Rhinoplasty refers to a procedure in plastic surgery in which the structure of the nose is changed by adding or removing bone or cartilage, grafting tissue from another part of the body, or implanting synthetic material to alter the shape (and function) of the nose. Nasal surgery can be performed to correct functional problems (e.g. improvement in airway function without changes in nasal contour) or purely for cosmesis. However, the most common scenario involves a patient seeking both functional and cosmetic nasal enhancement. After all, a misshapen nose is often associated with corresponding functional abnormalities such as a deviated septum.
Despite the fact that rhinoplasty is the most common facial, and overall the third most common, operation in aesthetic plastic surgery among both men and women, it is one of the most technically difficult surgical procedures requiring a high level of expertise and experience. To obtain aesthetically pleasing results, ensure patient satisfaction, and minimise complications, the rhinoplasty surgeon must possess a thorough knowledge of nasal anatomy and ideal facial aesthetic proportions. The surgeon must also be familiar with all types of graft material and the current techniques and methods to correct nasal deformities. This article addresses augmentation of the nose based on a unique method developed by Mr Tim Leontsinis (Consultant ENT and Facial Plastic Surgeon) using rib cartilage in conjunction with commercially available bovine pericardium (Tutopatch®).
Cosmetic rhinoplasty
Cosmetic alteration to the nose may be undertaken for a variety of different indications. The commonest practice is to carry out a reduction rhinoplasty to reshape the nose and to make it smaller. The patient usually wants the removal of a nasal hump or a more refined nasal tip. This will often make the nose look smaller because bone or cartilage has been removed. Hence the term ‘reduction rhinoplasty’ is used to describe the procedure. An example of reduction rhinoplasty and profile realignment is shown in Figure 1.


Figure 1: Reduction rhinoplasty.

Figure 2: Wegener’s granulomatosis.
Augmentation rhinoplasty, however, is performed when the individual has too little tissue to provide an attractive shape to the nose. The nose also usually lacks support and may appear ‘floppy’ with some compromise of breathing as well. The cause of this type of deformity may be congenital or due to an accident or even the result of previous nasal surgery. The latter occurs if there has been over-reduction of the dorsum or tip from a previous rhinoplasty or if too much septal cartilage has been removed with a previous septoplasty. Previous over-reduction of the bony dorsum will give the nose a so-called ‘ski slope’ appearance.
If too much cartilage from the septum has been removed due to an overzealous septoplasty, the deformity that may ensue is that of a saddle nose. In this instance the loss of cartilage causes collapse of the area immediately above the tip, which causes an over-rotated tip and a shortened nose with a ‘piggy’ look. Medical conditions such as Wegener’s granulomatosis may also result in this problem, due to septal collapse. An example of Wegener’s is shown in Figure 2. Another reason for collapse of the septum is cocaine use, which causes septal perforation.
Augmentation rhinoplasty is therefore carried out to correct the cosmetic deformities that result from either previous over-reduction of the nose or nasal collapse due to the reasons discussed above.
Materials used in nasal reconstruction
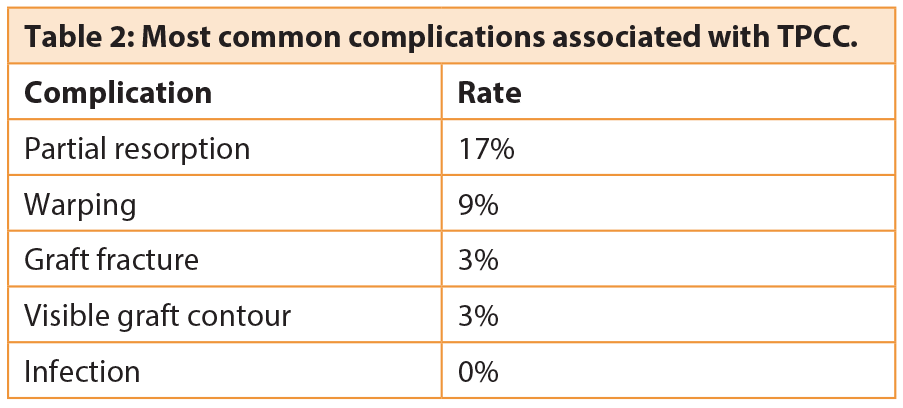
Throughout the 20th century, various alloplastic materials – as well as autologous grafts – were used for nasal reconstruction. In 1907, Jacques Joseph described the use of autologous cartilage inserted as a free graft through an endonasal incision [1]. In 1941, Peer described the ability of autologous septal and auricular cartilage to resist resorption [2]. Over the ensuing decades, a variety of grafts for augmentation of the dorsum and tip have been described. In 1979, Tardy described 2000 cases of dorsal augmentation performed by using autograft cartilage (septum, pinna and rib), with low resorption and complication rates, which subsequently became standard practice for primary augmentation rhinoplasty [3]. In recent decades, in addition to the traditional autograft dorsal augmentation, a vast array of alloplasts, xenografts and allografts for nasal augmentation has also been described (Table 1). As for tip enhancement Jack Sheen and others began using tip grafting to project the nasal tip in the early 70s [4]. First single grafts were used followed, a few years later, by multiple layered grafts of solid, scored, or morselised cartilage. Over the years tip grafting with autograft material, such as septal or auricular cartilage, has proven to be a reliable, stable method to improve tip projection and definition, and to camouflage irregularities.
The prevailing view is that permanent alloplasts (foreign material) are undesirable. The safest option is always to use natural material, preferably the patient’s own tissue. However one’s own cartilage is not always fit for purpose and may also be either insufficient in amount or difficult to harvest. Our personal view is that bone should never be used for augmentation. Ear cartilage is not always suitable, especially in the dorsum above the level of the rhinion (i.e. the point where the cartilage and bone meet on the dorsum). The skin is thin above this area, so the graft is easily seen if it is not well camouflaged. Ear cartilage may distort with time, so that an initially good result may worsen later especially in the aforementioned area of the nose.
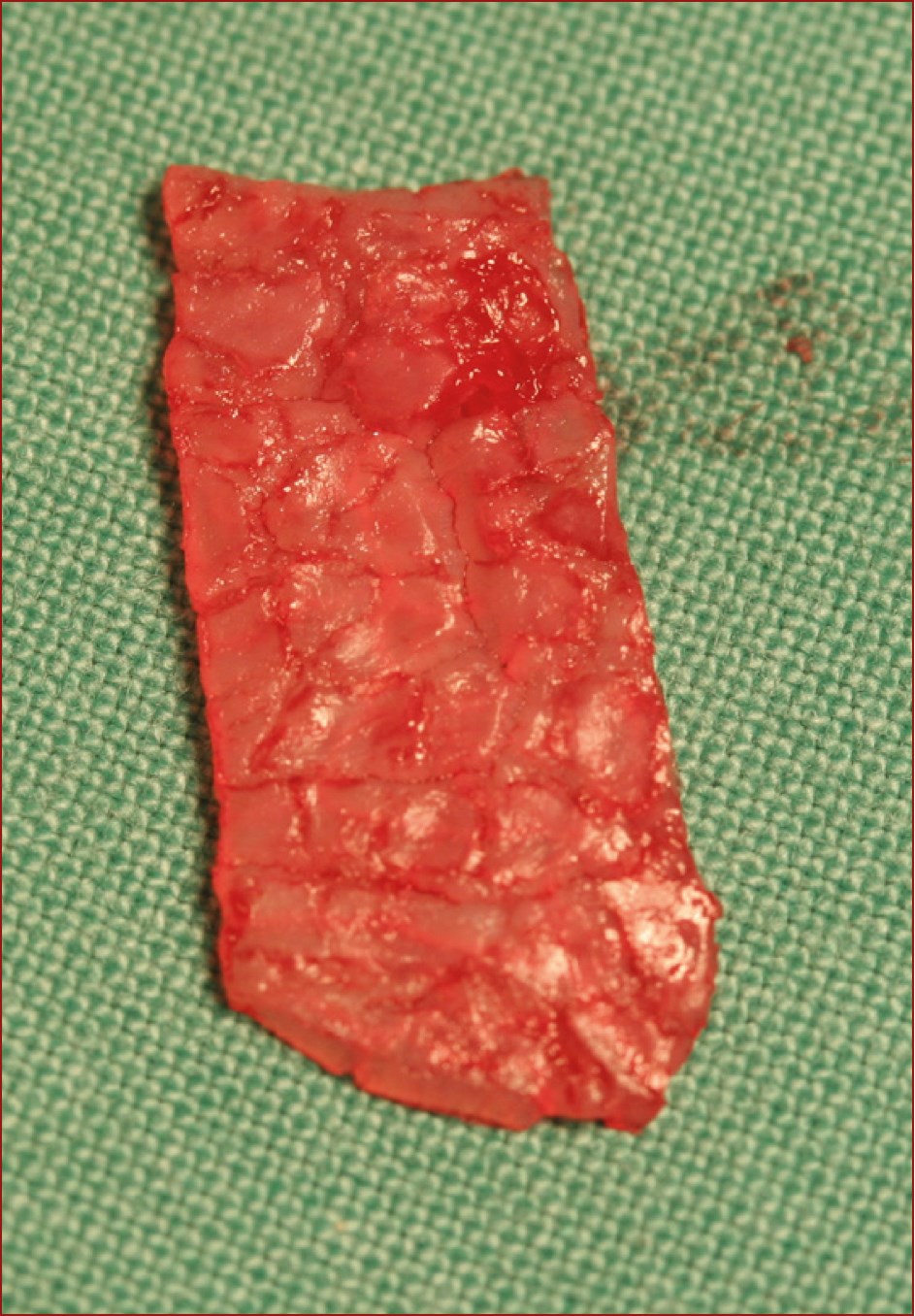
Figure 3: Crushed septal cartilage.

Figure 4a: Before augmentation with septal cartilage.

Figure 4b: Crushed cartilage placed externally.

Figure 4c: Appearance after augmentation.


Figure 5: Septal cartilage augmentation
(Top – pre augmentation and bottom – post augmentation).


Figure 6: Rib cartilage immediately after harvesting
and shown after balanced cross- sectional carving.
In primary rhinoplasty the first choice for an autograft is septal cartilage, often crushed to prevent it from being visible through the skin. Figure 3 demonstrates the appearance of septal cartilage after it has been crushed in preparation for use in nasal augmentation. Figures 4 and 5 demonstrate augmentation using septal cartilage.
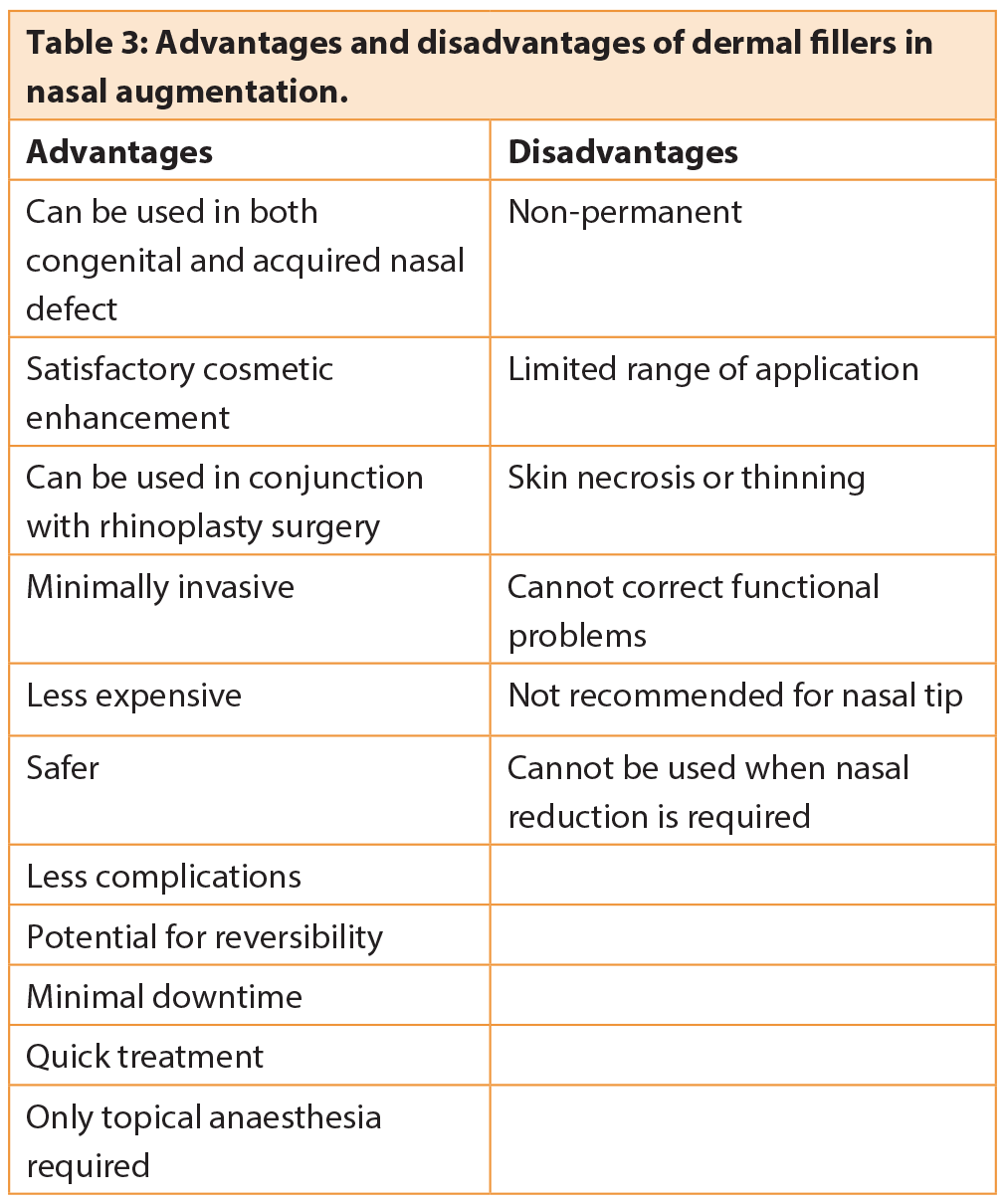
The alternative method is rib cartilage, which can be used in the dorsum or to reconstruct the septum (Figure 6). Rib cartilage is often a good choice in the dorsum but some patients may refuse to allow their own rib to be used because of perceived morbidity and scarring. In that case another option would be the use of human cadaver rib cartilage, available commercially as Tutoplast-processed costal cartilage [TPCC] which is one of the safest and strongest allograft options available [5]. Tutoplast® is a patented, scientific and technology based process of virally inactivating, preserving and sterilising human tissue for transplantation. Surgeons all over the world have used Tutoplast allografts for over 30 years. More than one million patients have received Tutoplast tissues without a single known or documented case of disease transmission [1]. In augmentation rhinoplasty, particularly in revision surgery where the availability of sufficient autologous cartilage becomes more of an issue, TPCC may be used as an alternative to autologous cartilage as it eliminates the need for cartilage harvesting and is not associated with donor site morbidity and scarring or additional operation time. In addition TPCC retains most of the general characteristics of autologous cartilage.
Nasal augmentation with the use of Tutopatch
Our preference for augmentation of the dorsum is to use rib cartilage. Although it is possible to obtain a very good result with rib cartilage that has been carved appropriately and then placed in position without fixation, Mr Leontsinis’ usual practice is now to use a different method of preparation of such grafts. The carved rib graft has the potential to be visible through the skin and also has the potential to warp. The latter may cause the nose to look deviated, although this occurs only in a minority of such grafts (Figure 7). Symmetrical carving of the harvested rib can minimise warping. Warping usually occurs early, so it might be evident even during surgery. In such instances this can be corrected immediately. If the graft warps later on, however, revision surgery might be indicated.

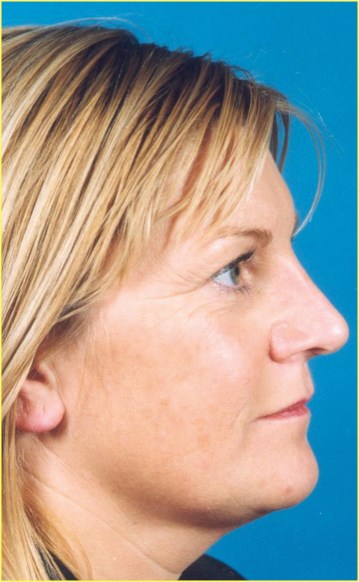
Figure 7: Conchal graft distortion and subsequent
correction using autograft rib cartilage.
Mr Leontsinis’ method is to chop up the rib, using the resulting shavings to augment the nose. The shavings can be wrapped in fascia or commercially available bovine perichondrium (Tutopatch), which helps to disguise the graft and allows it to be moulded so that it assumes a more natural and less ‘hard’ appearance. Once the desired length and thickness of the Tutopatch envelope containing rib fragments has been created the composite graft can be inserted via a closed or an open approach and placed as a single layer onto the nasal dorsum. No fixing is required other than a nasal splint which needs to be worn for at least seven days. Tutopatch is a solvent-dehydrated gamma irradiated preserved bovine pericardium surgical mesh. The Tutopatch implant consists of collagenous connective tissue with three dimensional intertwined fibre. Therefore, it has a multidirectional mechanical strength and can be fixed regardless of the direction of the graft. Collagenous connective tissue with multidirectional fibres retains the mechanical strength and elasticity of the native tissue, while providing the basic formulative structure to support replacement by new endogenous tissue resulting in a smoother and more natural result. Commercially available human cadaver rib (TPCC) offers an alternative to harvesting the patient’s own rib as discussed earlier.
Other implants
The use of silicone and other permanent graft materials in the nose is generally not advocated. These tend to be unreliable and the rate of extrusion and other complications is too high to make such grafts a viable and safe option.
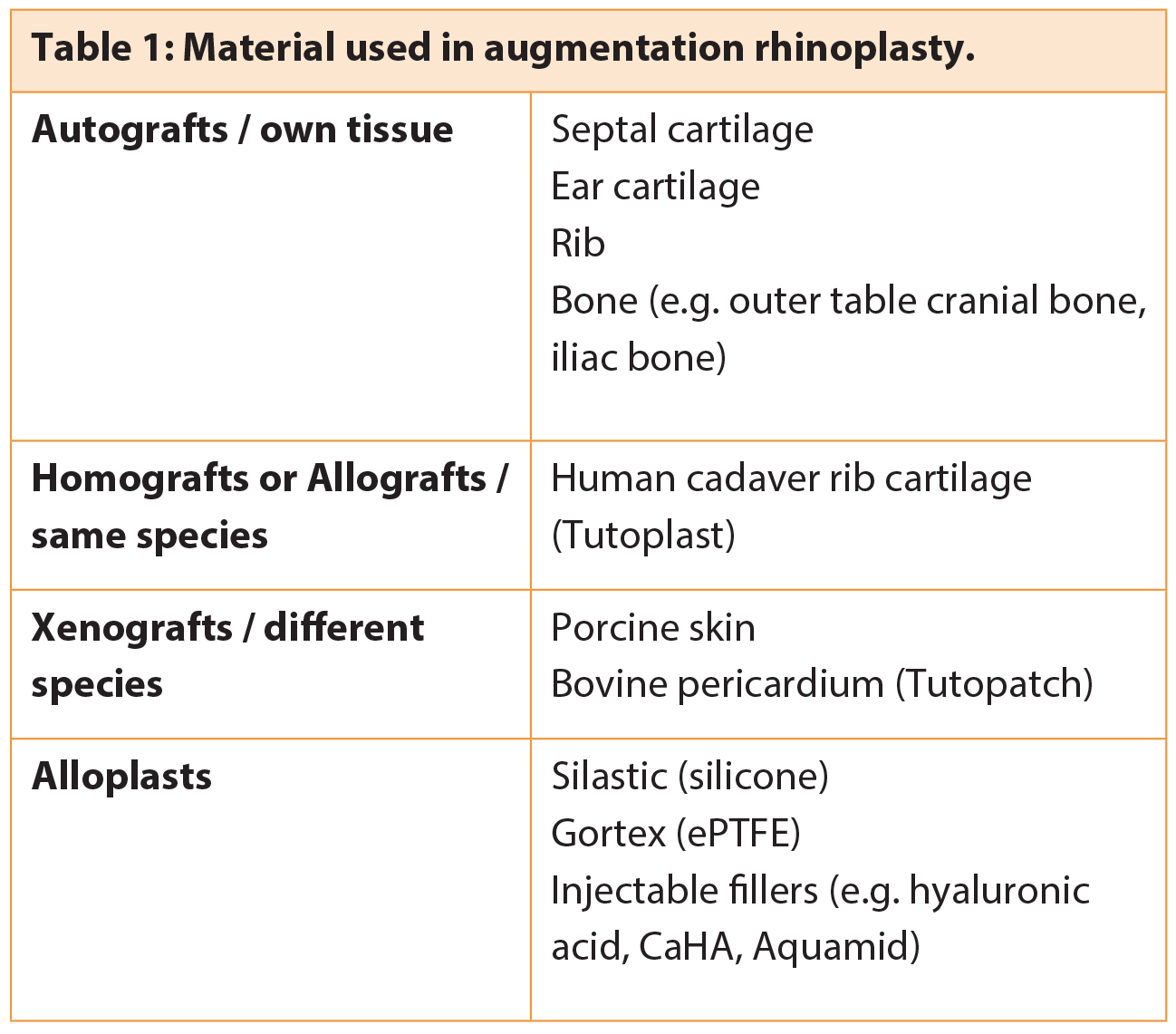
Injectable hyaluronic acid or CaHA fillers are suitable for augmentation of minor defects. They offer a good alternative to revision surgery when there is only a small area to be filled out. The patient should be made aware of the fact that repeat injections are likely to be necessary to maintain the result. Generally, fillers are not suitable in the nasal tip and their use is best confined to the dorsum, where they should be injected just above the periosteum or perichondrium.
Conclusion
The key to success in nasal augmentation is to correctly analyse the cause of the deformity and then to choose the simplest effective option to correct the defect. This may involve the use of one or more grafts as discussed above, preferably using natural tissue and sometimes with the assistance of a dermal filler for minor refinements.
References
1. Joseph J. Contributions to Rhinoplasty. Berl Klin Wahnschr 1907;46:470.
2. Chu EA. Augmentation Rhinoplasty. emedicine.medscape.com/article/881443-overview. March 2009
3. Tardy ME, Denney J, Fritsch MH. The versatile cartilage autograft in reconstruction of the nose and face. Laryngoscope 1979; 95: 523-33.
4. Sheen JH. Achieving more nasal tip projection by the use of a small autogenous vomer or septal cartilage graft. Reconstr Surg 1975;56:35-40.
5. Hyung MS. Processed costal cartilage homograft in rhinoplasty. The Asian Medical Center Experience. Arch Otolaryngol Head Neck Surg 2008; 134(5).
Acknowledgement:
With thanks to Mr Tim Leontsinis, Consultant ENT and Facial Plastic Surgeon, City Hospitals Sunderland NHS Foundation Trust.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME