With lip augmentation an ever popular option for those seeking more youthful looks it is vital that practitioners have a proper understanding of anatomy. In the first of our two-part special focus (see here for Part 2) on lips Dr Foutsizoglou provides a comprehensive guide to function and anatomy.
The lips are pliable, mobile, muscular folds that encircle the opening of the oral cavity. They contain the orbicularis oris and superior and inferior labial vessels and nerves. The lips are covered externally by skin and internally by mucous membrane. A sagittal cut through the lip can reveal the layers of soft tissue that form this relatively simple anatomical structure.
That is, from superficial to deep: skin, superficial fat compartment, orbicularis oris muscle, deep fat compartment and mucosa. The lips are used for grasping food, sucking liquids, clearing food from the oral vestibule, forming speech, osculation, and controlling the size of the oral aperture.
Functions of the lips
Food intake
Lips serve to close the mouth airtight shut, to hold food and drink inside.
Mastication
Lips help to hold food between upper and lower teeth during chewing.
Deglutition
Lips push food into the oral cavity proper during the voluntary phase of swallowing where it is ingested and prepared for digestion in the stomach and small intestine.
Articulation
The lips serve for creating different sounds – mainly labial, and labiodental consonant sounds.
Tactile organ
The lip has many nerve endings and reacts as part of the tactile senses. Lips are very sensitive to touch, warmth and cold.
Erogenous zone
Because of their high number of nerve endings, the lips are an erogenous zone. The lips therefore play a crucial role in osculation and other acts of intimacy.
Facial expressions
The lips form an integral part of facial expression e.g. smiling, frowning, etc.
Figure 1: Anatomical landmarks of the lip.
Lip anatomy
The upper lip lies between the nose and the orifice of the oral cavity. Laterally the lips are separated from the cheeks by the nasolabial grooves that extend from the nose and pass approximately 1 cm lateral to the angles of the mouth. These grooves or folds are easier to observe when smiling. The upper lip has an infranasal depression, the philtrum (Greek for love-charm), that extends from the external nasal septum, separating the nostrils, to the vermillion border – the sharp demarcation between the coloured edge of the lip and surrounding skin. The lower lip lies between the mouth and the labiomental groove, which separates the lower lip form the chin [1]. The upper and lower lips are continuous at the angles of the mouth or oral commissures (Table 1).
In adults the outer lip skin is thicker and contains hair, sweat glands, and sebaceous glands. The edges of the lips are covered with reddish skin, called the vermillion, and are abundantly provided with sensitive nerve endings. The vermillion is a transition layer between the outer, hair-bearing tissue and the inner mucous membrane. The skin of the vermillion is made up of three to five cellular layers and is very thin compared to the skin on the rest of the face, which is typically arranged in 16 cellular layers. The mucous membrane of the lip is full of capillaries that are close to the translucent surface of the vermillion, giving it its characteristic reddish colour. In newborn infants the inner surface is much thicker, with sebaceous glands and minute projections called papillae. These structural adaptations seem to aid the process of sucking [4].
The upper lip (labium superioris) is superior in name only since it is actually somewhat smaller than its partner, the lower lip (labium inferioris). In an ideal world, the lower lip vermillion show should be Phi times greater than the upper vermillion. However, that ratio can vary dramatically with ethnic background, and even from individual to individual within the same ethnic group.
The vermillion or ‘dry’ part of the lip is not hairy and does not have sweat or labial glands. Therefore, it does not have the usual protective layer of sweat and body oils which keep the skin smooth, inhibit pathogens, and regulate warmth. For these reasons, the lips dry out faster and become chapped more easily. On the other hand, the epithelium of the mucosal lip or ‘wet’ part of the lip is moistened by labial and other glands associated with the oral cavity.
The muco-cutaneous line or ‘wet-dry border’, formed where the upper and lower lips meet, marks the transition between the vermillion lip and the mucosal lip. The skin of the lips is categorised as stratified squamous epithelium, or flattened tissue cells.
The outer lip skin is keratinised stratified squamous epithelium with numerous hair follicles. As a ‘keratinised’ or waterproofed component of the skin, stratified squamous epithelium provides substantial protection against friction, microbial invasion and desiccation. As the epithelium approaches the so-called red area of the lip, the epithelium becomes non-keratinised stratified squamous epithelium. This type of epithelium is designed for protection and lubrication during chewing and swallowing.
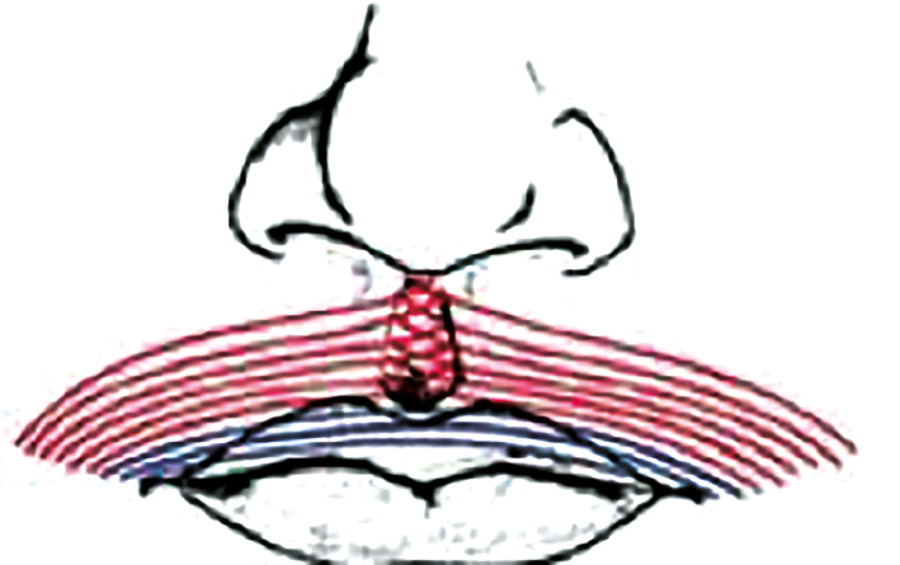
Figure 2: Anatomy of normal orbicularis oris muscle: pars marginalis (blue) and pars peripheralis (red).
Orbicularis oris
The orbicularis oris muscle, the lip muscle, is a broad elliptical muscle around the mouth (Figure 2). When the orbicularis oris is tonically contracted, the mouth is closed, whereas active (phasic) contraction causes the mouth orifice to become narrower as when kissing or whistling. Its lateral fibres join the modiolus, a chiasma of facial muscles held together by fibrous tissue, located lateral and slightly superior to each angle of the mouth.
Orbicularis oris consists of two distinct parts, the pars marginalis and pars peripheralis, which differ in location and function [5]. Anatomical studies have shown that pars peripheralis fibres decussate at midline and insert into the contralateral philtral ridge, whereas pars marginalis fibres form a continuous band from modiolus to modiolus.
Pars marginalis
It is developed to a unique extent in human lips and is closely associated with speech. In each quadrant, the pars marginalis consists of a single (occasionally) double band of narrow-diametre muscle fibres lodged within the vermillion zone of the lip. At their medial end, the marginal fibres meet and interlace with their contralateral fellows and then attach to the dermis of the vermillion zone a few millimetres beyond the median plane. At their lateral ends, the fibres converge and attach to the deepest part of the modiolar base along a horizontal strip level with the buccal angle [6].
Pars peripheralis
It is located in the cutaneous lip. It is the thinner and more peripheral portion of the muscle [7]. Pars peripheralis fibres are reinforced directly by the buccinator, levator anguli oris, and the superficial part of zygomaticus major in the upper lip, and from buccinators and depressor anguli oris in the lower lip. Its most peripheral fibres are connected with the maxillary bone and nasal septum above and with the mandible below. It has a dilatory function. The contraction of this portion of the muscle is responsible for accentuation of vertical fine perioral wrinkles or ‘smoker’s lines’.
Orbicularis oris is supplied mainly by the superior and inferior labial branches of the facial artery, the mental and infraorbital branches of the maxillary artery, and the transverse facial branch of the superior temporal artery. Its nerve supply comes from the buccal and mandibular branches of the facial nerve.
Sensory innervation
Upper lip
Superior labial nerve from the infraorbital nerve, one of the major cutaneous branches of the maxillary nerve (CNV2), the intermediate division of the trigeminal nerve.
Lower lip
Mental nerve from the inferior alveolar nerve, a major branch of the mandibular nerve (CNV3), which arises in the mandibular canal and emerges from the mental foramen normally located inferiorly to the second premolar tooth in the mandible. Those practitioners who use mental blocks for injections into the lower lip should be aware of the anatomical changes associated with loss of mandibular teeth. Following complete loss or removal of mandibular teeth, the alveoli begin to fill in with bone and the alveolar process begins to resorb. Gradually the mental foramen lies near the superior border of the body of the mandible. In extreme cases, the mental foramina disappear, exposing the mental nerves to injury. Pressure from a dental prosthesis, resting on an exposed nerve, may produce pain during eating. Loss of all the teeth also results in a decrease in the vertical facial dimension and mandibular prognathism [1].
Blood supply
Superior and inferior labial arteries arise from the facial artery. They are located 1mm posterior to the mucocutaneous border or white roll – the transition between the mucosa and skin of the lip. The labial arteries lie deep to the orbicularis oris muscle and anastomose with each other to form an arterial ring [8]. The pulse of these arteries can be palpated by grasping the upper or lower lip lightly between the first two digits.
Lymphatic drainage
Upper and lower lateral lip drain primarily into the submandibular nodes, whereas lymph from the medial part of the lower lip passes initially to the submental lymph nodes.
Lip assessment / evaluation
Lip-teeth relationships
- The maxillary incisal edge curvature should be parallel to the curvature of the lower lip in an ideal smile arc.
- At rest, there should be 2-4mm vertical exposure of the maxillary incisors in relation to the upper lip.
Tooth proportions and symmetry, gingival aesthetics, the smile arc, width of the smile, buccal corridors, incisal and gingival display, dental integrity, and occlusal relationship should be all be examined as part of the lip assessment.
Figure 3: Smile arc and teeth symmetry should be examined.

Figure 4: Lips showing soft tissue changes.
Chronological lip changes
Maxilla
- Maxillary retrusion in both dentate and edentulous individuals.
- Maxilla rotates clockwise.
- Decrease in the maxillary angle and height leading to posterior positioning of the lip and deepening of the nasolabial folds (NL).
Mandible
- Height of ramus and mandibular body length decrease with age.
- Loss of mandibular volume contributes towards laxity of platysma.
- Mandibular angle increases. This may result in blunting of jawline definition.
The dentition
- Chronological tooth wear results in flattening of the incisal edges affecting the smile arc.
- Tooth loss causes alveolar ridge resorption and cortical bone loss leading to decreased anterior lip projection (lips look thinner and inverted).
- Dentures affect the position of soft tissues and lips.
Soft tissue changes
- Epidermal thinning with flattening of the dermal-epidermal junction.
- Loss of collagen and elasting leading to reduced elasticity of skin.
- Reduction in glycosaminoglycans leading to water loss and dry skin.
- Reduction in soft tissue volume, elasticity and repeated perioral muscle activity leading to perioral rhytids.
- Perioral fat compartments become lipodystrophic and ptotic.
Structural lip changes
- Upper lip loses its volume, lengthens and inverts.
- Lower lip becomes thinner and rolls inward.
- The intercommissural width becomes smaller.
- Commissures drop.
- Decreased display of the maxillary anterior teeth.
- Exposure of mandibular anterior teeth increases.
- Philtrum columns flatten and ‘splay’ as they approach the upper vermillion border.
- Vermillion border becomes thinner.
- Partial loss of Cupid’s bow.
- Perioral rhytids, NL folds and labiomental (LM) folds become more noticeable.
- Curves of the lips are lost.
- Lips become more dry.
References
1. Moore KL, Dalley AF. Clinically Oriented Anatomy. 4th Edition. Lippincott Williams & Wilkins; 1999.
2. Hennekam RC, Cormier-Daire V, Hall J, et al. Elements of morphology: standard terminology for the nose and philtrum. Am J Med Genet A 2009;149A:61-76.
3. Carey JC, Cohen MM Jr, Curry C, et al. Elements of morphology: standard terminology for the lips, mouth, and oral region. Am J Med Genet A 2009;149A:77-92.
4. www.britannica.com
5. Azib N, et al. Anatomy and Lip Enhancement. Paris, France; E2e Medical Publishing / Master Collection 4; 2011.
6. Standring S. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 41st Edition. Elsevier; 2016.
7. Trevidic P, Sykes J, Criollo-Lamilla G. Anatomy of the lower face and botulinum toxin injections. Plastic Reconstruct Surg 2015;136:55.
8. Brown DL, Borschel GH. Michigan Manual of Plastic Surgery. Lippincott Williams & Wilkins; 2004.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME