This article has been verified for CPD. Click the button below to answer a few
short questions and download a form to be included in your CPD folder.
The authors describe their technique and experience of treating rhinophymas with a CO2 laser at the Welsh Centre for Burns and Plastic Surgery in the UK.
Rhinophyma, a severe form of chronic rosacea, is a benign proliferative disorder of the nose almost exclusively affecting Caucasian men [1]. Although its pathogenesis is still not completely understood, clinical manifestations include erythema and enlargement of the nose with tumour-like growths due to sebaceous and connective tissue hypertrophy [1].
The subsequent deformity can not only result in nasal obstruction but also has psychosocial implications due to its unsightly appearance and perceived association with alcohol abuse, resulting in negative effects on quality of life [2,3]. Numerous different treatment methods have been outlined including dermabrasion and surgical excision, however, more recently the use of a CO2 laser has been described [1,4,5].
This ablative laser works by targeting intracellular water resulting in cell vaporisation and subsequent tissue destruction. In this article we describe our technique and experience of treating rhinophymas with a CO2 laser at the Welsh Centre for Burns and Plastic Surgery, Swansea, United Kingdom.
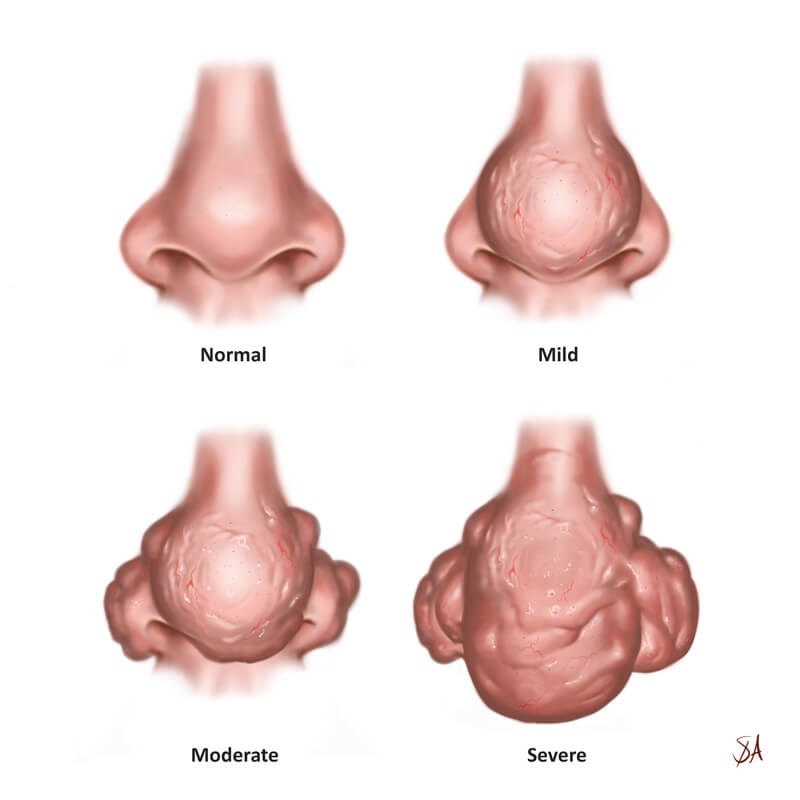
Figure 1: Schematic representation of the clinical severity of rhinophyma according to
The Welsh Centre for Plastic Surgery criteria for severity assessment and laser treatment of rhinophyma.
Technique
We perform the procedure under local anaesthetic in an outpatient setting. The nose is prepared with an antiseptic solution and the anaesthesia administered. All necessary safety precautions are undertaken, including eye protection for both staff and the patient prior to commencement of the treatment. The UltraPulse® CO2 laser, aided by use of the plume evacuator, is then used to ablate the main bulk of the rhinophyma. This is achieved by selecting a 2mm ‘TrueSpot’ hand piece on continuous wave settings. This may start at 12 watts, or be increased as high as 30 watts, depending on the size of the area to be reduced. A ‘layer-by-layer’ technique is used. The high settings ensure vaporisation of the tissue and usually there is no requirement to wipe away the eschar. Early signs of adequate ablation include visible expression of the contents of the dilated glands, coined the ‘gopher sign’ by the senior author [6].
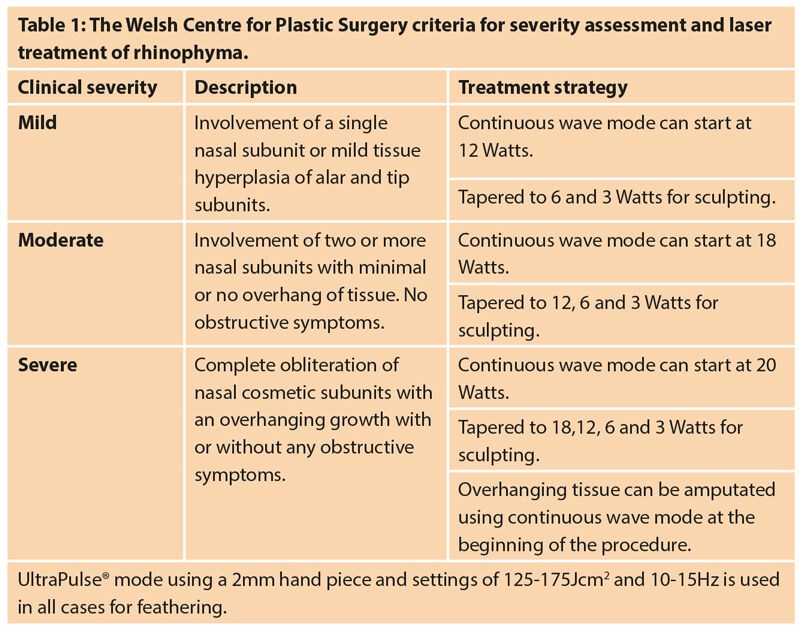
As the bulk is reduced it is important to progressively lower the energy to maintain control and minimise the potential of over-reduction and scarring. This usually follows a pattern of 8 watts, 6 watts and 3 Watts until a satisfactory end point is achieved (Table 1). Finally, the CO2 laser is changed to the UltraPulse® mode. Using a 2mm hand piece and settings of 125-175 Jcm2 and 10-15 Hz, finer shaping, ‘feathering in’ and blending of treated areas into normal surrounding tissue is achieved. The patient is given a mirror prior to concluding the treatment to ensure the outcome of the ablation is satisfactory.
An antibacterial ointment is applied to the area following treatment, which remains covered with a brown eschar that gradually separates over a period of three weeks. Written instructions for aftercare are also given and discussed with the patient.

Figure 2: An 89-year-old gentleman who was referred to our service with moderate rhinophyma.
The patient had involvement of at least three nasal subunits with no overhang of tissue.
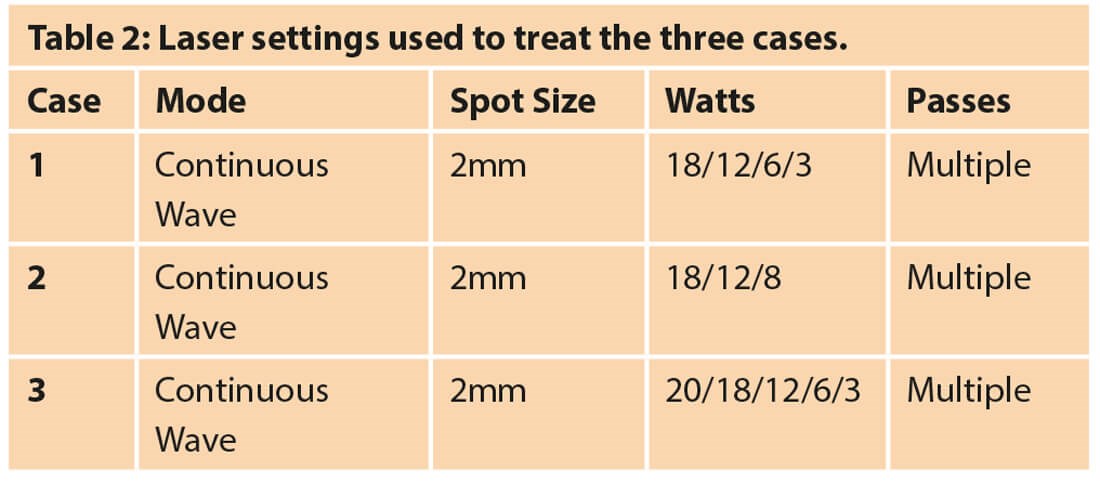

Figure 3: Three months post a single treatment session with the CO2 laser.
Case 1
Figure 2 illustrates the appearance of an 89-year-old gentleman who presented with a rhinophyma. The patient had a history of nasal obstruction and was unhappy with his appearance. He had undergone no previous treatments for his rhinophyma, which was classified as moderate as per our protocol, with significant proliferation of tissue over both nasal alae. The patient underwent a single CO2 laser treatment using continuous wave and UltraPulse® modes. The laser power was progressively reduced to precisely sculpt the aesthetic units of the nose (Table 2). The patient achieved excellent improvements in the shape, texture and size of the nose and was very happy with the outcome of his treatment (Figure 3).

Figure 4: A 60-year-old gentleman who was referred to our service with severe rhinophyma.
The patient had previously trialled various topical agents without success.
The patient had obliteration of nasal aesthetic subunits with a tissue overhang.
Case 2
A 60-year-old gentleman with a known history of rosacea presented with a progressively enlarging rhinophyma (Figure 4). He was self-conscious regarding his appearance and had undergone numerous medical treatments for his rhinophyma in the past. Clinically, the patient had a bulbous and nodular overhanging rhinophyma primarily affecting the tip of the nose causing obstruction of his right nostril. There was also moderate involvement of both alae and therefore the rhinophyma was classified as severe. The patient was treated with a continuous wave mode of CO2 laser using the settings shown in Table 2. The overhanging rhinophyma was amputated using the laser before sculpting the nasal aesthetic subunits.

Figure 5: Immediate post-treatment appearance illustrating complete
haemostatic control with no requirement for wound dressings.

Figure 6: Appearance three months post a single treatment session with the CO2 laser.
Figure 5 represents the immediate post-treatment appearance of the nose demonstrating haemostatic control of the treated area. At three months the treated area had healed completely with no scarring or residual oedema (Figure 6). There was, however, some hyperpigmentation noted although it did not affect the patient and no further treatment was undertaken.

Figure 7: An 81-year-old gentleman who was referred to our service with severe rhinophyma.
The large polypoid growth extending from the nasal tip was making it extremely difficult for him to drink.
Case 3
An 81-year-old gentleman with a one-year history of severe rhinophyma presented to our outpatient clinic (Figure 7). The patient always found his rhinophyma to be unsightly, however, he was now finding it increasingly difficult to drink, which subsequently prompted his referral to our unit. He had a large polypoid growth affecting the nasal tip, which extended to the dorsum of the nose superiorly and the nasal alae bilaterally. The weight of the growth was also causing mechanical collapse of the nostrils.

Figure 8: Appearance three months post a single treatment session with the CO2 laser.
The patient was treated with a continuous wave mode of CO2 laser and the overhanging rhinophyma was amputated before sculpting the nasal aesthetic subunits (Table 2). At three months the wounds were completely healed, and a good nasal contour and shape was achieved with no scarring (Figure 8).
Discussion
Rhinophyma is a progressive proliferative disorder with an incompletely understood aetiology that can lead to significant deformity of the nose. Despite the common belief that it is associated with alcohol excess, none of our cohort demonstrated a history of this. This finding is supported by existing literature outlining that little evidence exists confirming this association [7,8]. Various different modalities exist for its management, including topical medications, however, it is widely accepted that for severe cases surgical intervention is required [4,9]. Techniques including electrosurgery, cryosurgery and scalpel excision have all been described, although more recently the use of CO2 ablative lasers have been utilised. Both fractionated and non-fractionated lasers can be used, with fractionated devices delivering the laser energy as interspacing columns creating areas of tissue that remain unaffected [4]. For this reason the amount of debulking may be less, resulting in more modest outcomes if used alone. Serowka et al. [4] advocated its use in early to moderate cases of rhinophyma due to previous concerns regarding the side-effect profile of non-fractionated ablative lasers, including prolonged oedema, permanent pigmentary changes and scarring [10,11].
In our experience, the CO2 laser’s continuous wave mode for tissue ablation followed by UltraPulse® mode for feathering and finer sculpting produces excellent results. In the first few cases treated by our laser service, alar notching was observed following treatment due to overtreatment of the areas. This was corrected by adjusting the continuous wave mode settings and following a careful ‘layer-by-layer’ approach. In some cases pigmentary changes were also noted. Hyperpigmentation was usually self-limiting and settled by three months. Such changes were further reduced by advocating the use of sunscreen in the post-treatment period. Hypopigmentation was also observed and was more obvious within a background of persistent rosacea. If needed, this redness could be addressed with a vascular laser, however, none of our patients requested further treatment. We found that the majority of complications encountered are minor and widely acceptable to patients, with the cohort reported in this study being universally pleased with the outcome following treatment. This is, albeit, user dependent and experience is paramount, along with a sound knowledge of the nasal aesthetic subunits.
The main advantages that we find to using a CO2 laser is the immediate haemostasis and precision that can be obtained with regards to the depth and area of tissue destruction when compared to other surgical treatment methods. Van Gemert et al. demonstrated this through histological analysis and found vaporisation of tissue with a CO2 laser occurs within a 0.5mm error in the desired treatment area [12]. Because the treated area formed a dry eschar requiring only antibacterial or paraffin-based ointment, no wound dressings were necessary and minimal hospital visits for wound care were required, resulting in reduced healthcare costs
Conclusion
In our experience, the CO2 laser is an extremely effective modality for the treatment of rhinophyma of all severities. Its marked haemostatic effects and precision allow for controlled and safe ablation of the intended tissue.
References
1. Amaral MTSS, Haddad A, Nahas FX, et al. Impact of fractional ablative carbon dioxide laser on the treatment of rhinophyma. Aesthet Surg J 2019;39(4):68-75.
2. Lazzeri D, Larcher L, Huemer GM, et al. Surgical correction of rhinophyma: comparison of two methods in a 15-year-long experience. J Craniomaxillofac Surg 2013;41(5):429-36.
3. Sadick H, Goepel B, Bersch C, et al. Rhinophyma: Diagnosis and treatment options for a disfiguring tumor of the nose. Ann Plast Surg 2008;61(1):114-20.
4. Serowka KL, Saedi N, Dover JS, et al. Fractionated ablative carbon dioxide laser for the treatment of rhinophyma. Lasers Surg Med 2014;46(1):8-12.
5. Madan V, Ferguson JE, August PJ. Carbon dioxide laser treatment of rhinophyma: a review of 124 patients. Br J Dermatol 2009;161(4):814-8.
6. Javed M, Murison M. The ‘Gopher Sign’: A clinical sign to determine the adequate depth of CO2 laser ablation in rhinophyma. World J Plast Surg 2019;8(1):120-1.
7. Curnier A, Choudhary S. Rhinophyma: dispelling the myths. Plast Reconstr Surg 2004;114(2):351-4.
8. Wiemer DR. Rhinophyma. Clin Plast Surg 1987;14(2):357-65.
9. Fink C, Lackey J, Grande DJ. Rhinophyma: A treatment review. Dermatol Surg 2018;44(2):275-82.
10. Nanni CA, Alster TS. Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Dermatol Surg 1998;24(3):315-20.
11. Helm TN, Shatkin S Jr. Alabaster skin after CO2 laser resurfacing: Evidence for suppressed melanogenesis rather than just melanocyte destruction. Cutis 2006;77(1):15-7.
12. Van Gemert M, Welch AJ, Tan OT. Limitations of carbon dioxide lasers for treatment of port-wine stains. Arch Dermatol 1987;123(1):71-3.

COMMENTS ARE WELCOME