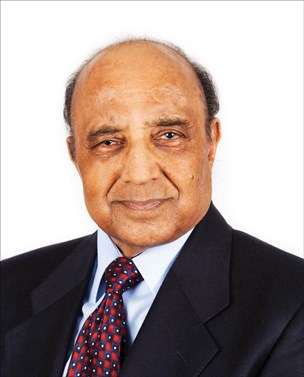
British Medical Laser Association (BMLA) held its 39th annual conference, the first in-person gathering following the COVID-19 pandemic, in the academic surrounding of the Surgeons’ Quarters of the Royal College of Surgeons in Edinburgh. Chris Henson caught up with 87-year-old Vasant Oswal, the Vice President of the BMLA, to reflect upon his ENT career spanning over the past 62 years. Widely known for his pioneering work in developing laser surgery for ENT way back in 1982, the interview with Chris focuses on those early days when even the word laser was not in everyday vocabulary.
What would you say was your motivating factor in innovating the use of lasers in ENT?
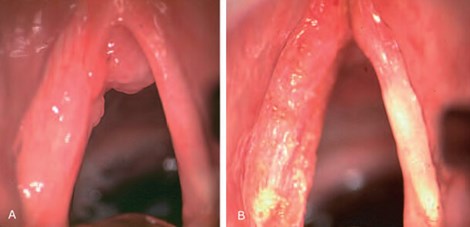
In ENT, and specifically in laryngology, it is essential that while removing the entire diseased tissue, we do not damage the integrity of the vocal fold; otherwise, the patients would end with a worse voice production due to loss of normal tissue and scar formation. Traditionally, tissues are cut with cold steel instruments, which also cut the blood vessels, needing constant mopping or sucking. Electric diathermy or cautery did seal the blood vessels, but their energy could not be controlled precisely for delicate surgery on the vocal folds. Laser offered a technology that vaporised the tissue and simultaneously sealed off minute blood vessels, allowing an unobstructed view of the excision line.

Conventional instruments have a long shaft which carries the cutting end, such as a knife or a pair of scissors, obstructing a full view of the operating site. The laser beam does not need a carrying handle and thus allows an unobstructed view of the surgical site – the beam was dubbed the ‘handle-less knife’. And then there are even more advantages; the hot beam seals lymphatics which prevents the microscopic spread of cancer, within the organ or even outside, into the lymph nodes. And as a bonus, the beam plugs the nerve endings with shrivelled tissue, significantly reducing postoperative pain. So, apart from a very significant initial outlay, there were many plus points to using the laser technology for surgery.
What were your initial steps with the technology? How did it begin to influence practice?
An interesting question: what my initial steps were. The most crucial step was to find £40,000 to get the laser for our department, a vast sum of money in 1982. My hospital certainly did not have that kind of money, and that too, for technology so new that even the word laser was not in everyday vocabulary. Some people I knew helped me establish a public appeal to raise funds. To my astonishment, they collected all £40,000. The appeal was so successful that it went on £72,000 in six months when we closed it.
The laser was installed by a company called Coherent (UK). Then came the tricky part. What do I do with the laser? I had used it on an apple at the conference in Budapest in 1981, where it was in the trade exhibition. There were very few articles in the journal, mainly on the laser surgical outcome rather than the fundamentals of the laser as a source of energy for surgery. There were also no courses that I could go to. So, I decided to do bench experiments to teach myself.
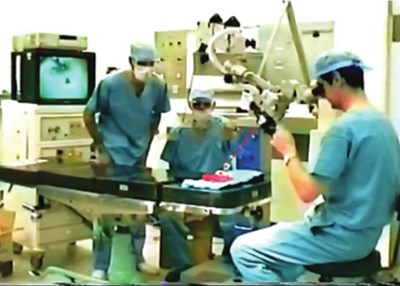
Fortunately, video cameras were just being introduced in the market, and we got one to mount on the operating microscope to record the experiments. The technicians in the theatre, Paul, Dennis and Gordon, stayed back in the evenings to help me. I spent evenings and weekends in the theatre for the next six weeks. We decided to use steak from the butchers to mimic tongue muscles. That evening, I took the recording home and studied the laser effects by advancing each frame. There are twenty-five frames in one second in the VHS format. Thus, I could clearly see the energy spread within the steak at the various power and exposure settings.
It was a great time. Now, I had a calibration chart to set the power and exposure time to control its deep spread, which was necessary not to damage the vocal folds during the surgery on the larynx. Later on, I used egg white to strike the laser beam. Being transparent, the spread of the energy causing coagulation was clearly seen, a very visual teaching method!
How did you navigate the use of lasers in delicate procedures, such as surgery involving the larynx?
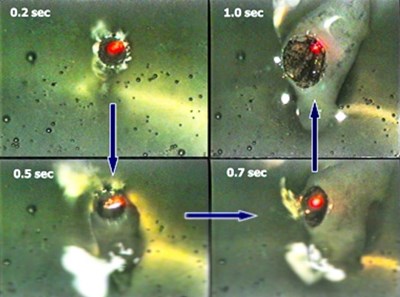
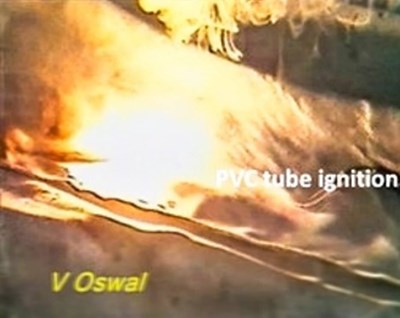
We did many more experiments to determine laser beam effects with strikes on instruments, swabs, plastic and rubber anaesthetic tubes – present in the operating field. Again, I studied the spread of the laser effect frame by frame. The most dramatic effect was on the plastic and the rubber anaesthetic tubes; in the presence of 50 per cent oxygen, the plastic tube burnt with an explosive fire within half a second of the strike. The rubber tube also caught fire but a bit slowly.
One day while having a shower, I thought, why not make a metal tube for anaesthesia which will not catch fire? Our physics department and John Hunton, our anaesthetist, helped us design a tube. We struck it with the laser beam, and as expected, there was no fire. We found an instrument maker from Lancaster; he came to the theatre with his technician and designed a set of tubes, including a baby tube for a nine-month-old with a papilloma on the vocal fold.
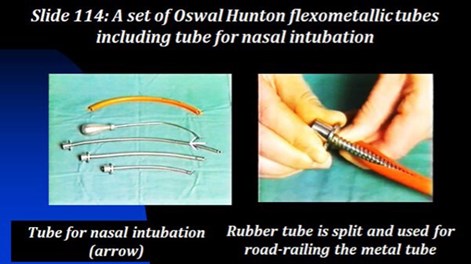
There was an article on using metal tubes from the States, but they were not marketed. Our instrument maker marketed them as Oswal-Hunton flexo-metallic fire-proof anaesthetic tubes. Hand in hand, we continued to develop laryngeal surgery using several anaesthetic techniques such as tubeless anaesthesia, jet ventilation, apnoeic technique, etc. Then there were other ways, a bivalve laryngoscope, pressing on the thyroid cartilage to improve the exposure and so on.
Were you able to keep adapting the tube to make it more valuable over time?
I saw a nine-month-old baby with a hoarse cry; he had papilloma on the vocal fold. The manufacturers made a tube 4mm in diameter. We put it in the child. We took an X-ray on the operating table, which showed the far end butting against the posterior wall of the trachea. The technician who had brought with him several similar tubes bent the end by 15 degrees. We sterilised with alcohol and inserted it; the angulation was now perfect. The ‘baby tube’ was included in the set.

The CO2 laser was a pioneering achievement back in 1982. Does it continue to be the laser of choice for ENT?
That's an interesting question. In the medical field, many a time, a promising new technology does not last long because some unwanted side effects come to light or a better technology takes over. But the CO2 laser technology, with its advantages and very few disadvantages, secured its place as a standard tool in many specialities worldwide. This multi-speciality use meant that a substantial initial outlay is justified. And many patients recovered so well that they did not have to stay in the hospital for many days. The turnover of the inpatients thus increased.
But in our speciality, the most telling benefit was in the larynx. Before the lasers, we used six weeks of radiotherapy for early cancers. It had unpleasant side effects. All early cancers are removed precisely with a laser beam carried via a laryngoscope. The surgery is called transoral laryngeal laser surgery, and it is now a standard procedure for almost all types of conditions affecting the vocal folds.
Other lasers, the diode and the KTP, are also used since, unlike the CO2 laser, they can be delivered via a fibreoptic cable. Even as an office-based surgery on the larynx. But CO2 remains and, as far as I can tell, will continue to stay the wavelength of choice for ENT. It is, therefore, rightly called 'a workhorse laser for the ENT.' You can almost say that the transoral surgical approach, which was not possible before the lasers, is now used routinely with these lasers.
These advances in laryngeal surgery led to the establishment of a new subspeciality of laryngology. Many associations have been founded solely for laryngology. I founded the Asia Pacific Laryngology Association with many like-minded colleagues from the Asia Pacific region in 2017. we held the first conference in Singapore in 2019, attended by 350 participants. The second conference was planned in Manila but was called off due to the COVID-19 pandemic.
How did you continue to develop the technology to extend its use?
We ordered an adapter for using the laser in the bronchus. In some lung cancer patients, the spread into the bronchus obstructs their breathing. As cancer grows, they get desperate to breathe. The laser beam delivered with the adopter was able to burn cancer and open up the airway. These are complicated cases; the anaesthetist also has to use the obstructed airway simultaneously. Focusing the beam on the tumour was tricky; the char caused by the laser beam flared, and the smoke blocked the view. But gradually, we became more confident, and such cases became a routine. Several patients came from other centres, including Newcastle. Their surgeons also came to our theatre to watch and learn the new surgical techniques. The surgery to restore the airway for the obstructed patient was the most rewarding experience.
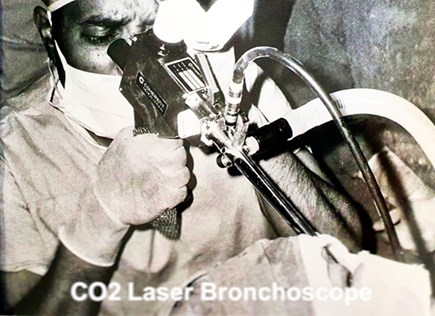
I undertook many such surgical procedures after this initial experience and became quite adept at using the laser. I chaired the first British conference in Middlesbrough in 1983 and started the laser course, which ran for 28 years! I also edited and wrote three laser books and received invitations from many countries to run their courses and chair conferences.
Lasers are a good indicator of the importance of technological advancements in laryngeal surgery – what are other key developments in head and neck surgery?
Robotic laser surgery is an advancement, but still, there are technical problems in dealing with cancers at the glottic level and below. Rehabilitation, providing the patient with as normal a life as possible, is also what we should be aiming at. Way back in 1974, I developed a ‘team concept’. As the surgeon removes the disease via laryngectomy, the patient can no longer continue everyday life. They lose their voice, swallowing becomes difficult, and there are other difficulties. I thought of it differently; the person who removes the larynx is also responsible for rehabilitating the patient. The ‘team’ would include a speech therapist to train the patient, a physiotherapist to see the patient before surgery, and we would also speak to the patient’s manager at work and inform them that the patient will not be able to work in a dusty environment.
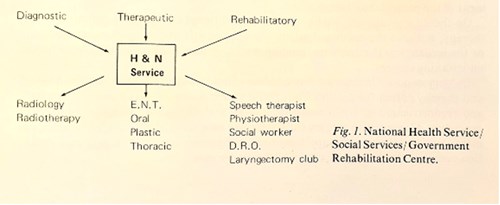

This approach was presented in Toronto in 1974 when they held a Centennial Conference on Laryngeal Cancer to mark the first laryngectomy performed 100 years previously, in 1874. Seven hundred surgeons attended and heard our presentation on the ‘Team Concept of Management of Cancer of Larynx’ (now known as a multidisciplinary team, or MDT). I am proud that my presentation was judged as the best entry at the conference and awarded a scroll.
Finally, Mr Oswal, a quick word on BMLA – how have you found the annual conference here in Edinburgh this year?
BMLA was established in 1982; I am a founder member. We have a membership of a couple of hundred members, and we hold annual conferences. The BMLA remains one of the most well-respected organisations about lasers and high-energy devices in the UK. Now, in 2022, our conference has a special significance, being the first since the start of the COVID-19 pandemic, in an academic surrounding of Surgeons’ Quarters at the Royal College of Surgeons of Edinburgh, founded in 1505! We were unsure if we would have in-person attendees. We are fortunate that restrictions were lifted, and we have a good response.

BMLA Executive Council (2022) L-R, Front row: Samira Syed, Reem Hanna, Harry Moseley,
Vasant Oswal, Vishal Madan, Kerry Belba, Kathy Fan Back Row: Jon Exley,
Kerry Muggeson, Tom Lister, Stan Batchelor, Sanjay Rajpara, Raman Bhutani.
There’s nothing like face-to-face contact; the way conferences used to be held prior to the pandemic, will always remain so. There is a bit of a lag in the industry support of the conferences; it may be due to the pandemic affecting their sales; I hope things can return to normality. The next conference is earmarked for Cardiff in May 2023. I would encourage people to attend. Experts conduct several BMLA Education Committee-approved courses on day one. Also, many course organisers in the UK and abroad apply for BMLA-approved status. The Education Committee look at their material, and if it meets our criteria of having high educational value, they gain our approval. That is our contribution to all those involved in all things laser and high-energy devices.
Mr Oswal, thank you very much for your time.
My pleasure and thank you for coming to the conference.
Globe Trotting and 62 Years of ENT by Vasant Oswal
is published by Kugler Publications and available to order free: