In cases of long-established facial palsy, one of the main problems faced by patients is the inability to smile. In this situation, consideration should be given to facial reanimation (smile) surgery. In most cases of chronic facial palsy new muscles will need to be imported into the face. The two main methods are either a regional muscle transfer or a free muscle transplant. With regard to regional muscle transfers, my preference is to use the temporalis muscle. This muscle has an ideal vector to restore a commissure (‘Mona Lisa’) smile, which is the commonest type of smile.
The temporalis transfer for smile restoration is not a new technique. It has been used either as a turnover flap or as an orthodromic transfer. Daniel Labbé (2000) developed an elegant refinement of the orthodromic temporalis transfer, which he called a lengthening temporalis myoplasty. This technique is based on the intrinsic ability of the temporalis muscle to stretch, such that its tendon can be made to reach the mouth without requiring the interposition of fascia. A major advantage of this procedure is that patients can learn to use the temporalis as a smile muscle, rather than a chewing muscle. In 2009 Labbé reported a modification (version two) of his original technique in which the extent of muscle dissection was reduced, lessening the duration of the operation. The procedure we perform in Newcastle is essentially version two of the lengthening temporalis myoplasty, with a few modifications.
Patient selection
Indications
- Facial palsy of at least a year’s duration.
- All age groups. In our unit, it has largely supplanted static techniques for facial reanimation in the elderly and in patients who are not suitable for free-tissue transfer.
Contraindications
- Denervated or damaged temporalis muscle.
- Severe facial tightness or synkineses.
Preoperative assessment
- The nasolabial fold is marked on the paralysed side.
- The patient is asked to smile in order to assess the smile type (Rubin 1974) on the normal side of the face.
- While smiling, the area medial to the non-paralysed nasolabial fold is closely examined for the insertions of the zygomaticus and levator muscles.
- The corresponding muscle insertions are marked as accurately as possible on the paralysed side.
Figure 1: Question mark shaped incision.
Operative procedure
- Nasotracheal intubation is preferred, so that the symmetry of the mouth can be assessed at the end of the procedure.
- Hydrodissection is performed by infiltrating 40-50ml of a solution of 100ml normal saline, 20ml 0.5% Chirocaine, and 0.2ml of 1:1000 adrenaline, into the plane between the superficial and deep temporal fascia. 10-15ml is also infiltrated into the nasolabial fold and the cheek.
- A ‘question mark’ shaped incision is made in the temporal scalp on the paralysed side (Figure 1).
- The scalp flap is quickly elevated through the loose areolar tissue between the superficial and deep temporal fascia.
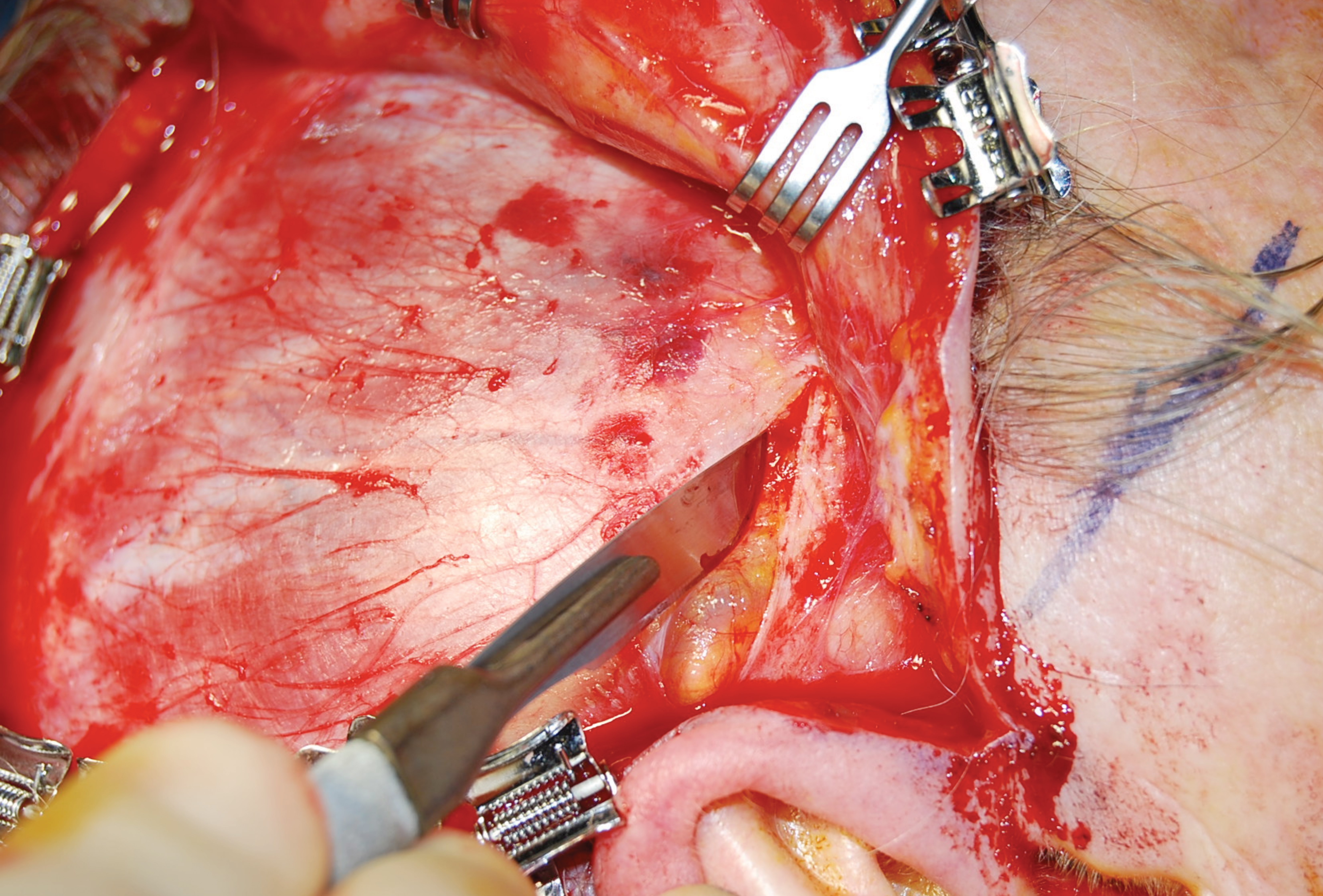
- Cologne scalp clips are applied for scalp edge haemostasis (Figure 2).
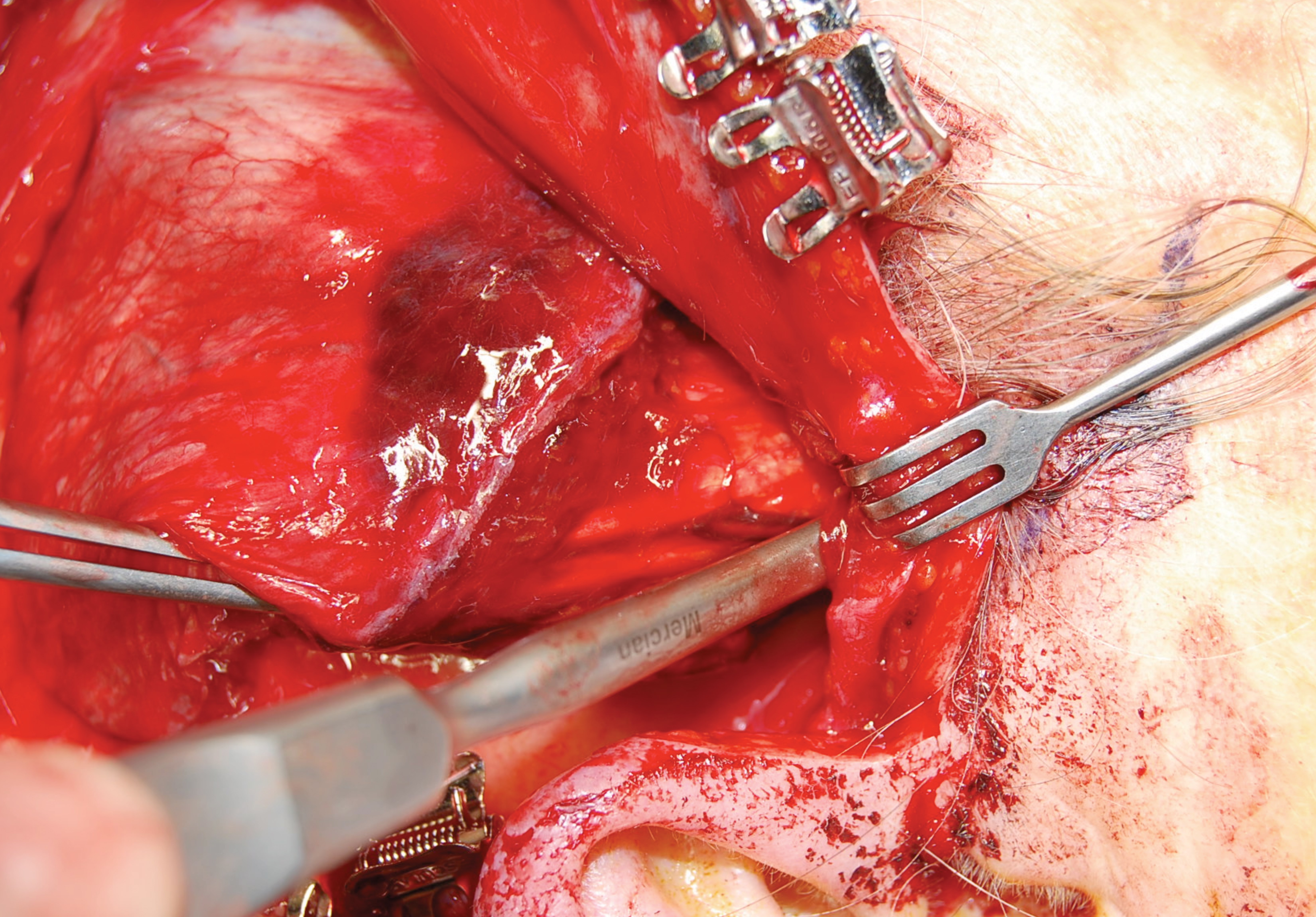
- About 1.5cm cranial to the zygomatic arch, both layers of the deep temporal fascia are incised down to the temporalis muscle (Figure 3). This allows a periosteal elevator to be passed under the zygomatic arch into the cheek (Figure 4), and is the same plane as the Gillies temporal approach to zygomatic arch fractures.
- The temporalis and deep temporal fascia are incised just below the inferior temporal line, leaving a cuff of fascia attached to the superior temporal line. This incision is carried straight through the pericranium to the bone and continues in this fashion parallel to the original scalp incision.
- The anterior quarter of the cranial part of the muscle is not incised, but instead remains attached to the anterior part of the temporal scalp flap and to the deep temporal fascia above. In theory, this maintains a blood supply to the muscle in cases where the maxillary artery has been ligated or damaged.
- The temporalis muscle is elevated subperiosteally off the temporal fossa with an Obwegeser periosteal elevator (Figure 5), preserving the delicate vessels and nerves on its deep surface. This continues until the whole muscle is elevated off the temporal fossa, including elevation of the anterior fibres from the lateral orbital wall.
- Any remaining attachments to the root of the zygoma and the infratemporal crest are meticulously divided.
- A nasolabial incision is made on the paralysed side. This incision is undermined for a few millimetres medially. Laterally, subdermal dissection is performed for up to 2cm.
- Metzenbaum scissors are used to develop a pocket between the buccal fat pad and the masseter muscle. This pocket is further developed by blunt finger dissection.
- Coronoidectomy is performed with a reciprocating saw, with the direction of the saw towards the sigmoid notch of the mandible.
- Unwanted muscle fibres are cleared away from the temporalis tendon and any residual attachments to the mandible are divided. Downward traction on the coronoid process facilitates this process.
- Dissection is continued until the tendon easily reaches the nasolabial incision.
- The coronoid process is separated from the tendon subperiosteally.
- The tendon is sutured with 4/0 clear Prolene to the predetermined points just medial to the nasolabial fold.
- The posterior fibres of the temporalis muscle are reattached to the cuff of deep temporal fascia in a more anterior position, with 2/0 polydioxanone suture (PDS).
- The scalp is closed with staples after insertion of a fine bore suction drain.
- The nasolabial incision is closed with dermal Vicryl and subcuticular 5/0 Prolene.
Figure 2: Cologne clips on scalp edge.
Figure 3: Incision through deep temporal fascia.
Figure 4: Periosteal elevator passed under zygomatic arch.
Figure 5: Subperiosteal elevation of temporalis muscle.
Figure 6: Patient before surgery - at rest.

Figure 6: Patient before surgery - smiling.

Figure 7: Patient after surgery - at rest.
Figure 7: Patient after surgery - smiling.
Postoperative care
- The patient is kept on a soft diet for five to seven days.
- Discharge usually on the second postoperative day.
- Facial physiotherapy starts at three weeks.
Advantages
- Single stage procedure.
- Short operative time, around 120-130 minutes.
- Short inpatient stay.
- Predictable outcomes.
References
1. Langevin HM, Bouffard NA, Badger GJ, et al. Subcutaneous tissue fibroblast cytoskeletal remodelling induced by acupuncture: evidence for a mechanotransduction-based mechanism. J Cell Physiol 2006;207:767-74.
2. Gabbiani G, Hirschel BJ, Ryan GB, et al. Granulation Tissue as a Contractile Organ. A study of structure and function. J Exp Med 1972; 135(4):719-34.
COMMENTS ARE WELCOME
Declaration of competing interests: None declared.