhinoplasty is seen to be a simple, one-step fixing procedure at the mechanic’s workshop where the necessary repairs are done and a new, fully functioning car is delivered to the owner. In contrast, female patients learn from a very early age that looking more attractive requires several steps, which may lead to the occasional undesired result, and they generally have a greater acceptance of the limitations of surgery. While these generalisations tend to over-simplify the situation, it is generally true that more care needs to be taken of young male patients’ psychological needs.
In female patients, the relationship between menstrual cycle and perioperative loss had been a cause for concern, as it had been suggested that rhinoplasty around menstruation is associated with increased incidence of epistaxis. The effect of oestrogen and progestogens on nasal function has been firmly established, as many pregnant women in the third trimester will be troubled by nasal obstruction. However, recent studies do not show an increase in blood loss when rhinoplasty is performed in the perimenstrual period, however, there is a small increase in intraoperative blood loss in the peri-ovulatory period [18].
3. Facial analysis
Although the patient’s age and sex are significant in planning surgery, the most important step in creating a tailor-made game plan is practical and useful facial analysis. Good quality, standard photographs are computer analysed for modifiable surgical landmarks. Based on this analysis, a tailor-made surgical plan is created that is absolutely unique for that patient alone, and should not be repeated for someone else. The results of the analysis are presented to the patient in the second meeting. The interim period gives the patient and the surgeon time to adjust to each other and formulate the necessary questions.
Specific technical considerations in hybrid rhinoplasty
The hybrid rhinoplasty combines the best techniques from both the endonasal and the external approach to rhinoplasty that have evolved over the past century of surgical experience and scientific analysis. While utilising the endonasal approach to rhinoplasty, hybrid rhinoplasty is less traumatic to the nose than the external approach and allows for faster recovery times. In revision cases, especially when the nose has been operated on several times, the vascularity of the tissues and the quality of healing are both reduced. This makes tissue preservation and minimisation of trauma imperative. Patients care about the superficial appearance of the nose: the restoration of surface aesthetics is one of the main aims of hybrid rhinoplasty and precludes the obligatory structural reshaping of the nose through the external approach. However, a superficial problem may be due to deeper problems that have to be addressed. The patient-specific surgical plan acts as a guide in the operating room as it hangs directly in front of the surgeon’s field of vision along with the clinical photographs.
In primary cases, it is rare to find a perfectly symmetrical nose. The surgical plan will reflect this finding and guide the surgeon into performing asymmetric surgery. Osteotomies for example, are almost always performed asymmetrically. Similarly, cephalic trimming, refinements at the scroll areas and conservative superficial musculoaponeurotic system (SMAS) reduction are hardly ever equal on both sides.
While restoring surface aesthetics is one of the key aims of aesthetic rhinoplasty, it does not always require cutting and suturing of underlying cartilages. The key elements of an aesthetically pleasing nose, such as the brow-dome lines, or infra-tip break point can be re-fashioned with carefully placed crushed cartilage, often in an asymmetric manner. Thick SMAS patients pose a unique problem for the surgeon as vigorous excision of soft tissues creates marked stigmata of surgery and a highly undesirable outcome. The experienced surgeon may attempt very conservative, selective excision of the deeper layer of SMAS [19].
In cases with severe soft tissue damage to the nose where the quality of blood flow is questionable, it may be more prudent to avoid surgery and recommend a ‘medical’ rhinoplasty by an expert for filling of excessive tissue resection.
Conclusions
In planning a rhinoplasty for cosmetic and functional reasons, the astute surgeon needs to consider a large number of variables that can seriously affect the outcome. The growing science of facial plastics has led to the evolution of techniques making previously taboo subjects, such as operation of children, a thing of the past, whilst correcting deformities in the elderly now seems more complex with newer insights. Each patient presenting for a rhinoplasty is unique and requires a customised surgical plan that reflects the optimal matching of the wishes of the patient and a mature and honest assessment by the surgeon on how to deliver the desired outcome with the least risk of adverse events and complications.
References
1. Boenisch M, Nolst Trenitè G. Reconstructive septal surgery. Facial Plastic Surgery 2006;22:249-54.
2. Lawrence R. Pediatric septoplasy: a review of the literature. Int J Pediatr Otorhinolaryngol 2012:76(8):1078-81.
3. Tasca I, Compadretti GC. Nasal growth after pediatric septoplasty at long-term follow-up. Am J Rhinol Allergy 2011;25(1):7-12.
4. El-Hakim H, Crysdale WS, Abdollel M, Farkas LG. A study of anthropometric measures before and after external septoplasty in children: a preliminary study. Arch Otolaryngol Head Neck Surg 2001;127(11):1362-6.
5. Verwoerd CD, Verwoerd-Verhoef HL. Rhinosurgery in children: developmental and surgical aspects of the growing nose [Article in German] Laryngorhinootologie 2010;Suppl 1:S46-71.
6. Patterson CN. The aging nose: characteristics and correction. Otolaryngol Clin North Am 1980;13:275-88.
7. Rainsbury JW. The place of rhinoplasty in the ageing face. The Journal of Laryngology & Otology 2010;124:115-8.
8. Rohrich RJ, Hollier LH. Rhinoplasty with advancing age: characteristics and management. Otolaryngol Clin North Am 1999;32:755-73.
9. Krmpotic-Nemanic J, Kostovic I, Rudan P, Nemanic G. Morphological and histological changes responsible for the droop of the nasal tip in advanced age. Acta Otolaryngol 1971;71:278-89.
10. Parkes ML, Kamer FM. The mature nose. Laryngoscope 1973;83:157-62.
11. Patterson CN. The aging nose: Characteristics and correction. Otolaryngol Clin North Am 1980;13:275-84.
12. Winkler AA, Brian W. Aging male rhinoplasty. Facial Plast Surg Clin North Am 2008;16:329-35.
13. Rohrich RJ, Hollier LH. Rhinoplasty with advancing age: Characteristics and management. Clin Plast Surg 1999;32(4):755-73.
14. Pessa JE, Desvigne LD, Zadoo VP. The effect of skeletal remodeling on the nasal profile: Considerations for rhinoplasty in the older patient. Aesthetic Plast Surg 1999;23:239-45.
15. Rohrich RJ, Hollier jr LH, Janis JE, Kim J. Rhinoplasty with advancing age. Plast Reconstr Surg 2004;114(7):1936-44.
16. Goin MK. Psychological understanding and management of rhinoplasty patients. Clin Plast Surg 1977;4:3-7.
17. Shulman O, Westreich M, Shulman J. Motivation for rhinoplasty: changes in 5970 cases, in three groups, 1964 to 1997. Aesthetic Plast Surg 1998;22:420-4.
18. Findikcioglu K, Findikcioglu F, Sezgin B, et al. The impact of the menstrual cycle on intra-operative and postoperative bleeding in abdominoplasty patients. J Plast Reconstr Aesthet Surg 2012;65(12):e338-43.
19. Palma P, Khodaei I. Hybrid rhinoplasty: the 21st century approach to remodeling the nose. Arch Facial Plast Surg 2010;12(6):412-4.
Declaration of competing interests: None declared.