AESTHETIC FOCUS
Plasma: An ionised gas consisting of positive ions and free electrons in proportions resulting in more or less no overall electric charge, typically at low pressures (as in the upper atmosphere and in fluorescent lamps) or at very high temperatures (as in stars and nuclear fusion reactors) [1].
Along with solids, liquids and gases, plasma is a state of matter. It has no defined shape or volume when it is not contained. Plasma is considered the fourth state of matter and it is actually the most abundant state that elements are present in within the universe [2]. Plasma is formed by superheating a gas or by exerting a strong magnetic field to it [2]. There are various technologies that are able to create these strong fields including radiofrequency, laser or microwave generators. The action of superheating or applying a strong electromagnetic field converts atoms into ions and electrons and leads to dissociation of molecular bonds. It is for this reason that plasma is electrically conductive and responds to an electromagnetic field, allowing the creation of filaments [2], beams [2] and double layers [3]. Examples of plasma include lightening and neon signs. Plasma used in aesthetic medicine is referred to as ‘cold plasma’ with plasma generated at temperatures little above room temperature, at atmospheric pressure and with only about 1ppm of gas actually being charged into plasma.
Although any gas can be ionised to produce plasma, specific gases (noble gases such as argon and neon are commonly used) can be used for specific purposes with predictable properties. Many of the devices used in aesthetic medicine rely on the ionisation of the air between the tip of the device and the skin to generate plasma and the difference in potential between these two points produces an arc. It is this arc that delivers energy to the epidermis which results in electrical changes to cell membranes and their instant sublimation. It is this latter process that makes plasma treatments in skin procedures so appealing. Sublimation is the process of turning a solid directly into a gas without a transitional liquid phase and thereby preventing any thermal damage to surrounding tissue. A study comparing plasma (Plexr®, GMV) and radio-scalpel on the histology of induced cutaneous lesions in rabbits found that with plasma, there was “no heat damage to the dermis, no necrotic layer and the presence of an inflammatory exudate” [4]. The basement membrane remained intact in all samples.
The clinical effect of plasma devices on the skin is dependent on several factors including the mechanical and electrical resistance of the tissue and the difference in potential between the tip and the skin. This is a feature of the device and the distance between the points and there are different energy outputs depending on the device being used. Additional energy can be provided using a closed loop system where the device is grounded via an electrical pad applied to the patient. For example, the Plasma IQ (Schuco) takes advantage of this physical property and produces 1400W of energy using a closed loop system (electrical contact made with the patient and the device) on high setting and 950W when there is open loop (no electrical grounding made with the patient). Even on the low setting 1100W are generated using a closed loop compared to 650W with an open loop. If the patient has any metal implants, the use of an open system should be advocated so there is no current passing through the body.
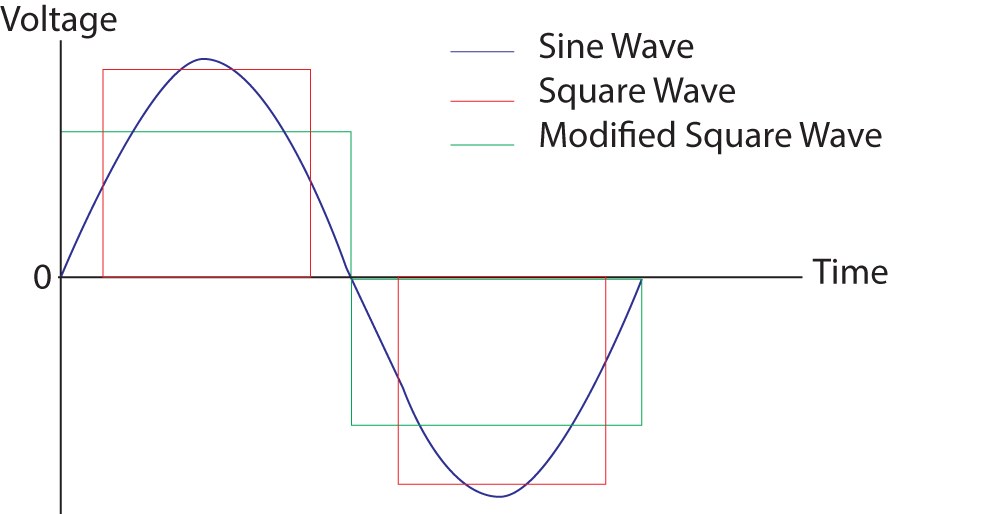
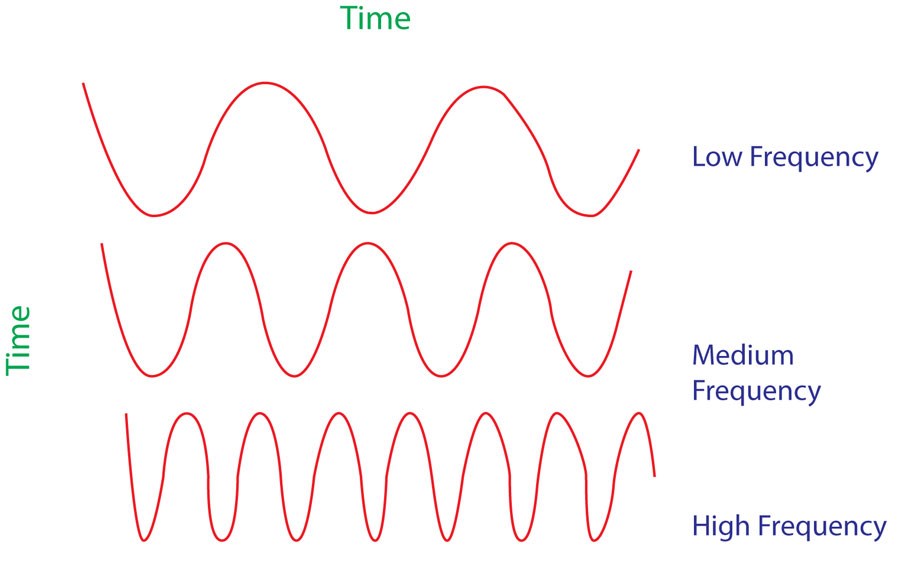
The latest generation of plasma devices used in aesthetic medicine rely on high frequency pulses as low frequencies would require a shorter tip gap and lead to unpleasant sensations including electro-muscular contractions and the sensation of electrocution. High frequencies are produced in a sine wave and often a step wave is introduced to produce a specific output where the energy produced is consistent and constant. The gap is defined as the distance between the tip and the target skin and relies on a potential difference between the two. The distance can be increased by increasing voltage or increasing frequency intensity to provide the ideal gap between the tip of the device and the patient, ensuring accurate targeting of the area or lesion to be treated.
Plasma medicine is a relatively new discipline that combines physics with medicine and already has quite a varied application, including sterilisation of implants and surgical equipment, disinfection, wound healing and treatment of skin cancers [6]. The exact mechanism of action of plasma in clinical medicine is unknown, although the process of sublimation is likely to be important as part of the epidermis is converted from solid state into a gaseous state thereby removing tissue without cutting or excision. The plasma also generates reactive oxygen species, reactive nitrogen species, free radicals and UV photons which create injury to surrounding cells. It is thought that cells which are more susceptible to damage by these chemically reactive atoms and to oxidative stress may be the reason plasma seems to be more selective in destroying bacteria and cancer cells [5]. This process of selectively targeting bacteria may help to explain why plasma treatments offer an alternative approach to the treatment of acne [6].
In aesthetic medicine, plasma can successfully treat scarring, stretch marks, acne, dyskeratosis, xanthelasma, warts, verrucae, naevi, fibromas, seborrhoeic keratosis and a host of other skin lesions [7], however the most exciting revolution for plasma technology for most patients is with non-surgical blepharoplasty.
There are a few contraindications with the use of plasma devices including pregnancy, breast feeding, use of Roaccutane®, systemic illness, infection at the treatment site, open wounds, body dysmorphia, allergy to anaesthetic agent being used, immunosuppression, auto-immune disease and keloid / hypertrophic scarring (although plasma may be used to treat scarring, it is not recommended to treat other indications in patients who are prone to the development of keloid or hypertrophic scarring). Plasma does not tend to affect the melanocytes so is safe to use in all skin types, however there may be increased healing time in darker skin types and some manufacturers recommend patch testing in Fitzpatrick skin types 4 and above. Following treatment with plasma, the skin does become more sensitive to the effects of UV radiation and it is important that patients apply a high factor, broad spectrum SPF to the area treated to prevent prolonged redness or hyperpigmentation. Of course, skin that is sublimated may take a few weeks to develop the same level of pigmentation as the surrounding skin.
Before treatment.
Day 1.
Day 2.
Day 3.
Day 4.

Day 5.
Day 6.
Non-surgical upper lid blepharoplasty
Non-surgical blepharoplasty using plasma is rapidly becoming an alternative to surgery without the need for a general anaesthetic, less downtime, less risk of damage to the underlying muscles, reduced risk of scarring, no difficulties in closing the eyes following the procedure, without the risk to vision, without risks associated with general anaesthesia (reactions, blood clots, cardiac and pulmonary complications) and more affordable to patients. However, patient selection is still important; while plasma is ideal for patients with excessive skin laxity those with a lot of hooding or pronounced subcutaneous fat in the upper lid may still choose surgery for better results. Following a full medical history and assessment with photographs, the patient is prepared using skin disinfectant and the application of a topical anaesthetic such as EMLA®, LMX4® or Pliaglis®. The author prefers Pliaglis® for this indication by the author as it contains a high percentage of local anaesthetic (70mg/g lidocaine and 70mg/g tetracaine) and is less fluid so is not likely to run into the eye itself. The topical anaesthetic can be removed after 30 minutes and then the excessive eyelid skin is treated using plasma applied at 0.5mm intervals as individual spots. Plasma treatment can be applied either by discrete spots or continuous spraying, however, when treating the delicate skin of the upper eyelids, it is important to leave healthy skin between the spots to allow contraction of the area treated and good wound healing. The patient can open and close the eyes during treatment and by applying some pressure on the skin to emphasise the skin laxity, the areas of concern can be treated more effectively. Treatment will normally take between 5-10 minutes per eye and results can be seen immediately, although the initial contraction seen may not reflect the final result and often three or more treatments are needed to produce results comparable to a surgical solution. Subsequent treatments should occur after a four to six week period. Following treatment, the application of a sun protectant and camouflage is advised and the author recommends Oxygenetix® which serves this purpose and promotes healing.
Following treatment, the patient will have brown spots at all the areas treated with plasma, this is due to carbonisation of the tissue. These resolve over five to seven days and will simply flake off, although patients are warned not to pick these off as this may lead to scarring. The following morning after treatment, there may be considerable peri-orbital swelling which resolves over the next 24-48 hours, this may be even longer if both the upper and lower lids are treated at the same time.
Possible complications from this procedure include suboptimal results, asymmetry, bruising, significant oedema, infection, erythema and pigmentation. Although plasma technology is very safe and there is data to suggest that the basement membrane is not breached so scarring does not occur, as with any medical procedure that causes destruction to the epidermis, the incorrect use of plasma may lead to scarring so education and training is paramount.
A non-surgical blepharoplasty using a plasma device (Plexr®, GMV) was conducted on 1000 patients over a two-year period (800 women and 200 men with an age range of 23-82-years -old) with 80% receiving 100% of the desired result within three treatments and 20% within one or two sessions. The recovery period was 7-15 days and no complications or adverse events were reported within the study [2] confirming that non-surgical blepharoplasty using a plasma device is a safe, effective, non-surgical option for the aesthetic practitioner.
References
1. https://en.oxforddictionaries.com/definition/plasma Last accessed February 2017.
2. Sotiris TG, Nikolaos G, Irini G. Plexr: the revolution in blepharoplasty. Pinnacle Medicine and Medical Sciences 2014;1(5):423-7.
3. Torvén S. Formation of double layers in laboratory plasmas. Astrophysics and Space Science Library 1976;74:109.
4. Gloustianou G, Sifaki M, Tsioumas SG, et al. Presentation of old and new histological results after plasma exercises (Plexr) application (regeneration of the skin tissue with collagen III). Pinnacle Medicine & Medical Sciences 2016;3(3):983-90.
5. Gay-Mimbrera J, García MC, Isla-Tejera B, et al. Clinical and biological principles of cold atmospheric plasma application in skin cancer. Advances in Therapy 2016;33(6):894–909.
6. Stamatina G, Sotiris TG, Aglaia V. Plexr in acne treatment. Pinnacle Medicine and Medical Sciences 2015;2(1):1-5.
7. Heinlin J, Morfill G, Landthaler M, et al. Plasma medicine: possible applications in dermatology. Journal of the German Society of Dermatology 2010;8(12):968-76.
COMMENTS ARE WELCOME











