Although the lesion known as Xanthelasma was first described by Addison and Gall in 1851 [1] it was recorded some 300 years previously in the famous painting of the Mona Lisa by Leonardo da Vinci. In this painting, Leonardo da Vinci depicted some skin discoloration of the inner corner of the left upper eyelid. This was spotted recently by an Italian researcher who proposed that this was due to an Xanthelasma.
This suggests that Xanthelasma was prevalent in the 16th century. In addition, the subject of the painting died as a young woman when she was only 37-years-old. It is possible that the Xanthelasma captured by the artist was an indication of a high level of blood lipid and, being a higher risk for ischaemic heart disease, may well have been associated with early demise.
Clinical presentation and prevalence
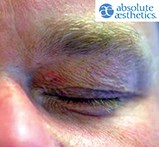
Xanthelasma presents as a yellowish plaque that forms around the eye area, most often near the inner canthus of the eye. Xanthelasmata are rarely, if ever found elsewhere on the face or body. Histologically the plaques are found to be accumulations of lipoprotein deposits. These deposits can vary between being soft to hard and calcareous – the variability usually being due to the chronicity of the plaques. Commonly they develop on the inner corners of the upper and lower eyelids but in more extreme cases they can develop across the entire eyelid area.
The prevalence of Xanthelasmata is still unknown but a publication by Hampton et al. in 2011 suggests that Xanthelasmata are rare in the general population [2]. They tend to effect women more than men and hardly ever effect children under the age of 15. The yellowish deposits tend to grow over time, usually peaking in size between the ages of 40 and 50. Once the yellow deposits have become established around the eye, they tend to enlarge over time but almost never regress spontaneously. Fortunately however, the presence of these plaques and deposits in the skin tends not to affect the eye or eyelid function.
Causes and associations
Xanthelasmata are easily recognised by the general public by sight if not by name and the condition is commonly identified as being linked to having a high cholesterol and elevated blood pressure. However, although a study by Christoffersen et al. in 2011 suggests that it can be a predictor of risk for myocardial infarction, ischaemic heart disease and atherosclerosis [3], there is very little research available on the exact cause of Xanthelasmata. Due to the nature of discoloured plaques around the eyes, Xanthelasmata are cosmetically upsetting, hard to hide and are a source of considerable worry for many patients. Fortunately, despite the worries of many patients, it is known that there is no malignant potential from these lesions.
As is the case with many conditions the pathogenesis of Xanthelasmata is unclear. In a personal series of over 55 patients many have normal cholesterol levels and normal blood pressure. One of my patients is convinced that their Xanthelasma developed following a trauma to the eye area, despite their blood pressures and cholesterol level being normal.


Treatment
As Xanthelasmata can be associated with cardiovascular disease and high lipid / cholesterol levels, all patients presenting with Xanthelasmata should have a cardiovascular review including history and basic clinical examination. Blood tests should be sent for fasting cholesterol and lipid levels and an electrocardiogram (ECG) should be considered if there is any concern.
Once significant cardiovascular disease has been excluded and any high blood pressure, hypercholesterolaemia or hyperlipidaemia has been either excluded or treated, attention can be turned to the Xanthelasmata.
The lesions of Xanthelasmata are not dangerous in themselves but their presence can have a significant psychological effect on the patient and many request removal for cosmetic reasons. Various treatment options are available but most have limited effectiveness and none of them are currently entirely satisfactory.
Different treatments that are offered to patients include:
- Conservative management – the advice to leave the lesions alone and untreated is often given by patients’ GPs as Xanthelasmata is a benign condition and is thought to be a difficult lesion to remove with a good cosmetic result.
- Topical trichloroacetic acid (TCA) application [4].
- Surgical excision [5].
- Lasers including Q-Switched Nd:YAG [6], KTP [7], Er:YAG [8].
- Garlic therapy (the application of pureed garlic applied to the area) [9].
Some published research shows good results from some of these treatments. However they can leave hypo or hyperpigmented areas as well as scars and, depending on treatment, they can be expensive, with varying degrees of downtime.
Advanced electrolysis for Xanthelasma removal
After seeing a number of patients who were unhappy with the failure of previous treatments or who did not like the idea of surgery I decided to try another approach. I had been having considerable success in treating a variety of other skin lesions using ‘advanced electrolysis’, a form of minor electrosurgery using a simple clinical electrolysis machine. Electrolysis was invented in 1875 by Dr Charles E Michel and was developed for the treatment of Trichiasis (ingrowing eyelashes).
Electrolysis has often been associated with ‘beauty treatments’ as it is widely practised for permanent hair removal. Over the years techniques have advanced and electrolysis is now used to treat a number of cutaneous lumps, bumps and skin lesions. These include seborrhoeic keratosis, syringoma, milia, sebaceous hyperplasia and skin tags. The treatment of these cutaneous and sub-cutaneous lesions is termed ‘advanced electrolysis’ to draw a clear distinction between the level of training and knowledge needed over and above the use of the technique for simple hair removal.
Advanced electrolysis has become one of the most popular treatments in my clinic and has shown to be suitable for most people needing the safe removal of benign skin lesions that are irritating or unsightly. Over recent years I have been developing and perfected techniques for treating various lesions that are not usually deemed within the scope of treatment by this technique. Such lesions include Xanthelasmata [10], dermatosis papulosa nigra (DPN) [11,12] and, most recently, epidermal skin cysts on the scrotum [13].
In view of the low cost, low downtime, low risk of scaring and minimally invasive nature of advanced electrolysis, it is surprising that this method of treating skin lesions as well as some superficial sub-cutaneous lumps and bumps is not widely known or recognised by many doctors and nurses.

Technique
The treating of Xanthelasmata with advanced electrolysis is conducted in a clean, non-sterile environment. I use a one piece stainless steel and short wave diathermy on fairly low settings (17-19Hz).
First, I use the fine needle to lift the fine epithelial layer of the skin covering the Xanthelasma to expose the yellow plaque underneath. Then, depending on the size, location and length of time the patient has had the Xanthelasma, I choose one of two of my preferred techniques for treatment. I refer to these two techniques as either ‘scratching’ or ‘dotting’.
To perform the ‘scratching’ technique, once the fine epithelial layer covering the plaques has been lifted, then the needle is worked over the area, gradually lifting the deposit from the skin. This method is used for the softer deposits and the plaque can be lifted with the aid of forceps.
I use the ‘dotting’ technique for Xanthelasmata that have been there for a number of years as they are often harder to lift, but respond well to being cauterised in situ. This technique involves the activation of the current and then repeated tapping of the plaque with the tip of the needle, allowing the heat to accumulate in the area. This can be seen as the plaque starts to darken and crust. To minimise the risk of scarring, particularly for the darker skin types, the dotting technique is used, cauterising the lesion in situ and then allowing the debris of the lesion to come away when the scab forms.
Using either technique, the treatment can be uncomfortable during the procedure itself. However the sensation passes as soon as the treatment is complete. There is no discomfort following the treatment and so local anaesthetic is generally not required.
Once the treatment is complete, the area resembles a graze and the scab that forms can remain on the area for between seven to ten days. When the scab comes away the pink skin underneath can naturally take a few weeks to settle and blend in with the skin colour.
Results
Using advanced electrolysis and these two different techniques, I have treated over 55 patients to date. More than one treatment episode might be required depending on the number of lesions and patient choice, but it is rare to need to treat a single lesion more than once. At four-week follow-up, my patient satisfaction rate has been 98%. I am currently developing the technique further and will be presenting and publishing my research in the near future.
Advantages of advanced electrolysis as a treatment for Xanthelasma
- Very little downtime
- No local anaesthetic is required
- Relatively low cost compared to other methods of treatment available
- Minimal or no postoperative scarring / blemishes.
References
1. Dequeker J, Muls E, Leenders K. Xanthelasma and lipoma in Leonardo da Vinci’s Mona Lisa. Isr Med Assoc J 2004;6(8):505-6.
2. Hampton Roy Sr, et al. Xanthelasma. Medscape 6 October 2011.
3. Christoffersen M, Frikke-Schmidt R, Schnohr P, et al. Xanthelasma, arcus corneae, and ischaemic vascular disease and death in general population: prospective cohort study. BMJ 2011;343:d5497.
4. Haque MU, Ramesh V. Evaluation of three different strengths of trichloroacetic acid in xanthelasma palpebrarum. J Dermatolog Treat 2006;17:48-50.
5. Lee HY, Jin US, Minn KW, Park YO. Outcomes of surgical management of xanthelasma palpebrarum. Arch Plast Surg 2013;40(4):380-6.
6. Fusade T. Treatment of xanthelasma palpebrarum by 1064-nm Q-switched Nd:YAG laser: a study of 11 cases. Br J Dermatol 2008;158(1):84-7.
7. Berger C, Kopera D. KTP laser coagulation for xanthelasma palpebrarum (German). J Dtsch Dermatol Ges 2005;3(10):775-9.
8. Mannino G, Papale A, De Bella F, et al. Use of Erbium:YAG laser in the treatment of palpebral xanthelasmas. Ophthalmic Surg Lasers 2001;32(2):129-33.
9. Xanthelasma.
http://www.hxbenefit.com/xanthelasma.html
Last accessed December 2013.
10. Smith VC. Xanthelasma - case series (Presentation and abstract). IMCAS Paris January 2012.
11. Smith VC. Dermatosis Papulosa Nigra - case series (Presentation and abstract). IMCAS Shanghai July 2012.
12. Smith VC. Dermatosis Papulosa Nigra - case series (Presentation and abstract). IMCAS Paris January 2013.
13. Smith VC. Early experiences of a new treatment technique for Scrotal Skin Cysts (Presentation and abstract). IMCAS Goa November 2013.
Declaration of competing interests: None declared.
EDITOR’S COMMENT
I must congratulate the author on sharing this experience which opens up a whole new area for discussion. The reality is that when the debate about what constitutes a ‘medical’ or a ‘beauty’ treatment is led by the medical profession then it is going to be biased. That is human nature. Electrolysis is going to treat sub-epidermal structures and there are those who claim this should only be undertaken by medically trained specialists. Now we are being presented with ‘advanced electrolysis’ which some would regard as an even more audacious advance into medical territory. I am a plastic surgeon who loves the Hyfrecator™ and I know there are those in my specialty who regard this device with disdain as being a tool for dermatologists. We need more discussion and informed debate and this is the platform for all to air their views. Please email diana@pinpoint-scotland.com with your comments.