How much does the position of a patient add to the risk of a surgical procedure? This is an extremely important question, and the answer is far from simple. All of those involved in surgery will recall the times when a procedure needs to be performed that is not part of the standard repertoire of a particular surgical team. This is a challenge in plastic and reconstructive surgery where a two-team approach is needed for resecting a tumour and reconstructing with a distant free tissue transfer. There are some comprehensive documents available which outline the considerations to be made when positioning patients. A simple Google search will turn up some very clear guidelines and one that impressed me came from the Association of Surgical Technologists (https://www.ast.org/AboutUs/surgical_technologists_responsibilities/#). Guideline 6 concerns patient positioning. It is a downloadable pdf file and gives a comprehensive account of the theoretical and practical aspects of the safe management of patients placed in different positions.
Just a simple exercise for distraction: how many of the following positions could you describe together with all their relevant patient safety features?
- Supine
- Prone
- Lateral
- Sitting
- Fowler
- Jacknife
- Kidney
- Lithotomy
- Sims
- Trendelenburg
- Reverse Trendelenburg
- Kraske
And what about the risks associated with these different positions? Now that is a key question, and one which again raised serious concerns about the nature of the so-called ‘expert opinion’ given by the prosecution experts in the case of Dr Vanessa Kwan. Both experts noted that the prone position of the patient put her at increased risk of cardiorespiratory compromise. This was relayed to the judge and the jury and gave rise to the unfortunate comment by the judge in her reasons for sentence: “Para 68. Lee was a vulnerable patient because of her obesity and the nature of her surgery whilst lying prone.”
Indeed, when we look at the historical advice regarding risks and patient positioning, we find in the early part of this century that the perspective of doctors and nurses in theatre was that the prone position had particular risks and these included: “skin breakdown, reduced respiration, circulation, nerve damage, eye or ear damage, damage to the breasts in women, or genitals in men.” (1). I added the bold emphasis, but it is there clearly stated, “reduced respiration”. This is where terminology becomes important, and we must be clear that from a physiological perspective this is wrong. This was outlined in a paper published almost 10 years later and I quote: “During prone positioning, ventilation is improved due to changes in pleural pressure and the amount of lung atelectasis present,” (2). This is accompanied by a diagram which I reproduce for educational purposes here:
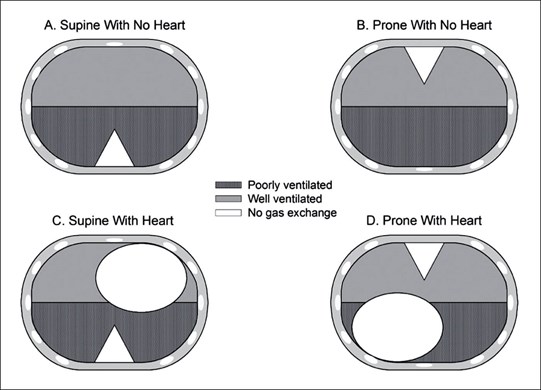
This explains why the prone position is favoured in patients with acute respiratory distress.
This finding has been very important in the COVID-19 pandemic, but also relates to other respiratory problems such as obstructive sleep apnoea. The prosecution anaesthetic expert was presented with this paper, and she dismissed it as not relevant because it concerned people with respiratory distress, not normal people under sedation. This evasive intellectual dishonesty is one of the major problems in complex medico-legal cases. The judge was just not equipped to weigh the arguments for and against admissible evidence, and yet again allowed the prosecution experts to perversely mislead the jury.
COVID-19 has taught us many things and “proning patients” has certainly led to a decrease in the need for mechanical ventilation. Proning is so effective it is recommended for home care (3).
Expert opinions must be based on facts and if you cannot give the facts then keep your opinions to yourself! They are not helpful. Next blog - snoring! What is it and what does it mean?
References:
- Preventing intraoperative positioning injuries. Nursing Management 2006;9-10. [This article was adapted from Graling P, Tea C. Intraoperative nursing management. In: Smeltzer SC, Bare B, eds. Brunner & Suddarth’s Textbook of Medical-Surgical Nursing. Philadelphia, USA: Lippincott Williams & Wilkins; 2003:432-4.
- Henderson William R, Griesdale DEG, Dominelli P et al. Does prone positioning improve oxygenation and reduce mortality in patients with acute respiratory distress syndrome? Can Respir J 2014;21(4):213-5.
- Bentley, Suzanne K, Iavicoli L, Cherkas D et al. Guidance and patient instructions for proning and repositioning of awake, non‐intubated COVID‐19 patients. Acad Emerg Med 2020;27(8):787-791.




