The authors detail the types of lasers and light-based devices that can be used in the treatment of epidermal and dermal pigmentations.
Skin colour differences have, for centuries, been associated with the economic, political and social status of a person; therefore, the appearance of a new pigmentation may imply a negative, emotional and psychological state. Non-white racial / ethnic groups (African-Americans, Hispanics and Asians) often seek medical procedures for the removal of pigmentation disorders due to the greater incidence of congenital and acquired pigmentary disorders among these groups.
These epidermal pigmentations are characterised by the melanin content in the epidermis or dermo epidermal junction:
- Ephelides
- Solar lentigo
- Lentigo simplex
- Seborrheic keratoses
- Dermatosis papulosa nigra
- Cafè-au-lait macules
- Naevus spilus
Dermo epidermal lesions show the melanin pigment at the epidermal and dermal position:
- Post inflammatory hyperpigmentation
- Melasma
- Becker’s naevus
- Junctional and compound melanocytic nevi
- Congenital melanocytic nevi
Dermal pigmented lesions are due to a deeper melanin in the dermis:
- Blue naevi
- Naevus of Ota
- Naevus of Ito
Lasers and light-based pigment removal: how they work
The majority of lasers used in medicine, and mainly in dermatology, generate light in the ultraviolet (200-400nm), visible (400-760nm), near-infrared (760-1400nm), mid-infrared (1400-3000nm) and infrared (> 3000nm) wavelengths. The typical features of laser light are its monochromaticity, coherence and collimation and these characteristics differentiate laser light from non-laser light, such as intense pulsed light (IPL). The absorption of photons by a specific target is the scope of every laser treatment in order to cause a biological effect; during this process all the energy delivered by the photons is transmitted to the target structures, the chromophores. Dermatological laser treatment changed radically in 1983 thanks to the introduction of the selective photothermolysis theory by Anderson and Parrish, defining how to localise thermal injury to the target tissue, thus minimising the damage to surrounding areas by choosing the adequate wavelength of light that the chromophore inside the target tissue absorbs.
The absorption depends mainly on the matching of the wavelength of the photons with the absorption peak of a particular chromophore. The absorption by melanin, ranging between 400 and 750nm, is maximal in the ultraviolet area, decreasing throughout the visible region.
The light absorption can cause three different types of biological effects in the skin: photomechanical, photothermal and photochemical. The photomechanical effect occurs when very short laser pulses, nanoseconds for the Q-switched laser or picoseconds for the picosecond laser, produce very strong energies; in this way the tissue undergoes rapid thermal expansion, and an optical breakdown with intense shockwaves. This photomechanical effect is crucial for Q-switched lasers and picosecond lasers that are able to disrupt the melanin and ink content of hyperpigmentation and tattoos (fragmentation of intracellular pigment into extracellular granules subsequently phagocytised by macrophages), as well as being a determining factor for high-fluence, short-pulse, pulsed dye laser treatment of vascular disorders. In fact, photomechanical damage, which clinically appears with purpura, is induced by short pulses and causes intravascular cavitation, vessel wall rupture and haemorrhaging.
The photothermal effect occurs when the energy of the irradiated photons is turned into heat due to the absorption of the photons by the chromophores. The consequences may vary depending on the degree of heating reached in the target chromophore, the duration of the target at that temperature, and lastly, the capacity to spread the heat to the surrounding tissues. The photochemical effect occurs when the absorbed photons affect the cellular metabolism or influence the signaling cascade. The consequences of the photochemical effect include increased cell proliferation and migration, modulation of growth factors, cytokines and other mediators, increased tissue oxygenation, and increased healing of wounds.
Several laser and light devices are available on the market for treating pigment alterations: Q-switched neodymium-doped:yttrium aluminium garnet laser (Nd:YAG) (532-1064nm), pulsed dye laser (PDL) (595nm), Q-switched ruby laser (694nm), Q-switched alexandrite laser (755nm), picosecond alexandrite laser (755nm), intense pulsed light (IPL) (590-1200nm), as well as nonselective lasers, erbium:YAG laser (2940nm) and carbon dioxide laser (CO2) (10600nm) through its fractional modality too [1-8].
Lasers and lights
Q-switched 532 nm Nd-YAG laser is the shortest wavelength laser employed for pigmented disorders removal (Figures 1-2). It is effective for superficial epidermal pigmentations like solar lentigines and freckles. The treated lesion is characterised by the appearance of a typical pinpoint bleeding and a haemorrhagic crust which lasts five to six days before falling off.

Figure 1: Top) A 49-year-old female patient with solar lentigo on the left cheek. Bottom) The disappearance of the most part of the solar lentigo after only one session of Q-switched 532nm Nd:YAG laser (SYNCHRO QS4, DEKA M.E.L.A., Calenzano, Italy).

Figure 2: Top) The typical brownish lentigos of the hands in a 63-year-old patient. Middle) The post-procedure erythema on the areas treated by Q-switched 532nm Nd:YAG laser (SYNCHRO QS4, DEKA M.E.L.A., Calenzano, Italy). Bottom) The results achieved after one session.
PDL uses a rhodamine dye dissolved in a solvent and pumped by a flash lamp, emits a 585-600nm wavelength yellow light, near the haemoglobin absorption peak, and therefore it is considered the most specific laser currently available for the treatment of superficial vascular lesions. It is also commonly used for treating Poikiloderma of Civatte and really superficial pigmented lesions like solar lentigines and ephelides, since its wavelengths are absorbed by melanin too (Figure 3). Despite its excellent efficacy and safety profile, the onset of purpura would limit patients’ acceptance as it may persist for 7 to 14 days after the laser session due to micro vaporisation of erythrocytes, vessel rupture and subsequent haemorrhage; a pressure diascopy during the PDL session removes the blood from the vessels by closing the vessel lumen, and the removal of vascular component of the lesion avoids the purpura after the PDL session for treating lentigines.

Figure 3: Top) a 44-years-old female patient with a diffuse photoaging. Bottom) remarkable improvement after two sessions of Fractional CO2 laser (SmartXide2 DOT/RF, DEKA M.E.L.A., Calenzano, Italy)
Q-switched ruby laser emits a 694nm beam of photons, being well absorbed by melanin and minimally by haemoglobin. It is effective for the removal of superficial pigmentations, lentigines, ephelides and pigmented actinic keratosis as well as deeper pigmented lesions, melanocytic naevi, naevus of Ota, naevus of Ito.
Q-switched alexandrite emits at 755-nm, belonging to the near-infrared category of lasers. At this particular wavelength the main chromophore is melanin, hence it is mainly used for hair removal and pigmented lesions. Since alexandrite has a similar wavelength with ruby laser, it shares the same pigmented indications; the longer wavelength allows a deeper effect on dermal melanin in fact its employment gives excellent results for nevus of Ota.
Picosecond alexandrite laser is a safe and effective modality for the removal of pigmentary disorders. Due to its great success in tattoo removal, several physicians have started to employ it for treating different pigmentations with promising results. Its effectiveness results from a greater pigment fragmentation induced by deep shockwaves (photomechanical effect), while its safety originates from a reduced and selective thermal damage (photothermal effect). As it targets the pigment through shorter picosecond pulses this kind of laser has the ability to achieve the same results as a Q-switched laser but through less sessions. The reduction of the number of laser sessions implies a shorter post-treatment downtime for the patients, who are able to better tolerate all the procedures.
Q-switched 1064nm Nd-YAG laser produces light in the infrared part of the spectrum at a wavelength of 1064nm. Melanin does not absorb this wavelength well, and for this reason the 1064nm Nd:YAG laser is not considered optimal for the removal of pigmented lesions. Its advantage results from the capability to penetrate deeper into the skin, up to 5-7mm; therefore its indications are deep pigmented disorders like naevus of Ota and tattoos. Patients usually complain of more discomfort and a prolonged downtime.
IPL technology uses a xenon broadband flash lamp to generate non-coherent light in a spectrum between visible and near infrared (500-1300nm). To reach the desired chromophore, filters cut the light emission according to the wavelengths required by the physician; consequently, this type of light source can excite more than one chromophore (haemoglobin, melanin, water). Its versatility entails a reduced selectivity. Handpieces have a large surface area, generally cooled, and application of gel on the skin surface is required during the procedure. For the treatment of pigmented lesions IPL is not comparable with Q-switched lasers since its pulse duration in the milliseconds range make it a second choice. IPL employment can give excellent results when the pigmentations are matched with vascular lesions (teleangiectasias, erythrosis, rosacea).
Er:YAG laser is a solid-state laser, characterised by the presence of erbium ions inside ytrrium-aluminum-garnet or other crystals; it emits photons at wavelengths of 2940nm, which are mainly absorbed by water in the superficial layers of the skin. This laser system is generally used for ablating the soft and hard tissues. Its main drawback compared to other ablative lasers like CO2 is its inability to coagulate. Er:YAG laser can be used for skin resurfacing with a fractional handpiece in a minimally ablative manner too.
CO2 is a gas-state laser that emits photons at wavelengths of 10600nm. It offers a type of ‘no-contact surgery’. In fact, this laser system enables precise, efficacious and targeted thermal action on the lesions treated while protecting the surrounding tissues, thus guaranteeing optimal re-epithelisation. This makes it suitable for surgical procedures since the limited inflammatory response is conducive to better healing. The extreme precision of the application means that the epidermis alone can be vaporised, or the thermal effect can be extended even deeper into the papillary or reticular derma. The use of ‘colour indicators’ allows for step-by-step visual assessment of the level reached and an accurate calculation of the clinical ‘end-point’ phase. Ablative resurfacing with CO2 laser has been considered the gold-standard for many years in the treatment of wrinkles, and skin damage from photoageing. These skin resurfacing lasers (Er:YAG and CO2) can be employed for removing superficial pigmented lesions like lentigo simplex, solar lentigo, seborrheic keratoses, and dermatosis papulosa nigra.
Fractional CO2 laser is equipped with a scanning system which makes it possible to obtain vertical micro-columns of damage, micro-ablative and micro-thermal zones (MAZs and MTZs), surrounded by areas of healthy tissue. Depending on the pulse used, the controlled release of heat in the treated micro-areas has an immediate tissue-shrinking effect and generates the stimulation of growth factors, wound repair, and the reorganisation of new collagen. Another feature which increases the versatility of this application is the possibility of selecting the distance (DOT spacing) between surrounding MAZs and MTZs, providing a resurfacing effect similar to the ablative technique with reduced spacing, or the more typical fractional effect, with greater spacing between DOTs. Each treatment session consists of numerous successive and consecutive pulses [1-5] in the same point without moving the scanner (‘scalpel effect’).
Therapeutic steps
1. Clinical features
The main features to be evaluated are the skin phototypes. Racial genetics play a significant role in determining a patient’s response to any skin laser treatment. Contrary to traditional skin classifications (the six Fitzpatrick types), the new genetic-racial classification takes into consideration the racial origins of patients rather than their skin colour alone. Indo-Pakistani, African and Asian, Aboriginal and Mixed race patients have a higher tendency to develop hypo and above all post-inflammatory hyperpigmentation (PIH) than European, Nordic and Mediterranean.
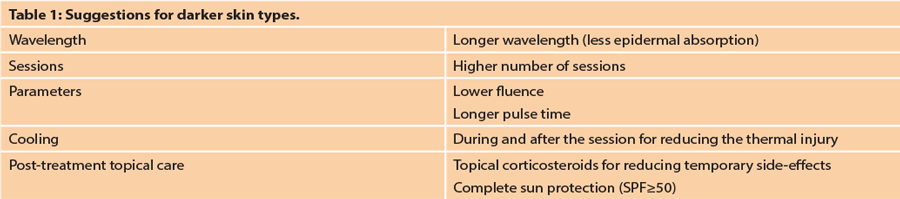
The treatment of these high-risk candidates requires management by expert hands, the correct instruments and within the proper parameters (Table 1) [9-13]. Nowadays, the knowledge of the patient’s racial origin, and that of parents and grandparents, should always be matched with a detailed ‘skin imaging report’ to determine appropriate laser treatment modalities. High performance 3D imaging systems provide life-like high quality 3D reconstruction images (such as 3D LifeViz®, Quantificare, Valbonne, France). These systems include an image management software with superior photo documentation capabilities to visualise, analyse and archive 3D images. With the 3D analysis module, users can detect and precisely quantify subtle features quickly and easily.
2. Selection of the parameters
Once the correct laser has been selected, the physician must decide on the most appropriate parameters, such as wavelength, spot size, fluence and pulse duration. The wavelength has to be chosen by considering the main chromophore inside the lesion, as well as its light absorption peak and depth. A Q-switched laser at 532nm is able to remove the superficial pigment of a brownish lentigo, whereas only if used at 1064nm can it remove black tattoo ink. The spot size should match the diameter of the target structure as closely as possible to minimise damage to the surrounding tissues. The fluence can be considered as the energy per unit area, and it is inversely proportional to the fraction of light absorbed by the target chromophore. Increased fluence must be used with chromophore-poor targets, deep skin targets and targets which barely absorb the wavelength.
At the beginning of the first treatment session the dermatologist should choose the fluence according to the patient’s pain threshold and in view of the clinical endpoint of that particular laser in use. The last parameter to be selected is the pulse duration, which is determined by the thermal relaxation time (TRT) of the target, that is, the time the tissue takes to lose half the acquired heat which is proportional to the square of the target’s diameter; the TRT of a larger structure will be longer than the TRT of a smaller structure. The pulse duration must be shorter than or equal to the TRT in order to limit the damage to the target tissue. If the duration is too short it could imply a loss of efficacy, whereas if the pulse is longer than the TRT the heat will spread to the surrounding structures, with the risk of possible scarring and other texture changes.
3. Performing the procedure
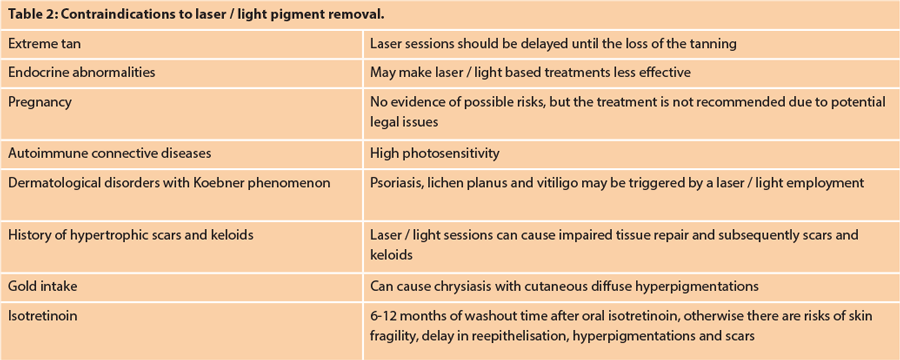
Before beginning with the laser session, it is very important to document a complete medical history of the patient, to identify any possible contraindications. There may be a reason that the patient cannot be treated (Table 2). A detailed photo documentation prior to each laser procedure is necessary for showing the results achieved and for potential legal medical issues. The patients should always be informed about the practical aspects of the session, giving them realistic expectations about the results. Moreover, they should receive written information about possible side- effects and post-procedure woundcare.
The physician must always begin with a test on a small part of the pigmented lesion, and continue the full treatment only if it is safe and effective. In our opinion melanocytic lesions should not be treated, since these treatments could impede or delay the correct diagnosis of malignancy; also the histological examination through a biopsy may not be enough to exclude an early malignant pigmented lesion. During the treatment, the laser / light emission should always be matched with a cooling system, which is important for all phototypes, but it becomes particularly necessary in patients with more epidermal melanin. Cryogen spray, cold air and direct contact cooling are commonly employed in combination with lasers and IPL.
Possible side-effects
The most common cutaneous reactions include erythema, oedema and discomfort up to pain, though more severe side-effects such as thermal burns, blisters, purpura, hyperpigmentation, hypopigmentation, atrophia, scarring and infections rarely occur. The most severe side-effects manifest in darker-skinned patients and these could be avoided by the selection of safer parameters, an effective cooling process during the session and the employment of correct post procedure care. The patient must always remember to avoid sun exposure and to apply sunscreen during the days following the session, as well as a topical steroid for three to five days to eliminate common erythema.
Conclusions
According to previous comparative studies, all the laser and light-based systems for pigmented lesion removal were revealed to be safe and efficacious if employed by experienced practitioners. These systems only vary according to the discomfort felt by the patient, and the possibility of treating darker-skinned patients and deeper lesions. New laser systems include the picosecond alexandrite systems which have achieved promising results not only for tattoo removal but also for many other pigmented disorders. Clinical studies and long-term data will be necessary to determine the effectiveness and the safety of these modalities for the future.
References
1. Jones CE, Nouri K. Laser treatment for pigmented lesions: a review. J Cosmet Dermatol 2006;5:9-13.
2. Polder KD, Landau JM, Vergilis-Kalner IJ, et al. Laser eradication of pigmented lesions: a review. Dermatol Surg 2011;37:572-95.
3. Goldberg DJ. Laser removal of pigmented and vascular lesions. J Cosmet Dermatol 2006;5:204-9.
4. Kilmer SL. Laser eradication of pigmented lesions and tattoos. Dermatol Clin 2002;20:37-53.
5. Levin MK, Ng E, Bae YSC, et al. Treatment of pigmentary disorders in patients with skin of color with a novel 755-nm picosecond, Q-switched Ruby, and Q-switched Nd:YAG nanosecond lasers: a retrospective photographic review. Lasers Surg Med 2016;48:181-7.
6. Petersen DT, Erlendsson AM, Nash JF, et al. Side effects from Intense Pulsed Light: importance of skin pigmentation, fluence level, and ultraviolet radiation – A randomized controlled trial. Lasers Surg Med 2017;49:88-96.
7. Babilas P, Schreml S, Szeimies RM, Landthaler M. Intense Pulsed Light (IPL): A Review. Lasers Surg Med 2010;42:93-104.
8. Watanabe S, Takahashi H. Treatment of nevus of Ota with the Q-switched Ruby laser. N Engl J Med 1994;331:1745-50.
9. Alexis AF. Lasers and light-based therapies in ethnic skin: treatment options and recommendations for Fitzpatrick skin types V and VI. Br J Dermatol 2013;169(Suppl3):91-7.
10. Kono T, Shek SY, Chan HHL, et al. Theoretical review of the treatment of pigmented lesions in Asian skin. Laser Ther 2016;25(3):179-84.
11. Chan JC, Shek SY, Kono T, et al. A retrospective analysis on the management of pigmented lesions using a picosecond 755-nm alexandrite laser in Asians. Lasers Surg Med 2016;48:23-9.
12. Lee SE, Choi JYC, Hong KT, Lee KR. Treatment of acquired and small congenital melanocytic nevi with combined Er:YAG laser and Long-pulsed Alexandrite laser in Asian skin. Dermatol Surg 2015;41:473-80.
13. Suh DH, Han KH, Chung JH. The use of Q-switched Nd:YAG laser in the treatment of superficial pigmented lesions in Koreans. J Dermatol Treat 2001;12:91-6.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME