The author explains how treating the face as a 3D structure is key to a good result with invasive or non-invasive procedures.
History
Rejuvenation of the face and trying to reverse the effects of ageing dates back centuries. Facial volume and rhytids are a natural and inevitable part of the ageing process. Over the last 100 years, restoration of volume with injectable devices has been tried, starting as early as 1893, when fat transfer was reported [1]. The first injections of liquid paraffin were performed in Vienna at the beginning of the 20th Century.
The delayed complications of paraffin injections began surfacing around 1914 and its use sharply declined. The name ‘paraffinomas’ was used to describe the delayed, chronic inflammatory reactions of this product. These inflammatory reactions would often progress to ulcerations, fistulas and necrosis [2].
Alternative injectable substances were explored. Facial injections of silicone oil became popular in the 1960s, especially with the description of the microdroplet injection technique. In 1981 bovine collagen (Zyderm®, Zyplast®) became the first Food & Drug Administration (FDA)-approved injectable filler for cosmetic use. Approximately 3 to 3.5% of the population demonstrate hypersensitivity to bovine collagen, requiring skin testing prior to injection. Despite a negative test, 1% of the population will still demonstrate hypersensitivity [3]. The modern era of injection with synthetic bioactive materials began in December 2003 with the FDA approval of Restylane®, a hyaluronic acid product. This had led to a boom in the popularity of injectable fillers.
Characteristics of hyaluronic acid
No matter the type of filler, the basic physical property that the material elicits on the tissue remains the same. The ability of the filler to withstand outside forces that include the movement of the overlying tissue and external pressure forces is known as the G’ (G Prime) of the filler or the elastic modulus. The G’ is calculated in vitro by using an oscillation instrument that exerts pressure on the material to calculate its stiffness or smoothness and thus immediate volume creation. Stiffness, contrary to popular belief, does not translate into the filler’s ‘lifting capacity’. It does not imply resistance of the gel. This property is known as cohesivity and has to do with both the filler’s resistance to degradation in vivo.
For example, biphasic HA fillers are quite stiff owing to their high G’. These fillers during production pass through a mesh of a certain size and thus are dependent on their particle size in their final form. These particles are not adherent to one another when compared to the monophasic materials. Biphasic fillers are not cohesive, thus are more susceptible to degradation. These fillers provide immediate filling capacity but may not have great ‘lifting capacity’ as those with lower G’ but higher cohesivity [4]. In summary, a filler’s lifting capacity is dependent on both the G’ and the cohesivity of the material [5].
Ageing process
As people age, many are left with the feeling that their physical appearance is no longer an accurate representation of their mental state, leaving them with the desire for facial rejuvenation. The face, like other parts of the body, ages in a unique but relatively consistent manner, creating a distinct and recognisable ‘aged’ appearance [6]. The typical aged face represents a combination of changes on many levels, including changes in bony structures, fat volume, muscle and ligament strength, skin properties and vascularity. Many verbs have been used to describe the underlying mechanical changes with ageing, including deflation, attenuation, ‘doubling over’, radial expansion and rotation [7].
In a landmark article in 1965, Gonzalez-Ulloa and Flores described the process of ageing as resulting from the gradual absorption of fat, decreased thickness and elasticity of skin, decreased adherence between the skin and subcutaneous tissue, sagging of the soft tissues, weakening of the orbital muscle and septae, and the progressive decrease in the volume of the craniofacial skeleton [8].
A recent study by Guyuron et al. highlights the importance of environmental factors in the ageing process by analysing identical twins that have led different lifestyles. Smoking and sun exposure were significantly associated with an older appearance, and the use of hormone replacement therapy was associated with a younger appearance. Interestingly, a higher body mass index (BMI) correlated with an older appearance up to age 40, after which it was associated with a younger appearance. This fact highlights the importance of adipose tissue in the aged appearance [9].
Structural components of facial ageing
Skeletal structure
Ageing of the craniofacial skeleton is due to a combination of bone atrophy and a change in the relative dynamics of bone expansion and bone loss [10]. There is an appreciable reduction in facial height, which is mainly due to changes in the maxilla and mandible, and a modest increase in facial width and depth. The orbits increase in size, whereas the maxilla decreases in size, compounding the inferior displacement of the malar fat pad and accentuation of the nasolabial fold. Maxillary resorption can also lead to a loss of support in the upper lip, which contributes to perioral wrinkling. In the mandible, tooth loss causes marked resorption of the alveolar ridge, and the shape and projection of the chin also change with age. There is a general coarsening of mandibular bony protuberances at the points of insertion of masticatory muscles (e.g. the gonial angle and inferior edge of the zygomatic eminence), and a general softening elsewhere.
Subcutaneous fat distribution
The youthful face is characterised by a diffuse, balanced distribution of superficial and deep fat, which confers a well-rounded 3D topography that is delineated by a series of arcs and convexities [11]. Facial ageing is associated with loss of soft tissue fullness in certain areas (periorbital, forehead, malar, temporal, mandibular, mental, glabellar and perioral sites) and persistence or hypertrophy of fat in others (submental, lateral nasolabial fold and labiomental crease, jowls, infraorbital fat pouches and malar fat pad) [12]. In addition to redistribution of facial fat and concomitant loss of surrounding fullness, the fat pockets become more discernible as separate entities, as do many of the underlying facial structures, e.g. the submaxillary glands and bony protuberances. With age, the malar fat pad gradually slides forward and down to bulge against the nasolabial crease, giving rise to the prominence of the nasal fold in the aged face [13]. This redistribution and demarcation of fat gives the senile face an unbalanced appearance.
Skin wrinkling occurs at some sites (periorbital and perioral areas) due to the repeated underlying muscle action to give a progression from dynamic rhytids initially to static rhytids as the skin changes become permanent. Elsewhere (jowl, submental area and nasolabial fold) sagging can occur due to a relative excess of skin and / or lack of elastic recoil as well as fat accumulation. Consequently, the defining arcs and convexities of youth are disrupted. From the front, the jawline appears scalloped, the temporal, buccal and suborbital areas are hollow, and the lips are straight and angular. In profile, the primary arc of the cheek is broken, the mandibular arc is replaced by a jowl line, and the forehead and brow lose their anterior projection.

Figure 1: Patient in her late 30s.

Figure 2: Patient in her late 40s (overweight).

Figure 3: Patient with deflation after bariatric surgery.
The importance of replacing volume
The patient above demonstrates the importance of replacing volume. She is shown in three moments of her life: late 30s, late 40s (overweight) and after bariatric surgery – notice the deflation of her face.
Replacing volume – soft tissue augmentation
The author’s preferred methods of soft tissue augmentation are fat grafting and hyaluronic acid fillers.
Fat injection
Despite a long history of clinical use and the evolution of fat-transfer techniques, no consensus exists on the best technique and the longevity of results, yet the principles of fat reimplantation are based on optimal recipient-site vascularity for increased fat survival [14]. Through a skin incision of a size corresponding to the diameter of the cannula, the fat graft is inserted at the level of the anatomical region affected. Small-gauge cannulas are thought to reduce trauma to the recipient site, thus reducing the risks of bleeding, haematoma formation, and poor graft oxygen diffusion. Because revascularisation starts at the periphery, ischaemic time is longer in the centre of the graft [15].
Therefore, fat reinjection in multiple small-volume sessions is preferred over one single injection. Usually, through multiple access sites, multiple tunnels are created on insertion, but fat is injected only during withdrawal of the cannula in a ‘fanning-out’ pattern. Fat grafts are distributed in small aliquots and fanned out to varying depths in the soft tissue to avoid excessive interstitial pressure at the recipient site and overcrowding of the transplanted adipocytes.
Studies on fat-graft maintenance have demonstrated that mobile areas of the face, such as the glabella and lips, are less amenable to correction than are less-mobile areas, such as the malar and lateral cheek areas. Regarding the cannula size, several authors use different cannulas for fat injection; the nature of the recipient site is the major determinant in the choice of cannula size. Fat grafting continues to be the choice to augment soft tissue during face surgery. In an office-based practice, hyaluronic acid has an important role in soft tissue augmentation due to its predictability and availability.
Hyaluronic acid (HA) dermal fillers
Scientists and physicians are constantly searching for the ideal dermal filler. This ideal filler should be safe, effective, biocompatible, non-immunogenic, easy to distribute and store, and should require no allergy testing. Moreover, from a practitioner’s perspective it should be low cost, have an acceptable persistency, and be easy to remove if necessary. HA dermal fillers have most of these ideal characteristics [14]. HA fillers can easily be removed whenever the practitioner considers necessary by injecting commercially available hyaluronidase into the concerned area. Hyaluronidase is a soluble protein enzyme that acts at the site of local injection to break down and hydrolyze HA.
These important characteristics have made HA-based cosmetic injections the second most popular non-surgical procedure for women and the third most popular procedure for men. Several HA fillers are currently commercially available for mid to deep dermal implantation for the correction of moderate to severe facial wrinkles and folds and to refill the face globally. The technique varies according to the case. The author’s preferred technique is the Redka-Galadari (RG) method. The RG point is an anatomical safe zone located by following a perpendicular line from the lateral canthus to 1cm-2cm below the orbital rim. From this entry point, filler can be deposited throughout the cheek and tear trough area and depending on the size of the cannula, other areas can be treated [15]. It is very important to know exactly where to place the filler to avoid complications.

Figure 4: Fat grafting – the ideal fat prepared.
Complications
Over the past few years, the number of procedures involving soft tissue fillers has increased exponentially [16]. Concomitantly with this, complications are becoming more frequent. The classification of filler complications can be divided according to severity (mild, moderate or severe), nature (ischaemic complications and non-ischaemic), or by the time of the onset (early or late) [17]. A classification proposed by Rohrich et al. [18] suggested that complications should be classified as early, late and delayed, roughly defined as less than 14 days, 14 days to one year, and more than one year, respectively, as these time frames correlate well with the potential underlying aetiology. Although the panel proposed to classify filler complications as immediate onset (up to 24 hours after procedure), early onset (24 hour to four weeks), and delayed onset (more than four weeks), to facilitate the understanding and follow-up of the manuscript, the immediate- and the early-onset complications have been listed together. The most feared complication is blindness which can happen with any type of filler.
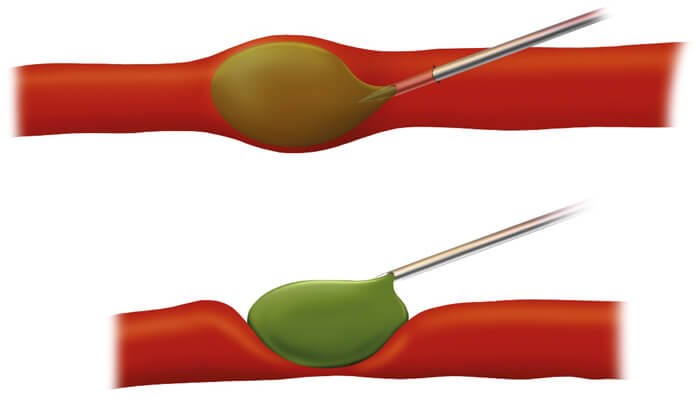
Vascular occlusion is a rare but severe and dreaded complication of soft-tissue fillers. It occurs because of inadvertent injection of the filler material into a blood vessel.
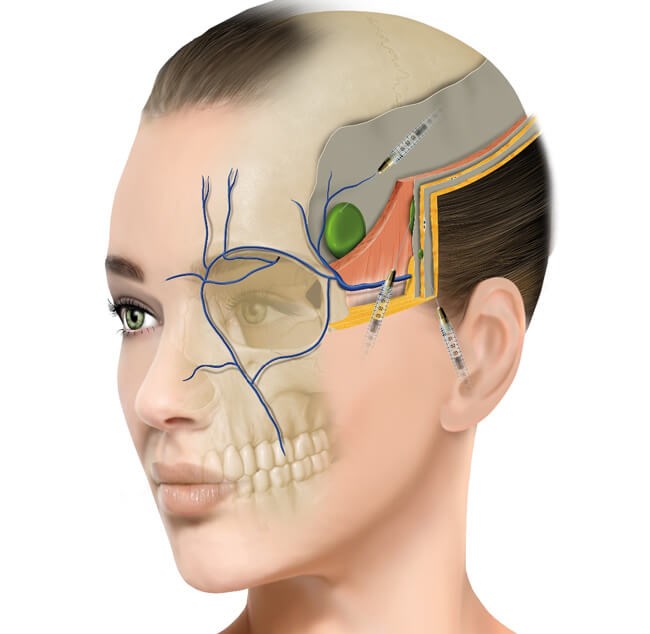
Figure 5: Filler in a deep position in the temporal area.

Figure 6: Before and after treatment of temporal hollowness using HA filler.
Intravascular injection of fillers or extravascular compression causing complication
The intravascular injection of fillers may lead to complications such as tissue ischaemia and loss, blindness, pulmonary embolisation [19] and even stroke. Beleznay et al. showed that almost 47.9% of cases of blindness were caused by autologous fat, whereas HA fillers were responsible for 23.5% of the cases [20]. Autologous fat, the most viscous soft-tissue filler had the highest risk of diffuse occlusion in the ophthalmic artery and was also associated with poor prognosis. It has been seen that hyaluronidase, an enzyme that degrades HA, may improve outcomes following an accidental intravascular HA filler injection. A review conducted by Carruthers et al. [21] showed that when hyaluronidase was injected next to a blood vessel clogged with HA, it catabolised the HA without needing to canalise the affected artery.
It is also suggested that in the case of retinal artery embolisation with the HA product, retrobulbar injection of a large volume of hyaluronidase might well be the single most effective option to dissolve the intraorbital intravascular hyaluronic acid in a time-sensitive manner. Recently, in a rabbit model, hyaluronidase was injected in a retrobulbar area after retinal artery occlusion by hyaluronic acid showed reperfusion. Retrobulbar hyaluronidase may be an effective evidence-based treatment option for humans. Hyaluronidase concentration and injection time are the important factors for faster recovery, but additional studies are still required [22]. All injectors must be prepared to treat complications and a crash kit must be available, along with protocols for a multidisciplinary management of this issue.
Intravascular injection of fillers or extravascular compression causing complication.
Conclusion
The facial ageing process encompasses all layers of the face. Understanding this process and treating the face as a 3D structure is key to a good result. Anatomical knowledge and the choice of the right filler is of upmost importance. Complications do occur and all injectors must be prepared to recognise and treat them immediately.
References
1. Neuber F. Fat grafting. Chir Kongr Verhandl Dtsch Ges Chir 1893;22-66.
2. Schmorl Paraffingranulome. Munch Med Wochenschr 1922;69:215-20.
3. Ashinoff R. Overview: soft tissue augmentation. Clin Plast Surg 2000;27;:479-87.
4. Sundaram H, Voigts B, Beer K, Meland M. Comparison of the rheological properties of viscosity and elasticity in two categories of soft tissue fillers: calcium hydroxylapatite and hyaluronic acid. Dermatol Surg 2010;36 Suppl 3:1859-65.
5. Galadari H. Soft Tissue Augmentation: Principles and Practice. Berlin, Germany; Springer-Verlag; 2018:10-1.
6. Gonzales-Ulloa M. The history of rhytidectomy. Aesthetic Plast Surg 1980;4:1-45.
7. Lambros V. Observations on periorbital and midface aging. Plast Reconstr Surg 2007;120:1367-76.
8. Gonzalez-Ulloa M, Flores ES. Senility of the face: basic study to understand its causes and effects. Plast Reconstr Surg 1965;36:239-46.
9. Guyuron B, Rowe DJ, Weinfeld AB, et al. Factors contributing to the facial aging of identical twins. Plast Reconstr Surg 2009;123:1321-31.
10. Bartlett SP, Grossman R, Whitaker LA. Age-related changes of the craniofacial skeleton: an anthropomorphic and histologic analysis. Plast Reconstr Surg 1992;90:592-600.
11. Hamra ST. The role of orbital fat preservation in facial aesthetic surgery. Clin Plast Surg 1996;23:17-28.
12. Coleman SR. Structural Fat Grafting. St Louis, Missouri, USA; Quality Medical Publishing; 2004.
13. Owsley JQ. Elevation of the malar fat pad superficial to the orbicularis oculi muscle for correction of prominent nasolabial fold. Clin Plastic Surg 1995;22:279-93.
14. Andre P. New trends in face rejuvenation by hyaluronic acid injections. Journal of Cosmetic Dermatology 2008;7:251-8.
15. Galadari H, Redka-Swoboda W. Injection of filler for volume replacement of the whole face using a single-entry method. J Am Acad Dermatol 2017;77(6):163-4.
16. American Society of Plastic Surgeons. 2014 Plastic Surgery Statistics Report.
https://www.plasticsurgery.org/
documents/News/Statistics/2014/
plastic-surgery-statistics
-full-report-2014.pdf
[Last accessed 17 December 2019.
17. Wagner RD, Fakhro A, Cox JA, Izaddoost SA. Etiology, prevention, and management of infectious complications of dermal fillers. Semin Plast Surg 2016;30(2):83-6.
18. Rohrich RJ, Nguyen AT, Kenkel JM. Lexicon for soft tissue implants. Dermatol Surg 2009;35(Suppl 2):1605-11.
19. Sclafani AP, Fagien S. Treatment of injectable soft tissue filler complications. Dermatol Surg 2009;35:1672-80.
20. Beleznay K, Carruthers JDA, Humphrey S, et al. Update on avoiding and treating blindness from fillers: a recent review of the world literature. Aesthetic Surgery Journal 2019;39(6):662-74.
21. Carruthers JD, Fagien S, Rohrich RJ, et al. Blindness caused by cosmetic filler injection: a review of cause and therapy. Plast Reconstr Surg 2014;134(6):1197-201.
22. Lee W, Oh W, Ko HS, et al. Effectiveness of retrobulbar hyaluronidase injection in an iatrogenic blindness rabbit model using hyaluronic acid filler injection. Plast Reconstr Surg 2019;144(1):137-43.
TAKE HOME MESSAGE
-
The ageing process involves changes in all structures of the face; the deflation is the most important factor relating to fillers.
-
Fat grafting is a very good choice to replace volume especially during face surgeries.
-
HA is a safe and effective filler. Its use is increasing worldwide and to master injections, knowledge of anatomy and choosing the right HA is key to a good result.
-
Recognising complications and knowing how to treat them is essential for any injector.
Declaration of competing interests: None declared.
Dr Andre Mattos is one of the speakers at the Dubai Derma 2020 Conference
taking place in Dubai on 15-17 June
Visit https://dubaiderma.com for further information.
COMMENTS ARE WELCOME






