Non-melanoma skin cancers (NMSCs) are primary cutaneous neoplasms comprising mainly of basal cell carcinomas (BCCs) and squamous cell carcinomas (SCCs). In 2011, 102,628 cases of NMSCs (74% BCC and 23% SCC) were recorded in England, making NMSC the most common form of malignancy in the country [1]. The actual incidence of NMSCs is expected to be higher; it is estimated that 30-50% of cases of BCCs and SCCs go unrecorded. Treatment of actinic keratosis (AK) and Bowen’s disease (BD), both of which can progress to invasive SCC will also be discussed in this article.
Actinic keratosis
AKs are sun-induced skin lesions commonly found on sun-exposed sites of elderly, fairer-skinned individuals. They typically present as small, dry, red and rough patches of skin on the scalp, face, hands and lower legs (see Figure 1). Lesions can be itchy or tender. Treatment is often initiated to prevent the development of SCC. It is estimated that 60-97% of SCCs originate from AKs, though risk of progression of individual lesions remains low [2].
Bowen’s disease
Bowen’s disease (BD) is histologically characterised as SCC in situ. Clinically it tends to present as a discrete, scaly, erythematous patch or plaque, often affecting the lower legs in women and on the scalp and ears in men. Lesions may be confused with psoriasis or eczema.
Several aetiological factors of BD have been described; ultraviolet (UV) radiation, radiotherapy, arsenic ingestion, immunosuppression and human papillomavirus infection are associated with increased risks of developing BD. Development of a lump or ulcer, pain or bleeding within BD may indicate progression to SCC, which occurs in about 3-5% of cases [3].
Figure 1: Extensive actinic damage on the scalp with a small SCC on the frontal scalp.
Hypopigmented scarring is secondary to cryotherapy.
Basal cell carcinoma
BCC is typically a slow-growing NMSC which can present in various clinical forms – nodular, superficial, cystic, pigmented and morphoeic. The classic nodular BCC (nBCC) is a pink, shiny, telangiectatic nodule, with a rolled edge. It is associated with history of excessive sun exposure or frequent sun burn, and can sometimes be seen in inherited conditions such as Gorlin syndrome, Bazex-Dupré-Christol syndrome and xeroderma pigmentosum. Alterations in the hedgehog signalling pathway have been implicated in the development of both hereditary and spontaneous BCC, forming the basis of treatment with novel systemic agents.
Metastasis from BCC is very rare but tumours can be locally aggressive and may recur. High risk factors include site (central face, nose, lips and ears), histological subtypes (morphoeic, infiltrative and micronodular) and patient immunosuppression [4].
Keratoacanthoma and squamous cell carcinoma
Keratoacanthoma (KA) is often regarded as a self-healing variant of SCC, and can develop in sun-damaged, hair-bearing skin following minor injury. It is characterised by the presentation of a nodule with a history of rapid growth, followed by a static phase and subsequent resolution, leaving a puckered scar.
SCC often presents as a tender, crusted or ulcerated nodule with a shouldered edge. SCCs tend to develop in sun-exposed areas, such as the lips, ears, face, hands, forearms and lower legs. Apart from AK and BD, chronic leg ulcers or thermal scars can lead to an increased risk of developing SCC. SCCs developing in sites of chronic scars or inflammation are classified as high risk tumours. Other attributes of high-risk SCC include tumour size greater than 20mm, tumour site (lip, ear or non-exposed areas, e.g. perineum, sacrum, sole of foot), recurrent tumour, tumour thickness more than 4mm, moderate or poor histological differentiation, perineural invasion, acantholytic, spindle or desmoplastic histological subtypes, and patient immunosuppression.
Treatment
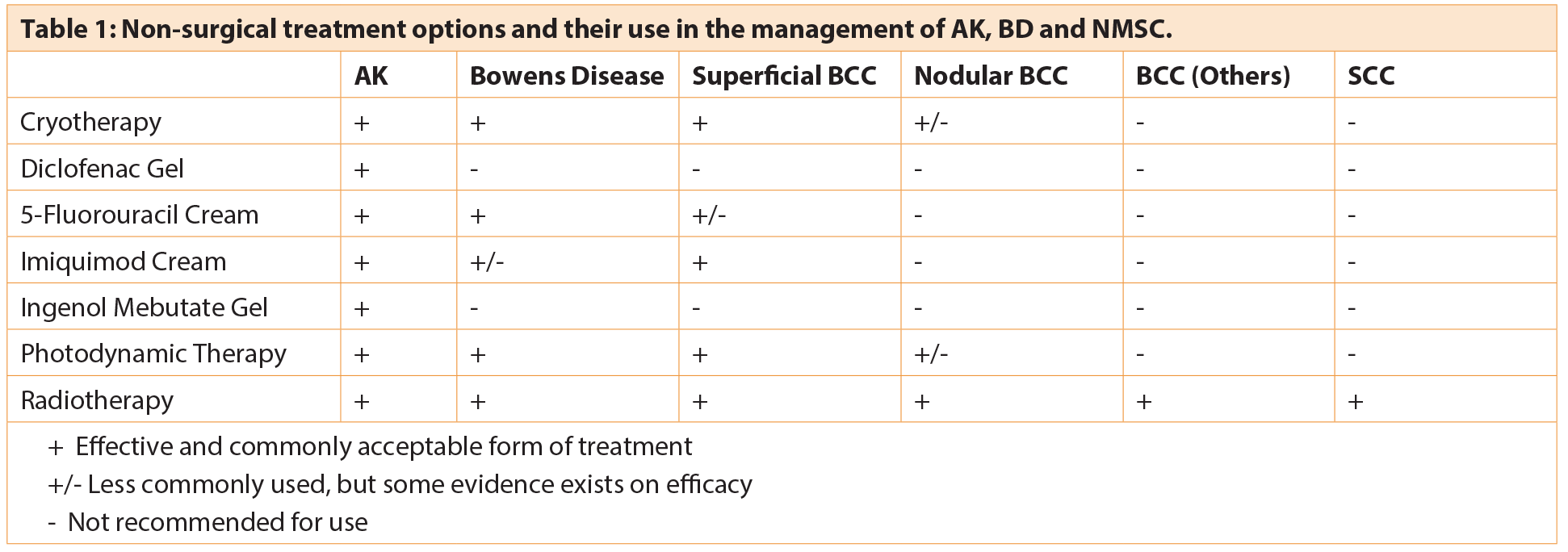
Surgical management remains the mainstay of treatment of BCC and SCC, with Mohs micrographic surgery often regarded as the gold standard of treatment for the former. However, in cases where tissue sparing or non-surgical treatment modalities are preferred, or in low-risk tumours, topical or non-invasive treatment options can sometimes be used. A range of different non-surgical treatment options exist for the treatment of AK, BD and some cases of NMSC; new agents continue to be developed and added to the list of choices available (see Table 1). Choice of treatment modality of NMSC is dependent on tumour risk stratification, patient preference or suitability, and availability of local services. Depending on the level of diagnostic certainty, pre-treatment skin biopsies for histological confirmation should be considered if not already performed, especially for risk stratification of BCC and SCC and when ablative treatment is being considered.
Cryotherapy
Cryotherapy involves the delivery of liquid nitrogen (temperature of -196°c) using cryospray, cryoprobe or a cotton-tipped applicator to the target tissue to induce cellular damage via a freeze-thaw cycle. Application time is measured in seconds from when an ice ball forms (lesion turns white). This is known as the freeze time, which can be highly variable, depending on the type of lesion treated. Two or more freeze-thaw cycles may be repeated, especially in the treatment of skin cancers.
Cryotherapy is usually used in treatment of AK, BD, superficial BCC (sBCC) and sometimes, small, nBCC. It is contraindicated in high-risk BCC due to lower cure rates, in SCC due to the risk of metastasis, and in melanocytic lesions. Cryotherapy should not be used on lesions near the eye margins, and care should be taken when treating lesions on the lower limbs of patients with peripheral oedema or diabetes mellitus, due to the risk of ulceration and delayed wound healing.
Acute complications of cryotherapy include pain and blister formation. These may be followed by delayed swelling, haemorrhage, ulceration and infection. Permanent complications include scarring, pigmentary changes and alopecia.
“Despite surgical treatment remaining the standard of care for the majority of NMSCs, non-surgical modalities are important in the management of pre-cancerous lesions, and can be appropriate alternatives in the treatment of malignant ones.”
Diclofenac gel
Diclofenac in hyaluran gel (SolarazeTM) is often used in the community to treat AK and is generally accepted to be well tolerated by patients, with the main side-effect being mild skin irritation. It is proposed to reduce angiogenesis and cellular proliferation via inhibition of cyclo-oxygenase-2, and upregulates apoptosis. It can be used for field treatment of AKs, and is applied twice daily for 90 days. However, it is the authors’ experience that clinical results tend to be disappointing in clinical practice.
5-fluorouracil
5-fluorouracil (5-FU) is a pyrimidine antimetabolite that inhibits DNA synthesis and is commonly used as a topical chemotherapeutic agent in the treatment of AK and BD. Complete AK clearance rates of 43-100% have been reported [5]. There is limited published evidence on the success rate of 5-FU in the treatment of superficial (aBCC), but a small study has found 90% histological cure rate at 16 weeks [6]. Preparations include 5% 5-FU cream (EfudixTM) and 0.5% 5-FU with 10% salicylic acid (ActikerallTM), which is useful for the treatment of hyperkeratotic AK. Variable treatment regimens exist for the use of 5-FU cream, and it is generally recommended to be used twice daily for two to three weeks for lesions on the face and scalp. Treatment courses may be longer for lesions on other sites.
Side-effects of 5-FU include redness, pain, crusting, infection and risk of ulceration. Topical hydrocortisone preparations are often prescribed at the outset to be used at the end of the treatment course to relieve associated inflammation. Written instructions and adequate warning of side-effects can improve compliance of treatment. Care should be taken when prescribing 5-FU for use by elderly, frail patients, on lesions on the lower limbs, or in patients with diabetes mellitus or peripheral vascular disease.
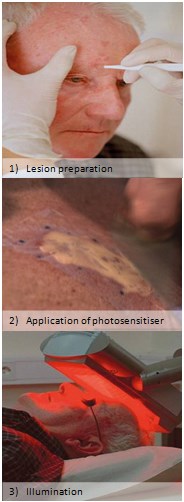
Figure 2: PDT treatment procedure.
Imiquimod
Imiquimod (AldaraTM) is a topical immune response modifier, and stimulates both the innate and adaptive cell-mediated immune pathways, via toll-like receptors expressed on Langerhans cells to produce anti-tumour effect. In the UK, it is licensed for the treatment of AK and sBCC, but evidence of its efficacy in the treatment of BD exists.
For treatment of AK, imiquimod is licensed for prescription three times a week for four weeks, to be repeated after four weeks if necessary (response rate of 84% was reported in a study when used continuously for 12 weeks [7]). For sBCCs, imiquimod is used five times a week for six weeks; assessment of patients following this regime for treatment of small sBCCs demonstrated a histological clearance rate of 82% at 12 weeks [8]. A study of once-daily application of imiquimod on BD over 16 weeks demonstrated histological clearance rates of 73% [9]. It is not uncommon for patients with extensive actinic damage to present with multiple lesions of AK, BD and sBCC, which can all appear clinically very similar. It is often more practical for patients to be prescribed one form of either topical 5-FU or imiquimod for treatment of all suspicious lesions at the same time.
Potential side-effects are similar to that seen in the use of 5-FU; flu-like symptoms and regional lymphadenopathy are sometimes seen.
Ingenol mebutate
Ingenol mebutate (PicatoTM) is derived from the plant Euphorbia peplus, also known as milkweed. It is currently licensed in the UK as a treatment for AK. Preparations of 0.015% are prescribed once daily for three consecutive days for lesions on face and scalp. The stronger 0.05% preparations are prescribed once daily for two days for lesions on the trunk and extremities. The specific mechanism of action of ingenol mebutate remains uncertain. It is said to have a dual mode of action, first by targeting dysplastic keratinocytes and leading to rapid cell necrosis, then by inducing neutrophil infiltration and facilitating antibody-dependent cellular cytotoxicity.
When assessed at 57 days, complete clearance of lesions was seen in 42.2% of cases treated for face and scalp lesions, and 34.1% of cases treated for lesions on the trunk and extremities [10]. The ease of use of ingenol mebutate gel can lead to improved compliance among patients. Application-site reactions peak the day after completion of treatment, and often include symptoms of redness, crusting, pruritus, irritation and pain.
Photodynamic therapy
In photodynamic therapy (PDT), a photosensitising drug is applied to the treatment site and subsequently activated by visible light (see Figure 2). This leads to the production of reactive oxygen species that destroy cells in the targeted site. 5-aminolevulinic acid (ALA) and its more lipophilic esterified derivative, methyl 5-aminolevulinate (MAL), are the common photosensitisers of choice today. The light source of PDT chosen is based on its wavelength, which should match the absorption wavelength of the sensitiser, and its ability to penetrate the desired depth of the treated tissue. Normally, red light (635 nm) is used, which can achieve a penetration depth of around 8-10mm.
PDT is often considered an effective first-line treatment choice for the treatment of AK and BD. Clinical clearance rates of BD treated by PDT were reported to be >88% at three months [11]. Compared to cryotherapy, 5-FU or imiquimod, PDT is probably more appropriate and better tolerated as a treatment for larger lesions (>3cm diameter), with two treatments of MAL-PDT, scheduled one week apart, clearing 96% of larger BD lesions at three months [12].
PDT is also used for the management of primary sBCC, with double-cycle ALA-PDT achieving initial clearance rates of about 90-95% [4]. It addition, it is increasingly being recognised as a potential treatment modality for primary, low-risk nBCC. Reports of the use of MAL-PDT in the treatment of non-facial nBCC have demonstrated clinical clearance of 91% at three months [13]. There is insufficient evidence to support the routine use of topical PDT for recurrent or infiltrative BCC, or SCC.
Pain, mild swelling, crusting and erosions are some of the commonly reported side-effects of PDT. Compared with cryotherapy and surgery, PDT often yields a better cosmetic outcome with increased patient satisfaction. However, it can be more time-consuming, requiring visits to specialist units, and correspondingly less cost-effective compared to other non-invasive treatment modalities for NMSCs.
Radiotherapy
Radiotherapy (RT) is the use of radiation to treat cancer by directing high energy radiation (typically X-ray) to target and destroy cancer cells. It tends to be given on an outpatient basis, requiring a number of visits to a specialist oncology centre. RT can be considered in the treatment of primary or recurrent BCC (except when previously treated with RT) in cases where patients are unwilling or unable to undergo surgery. It may also be used as an adjuvant therapy in incomplete excisions of high-risk BCCs. Five-year cure rates of >90% have been reported in the treatment of primary and recurrent BCC [4]. Good outcomes have been demonstrated on various facial sites, e.g. nose, lip, ear and peri-orbital skin. However, care should be taken when treating lesions on the dorsum on the hand, abdomen, or lower limbs, which involve higher risk of adverse effects such as ulceration.
RT is the only non-surgical treatment option for SCC with sufficient evidence supporting its role. Curative rates of >90% of cases have been reported [14].
Acute and chronic radiation dermatitis, scarring with pigmentary changes, skin atrophy, telangiectasia, hair loss and ulceration are some of the reported side-effects in RT. It also carries an increased risk of a second cancer developing in the treated site. However, this may be less relevant to the elderly population, who form the majority of patients referred for radiotherapy for NMSC.
Vismodegib
Vismodegib is a novel hedgehog signalling pathway inhibitor approved for use in the treatment of symptomatic, metastatic BCC, or advanced local disease not suitable for treatment by surgery or radiotherapy.
A dose of 150mg once daily is prescribed. A multi centre study conducted in the USA analysed 119 patients who took vismodegib over a median period of 5.5 months. A total of 46.4% of patients with locally advanced BCC and 30.8% of patients with metastatic BCC demonstrated some response to treatment. Stabilisation of disease was achieved in 48.2% and 51.3% of cases of locally advanced and metastatic BCC, respectively [15].
Potential side-effects include muscle spasm, altered taste, alopecia, diarrhoea, nausea, fatigue and weight loss. It is contraindicated for use in pregnancy due to risk of teratogenicity.
Conclusion
NMSCs are among the most common malignancies in the UK, demonstrating a trend of increased incidence over the past decades. Despite surgical treatment remaining the standard of care for the majority of NMSCs, non-surgical modalities are important in the management of pre-cancerous lesions, and can be appropriate alternatives in the treatment of malignant ones. A variety of non-surgical treatment options are available, and novel agents have been introduced in recent years, expanding the range of options available to patients. Health practitioners should familiarise themselves with the different agents available, in order to help patients reach an informed decision on the choice of treatment modality most appropriate for each individual.
References
1. Cancer Research UK. Skin cancer incidence statistics.
http://www.cancerresearchuk.org/
health-professional/cancer-statistics/
statistics-by-cancer-type/skin-cancer/incidence
Last accessed September 2015.
2. Ceilley RI, Jorizzo JL. Current issues in the management of actinic keratosis. J Am Acad Dermatol 2013;68(Suppl 1):S28-38.
3. Neubert T, Lehmann P. Bowen’s disease – a review of newer treatment options. Ther Clin Risk Manag 2008;4(5):1085-95.
4. Telfer NR, Colver GB, Mortion CA. Guidelines for the management of basal cell carcinoma. Br J Dermatol 2008;159:35-48.
5. Kaur RR, Alikhan A, Maibach HI. Comparison of topical 5-fluorouracil formulations in actinic keratosis treatment. J Dermatolog Treat 2010;21(5):267-71.
6. Romagosa R, Saap L, Givens M, et al. A pilot study to evaluate the treatment of basal cell carcinoma with 5-fluorouracil using phosphatidyl choline as a transepidermal carrier. Dermatol Surg 2000;26:338-40.
7. Stockfleth E, Meyer T, Benninghoff B, et al. A randomized, double-blind, vehicle-controlled study to assess 5% imiquimod cream for the treatment of multiple actinic keratoses. Arch Dermatol 2002;138:1498-502.
8. Geisse J, Caro I, Lindholm K, et al. Imiquimod 5% cream for the treatment of superficial basal cell carcinoma: results from a randomized vehicle-controlled phase III study in Europe. Br J Dermatol 2005;152:939-47.
9. Patel GK, Goodwin R, Chawla M, et al. Imiquimod 5% cream monotherapy for cutaneous squamous cell carcinoma in situ (Bowen’s disease): a randomized, double-blinded, placebo controlled trial. J Am Acad Dermatol 2006;54:1025-32.
10. Lebwohl M, Swanson N, Anderson LL, et al. Ingenol mebutate gel for actinic keratosis. N Engl J Med 2012;366:1010-9.
11. Morton CA, Birnie AJ, Eedy DJ. British association of dermatologists’ guidelines for the management of squamous cell carcinoma in situ (Bowen’s disease) 2014. Br J Dermatol 2014;170:245-60.
12. Lopez N, Meyer-Gonzalex T, Herrera-Acosta E, et al. Photodynamic therapy in the treatment of extensive Bowen’s disease. J Dermatog Treat 2012;23:428-30.
13. Rhodes LE, de Rie M, Enstrom Y, et al. Photodynamic therapy using topical methyl aminolevulinate vs surgery for nodular basal cell carcinoma. Results of a multicenter randomized prospective trial. Arch Dermatol 2003;140:17-23.
14. Motley R, Kersey P, Lawrence C. Multiprofessional guidelines for the management of the patient with primary cutaneous squamous cell carcinoma. Br J Dermatol 2002;146(1):18-25.
15. Chang AL, Solomon JA, Hainsworth JD, et al. Expanded access study of patients with advanced basal cell carcinoma treated with the Hedgehog pathway inhibitor, vismodegib. J Am Acad Dermatol 2014;70(1):60-9.
Declaration of competing interests: None declared.
TAKE HOME MESSAGE
-
Pre-malignant and malignant skin tumours are extremely common, especially on the face.
-
There are a range of non-surgical treatment options available.
-
Choosing the correct option depends on multiple factors and patients should be involved in choosing the most appropriate treatment modality.
COMMENTS ARE WELCOME