The authors, from the University of Catania in Italy, discuss the promise that erythema-directed digital photography is showing in the clinical evaluation and targeted treatment of rosacea.
Rosacea is a common chronic inflammatory facial condition that can lead to significant facial disfigurement and emotional suffering. Classically it manifests with four broad clinical subtypes (erythematotelangiectatic rosacea (ETR); papulopustular rosacea (PPR), phymatous rosacea; ocular rosacea) [1-2] and different cutaneous symptoms, including persistent centrofacial erythema (background erythema), visible blood vessels (telangiectasias), inflammatory lesions (papules / pustules), oedema, rhinophyma and ocular symptoms.
In clinical practice, different combinations of subtype / cutaneous symptoms (phenotypes) are often seen and therefore a classification based on phenotypes rather than subtypes has recently been suggested [3-5].
The diagnosis of rosacea is mostly clinical and generally easy, however, it may be difficult to assess the clinical features or severity grade for a correct diagnosis and optimal treatment.
New therapeutic topical options for rosacea include brimonidine 0.33% gel and ivermectin (IVM) 1% cream which are able to control persistent erythema in ETR and inflammation in PPR respectively. In particular, brimonidine tartrate is a highly selective α2-adrenergic receptor agonist characterised by a marked vasoconstriction effect [6] and ivermectin is a macrolide agent isolated from the fermentation of Streptomyces avermitilis with anti-inflammatory and anti-parasitic effects [7-8]. Therapeutic effectiveness of these current topical options is based generally on clinical observation of either reduction of persistent erythema or inflammation.
Non-invasive imaging systems, like the VISIA-CR™ system (Canfield Scientific Inc., Fairfield, NJ, USA), can be used to optimise treatment outcomes more precisely than simple clinical inspection or standard photography. In particular, this system is equipped with RBX™ technology (erythema-directed digital photography) which is able to highlight the red areas corresponding to increased vascular flare / inflammation in some facial inflammatory dermatoses including rosacea [9-10], acne [11] and seborrheic dermatitis [12-14].
The aim of this article is to investigate whether erythema-directed digital photography may enhance the clinical evaluation in rosacea patients so as to identify the most appropriate treatment for both ETR and PPR.
How to facilitate treatment decision-making in a group of ETR patients with both background erythema and telangiectasias?
Erythematotelangiectatic rosacea is characterised by flushing (transient erythema), persistent centrofacial erythema (background erythema), and telangiectasias. The severity of individual symptoms differs in each patient and this may complicate the selection of a targeted treatment. Treatment decisions should be made based on the severity of individual symptoms. We have previously demonstrated that erythema-directed digital photography might be useful to facilitate treatment decision-making through better differentiation of the main clinical features of ETR [9].
Example cases
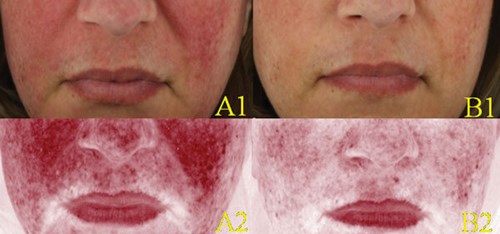
Figure 1: Scenario one: Clinical (A1-B1) and erythema-directed photography (A2-B2) of a patient affected by ETR presenting at baseline with marked background erythema and minimal telangiectasias (A1-A2). Excellent response six hours after topical application of brimonidine 0.33% gel, with marked reduction of background erythema and persistence of minimal telangiectasias (B1-B2).
Patient one (Figure 1) was a 44-year-old Caucasian female affected by ETR with marked background erythema and minimal telangiectasias for five years. She had received no previous rosacea therapy. Erythema-directed photography of the patient after six hours of application of brimonidine 0.33% gel showed marked reduction of background erythema and reduction of some teleangiectasias (scenario one, excellent response).
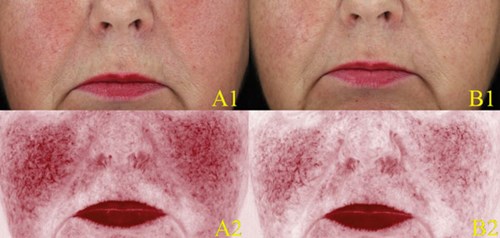
Figure 2: Scenario two: Clinical (A1-B1) and erythema-directed photography (A2-B2) of a patient affected by ETR presenting at baseline with marked background erythema and marked telangiectasias (A1-A2). Good response six hours after topical application of brimonidine 0.33% gel, with marked improvement of background erythema and persistence of telangiectasias (B1-B2).
Patient two (Figure 2) was a 60-year-old Caucasian female affected by ETR with both marked background erythema and telangiectasias for 20 years. She had been unresponsive to conventional rosacea treatment. Erythema-directed photography of the patient after six hours of application of brimonidine 0.33% gel showed marked improvement of background erythema and persistence of telangiectasias (scenario two, good improvement).
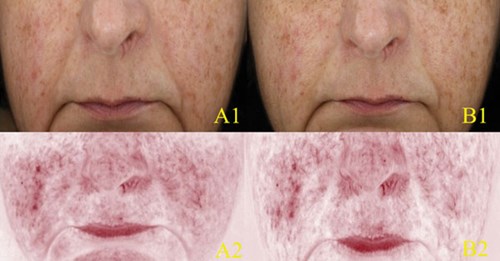
Figure 3: Scenario three: Clinical (A1-B1) and erythema-directed photography (A2-B2) of a patient affected by ETR presenting at baseline with minimal background erythema and marked telangiectasias (A1-A2). Poor response six hours after topical application of brimonidine 0.33% gel, with minimal reduction of background erythema and persistence of telangiectasias (B1-B2).
Patient three (Figure 3) was a 53-year-old Caucasian female affected by ETR with minimal background erythema and marked telangiectasias for 25 years. She had been unresponsive to conventional rosacea treatment. Erythema-directed photography of the patient after six hours of application of brimonidine 0.33% gel showed minimal reduction of background erythema and persistence of telangiectasias (scenario three, poor response to treatment).
Suggested management in ETR patients based on preliminary erythema-directed photography evaluation of the vascular component Based on these erythema-directed photography findings, we suggest a targeted rosacea management as follows:
- Persistent erythema characterised mainly by background erythema (scenario one) is best managed by topical brimonidine.
- Background erythema associated with marked telangiectasias (scenario two) by a combined approach of topical brimonidine and vascular laser (Figure 4).
- Predominant telangiectasias with minimal background erythema (scenario three) by vascular laser only [10].
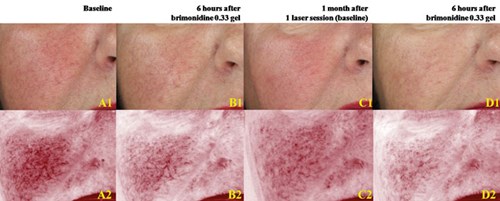
Figure 4: Scenario two: Clinical (A1-D1) and erythema-directed photography (A2-D2) of a patient affected by ETR presenting at baseline with marked background erythema and marked telangiectasias (A1-A2). Moderate response six hours after topical application of brimonidine 0.33% gel, with reduction of the background erythema but persistence of telangiectasias (B1-B2). One month after one session of Nd:YAG laser, disappearance of most of the telangiectasias (C1-C2). Further topical application of brimonidine after 6 hours determined marked reduction of background erythema (D1-D2).
Is it possible to enhance the clinical evaluation of PPR patients under treatment with IVM 1% cream?
In clinical practice, simple clinical observation does not allow for establishing either an accurate rosacea grading score at baseline or a correct post-treatment efficacy and tolerability evaluation. One study has evaluated the use of erythema-directed photography to enhance the evaluation of severity grading and therapeutic monitoring in a group of PPR patients [15].
Twenty patients with mild / moderate PPR were instructed to apply IVM 1% cream for eight weeks. Clinical efficacy was evaluated by 1) Investigator Severity Assessment (ISA) at baseline (T0), at two (T1), four (T2), six (T3), and eight (T4) weeks using a five-point scale (0=clear: no erythema, no papules / pustules; 1=almost clear: very mild erythema, very few small papules / pustules; 2=mild: mild erythema, few small papules / pustules; 3=moderate: moderate erythema, several small or large papules / pustules; 4=severe: severe erythema, numerous small and / or large papules / pustules), and by 2) Investigator Global Assessment (IGA) of efficacy at week eight using a six-point scale: (-1=worsening; 0=no response; 1=mild response:<50% improvement; 2=moderate: 50-80% improvement; 3=excellent: >80% improvement; 4=complete response / clear).
Instrumental evaluation of erythema was evaluated by erythema-directed digital photography at all time points by a five-point scale (0=no erythema; 1=very mild erythema; 2=mild erythema; 3=moderate erythema; 4=severe erythema). Data was analysed using the paired sample t-test (SPSS software). Nineteen patients (16 female / 3 male; mean age: 46.9 years) completed the study. One patient dropped out for local skin reactions. The results showed that at baseline no differences from ISA (mean value: 2.7±0.5) and erythema-directed digital photography (mean value: 2.7±0.5) mean values were found.
After two weeks of treatment, no clinical difference was found at ISA (mean from 2.7±0.5 at baseline to 2.7±0.5 at two weeks) whereas a significant decrease of erythema was detected by erythema-directed digital photography (mean from 2.7±0.5 at baseline to 2.4±0.7; p=0.02). At four, six and eight weeks, a significant reduction of rosacea severity was observed at ISA (mean from 2.7±0.5 at baseline to 2±0.9 at four weeks, to 1.5 ±1.1 at six weeks, to 1.1±1 at eight weeks; p<0.001) correlating with a significant decrease of erythema degree by digital photography (mean from 2.7±0.5 at baseline to 2±0.9 at four weeks, to 1.6±1.2 at six weeks, to 1.1±1 at eight weeks; p<0.001) (Figure 5). IGA at eight weeks showed complete response in six cases (31.6%), excellent in five (26.3%), moderate in three (15.8%), mild in three (15.8%), and no change in two cases (10.5%). The study confirmed the efficacy of IVM 1% cream leading to complete response in 31.6% of patients at eight weeks and highlights the value of erythema-directed photography allowing clinicians to see changes not visible with the naked eye as early as week two.
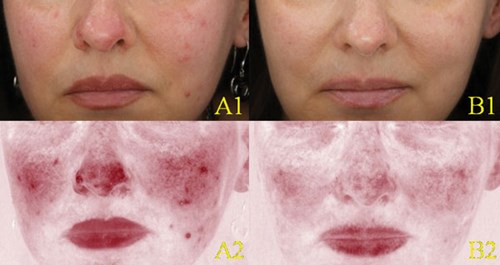
Figure 5: Clinical (A1-B1) and erythema-directed photography (A2-B2) of a patient affected by moderate PPR showing at week eight (B1-B2) complete / clear response compared to baseline (A1-A2).
Conclusions
The use of non-invasive, diagnostic, imaging techniques is experiencing increased popularity in the dermatologic community. Among these, dermatoscopy is the most common followed by reflectance confocal microscopy [16] and optical coherence tomography [17] which are mostly used for clinical research.
In our studies we have demonstrated that erythema digital photography is a novel, simple and interesting technique able to evaluate the rate and the extension of increased vascularity in different facial dermatoses, especially rosacea.
References
1. Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol 2002;46(4):584-7.
2. Wilkin J, Dahl M, Detmar M, et al. National Rosacea Society Expert Committee. Standard grading system for rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol 2004;50(6):907-12.
3. Gallo RL, Granstein RD, Kang S, et al. Standard classification and pathophysiology of rosacea: The 2017 update by the National Rosacea Society Expert Committee. J Am Acad Dermatol 2018;78(1):148-55.
4. Tan J, Almeida LM, Bewley A, et al. Updating the diagnosis, classification and assessment of rosacea: recommendations from the global ROSacea COnsensus (ROSCO) panel. Br J Dermatol 2017;176(2):431-8.
5. Van Zuuren EJ. Rosacea. N Engl J Med 2017;377(18):1754-64.
6. Jackson JM, Knuckles M, Minni JP, et al. The role of brimonidine tartrate gel in the treatment of rosacea. Clin Cosmet Investig Dermatol 2015;8:529-38.
7. Siddiqui K, Stein Gold L, Gill J. The efficacy, safety, and tolerability of ivermectin compared with current topical treatments for the inflammatory lesions of rosacea: a network meta-analysis. Springerplus 2016;5(1):1151.
8. Sahni DR, Feldman SR, Taylor SL. Ivermectin 1% (CD5024) for the treatment of rosacea. Expert Opin Pharmacother 2018;19(5):511-6.
9. Micali G, Gerber P, Lacarrubba F, Schäfer G. Improving treatment of erythematotelangiectatic rosacea with laser and/or topical therapy through enhanced discrimination of its clinical features. J Clin Aesthet Dermatol 2016;9(7):30-9.
10. Micali G, Dall’Oglio F, Verzì A, et al. Treatment of erythemato-telangiectatic rosacea with brimonidine alone or combined with vascular laser based on preliminary instrumental evaluation of the vascular component. Lasers Med Sci 2018;33(6):1397-1400.
11. Micali G, Dall’Oglio F, Tedeschi A, Lacarrubba F. Erythema-directed digital photography for the enhanced evaluation of topical treatments for acne vulgaris. Skin Res Technol 2018;24(3):440-4.
12. Dall’Oglio F, Tedeschi A, Guardabasso V, Micali G. Evaluation of a topical anti-inflammatory/antifungal combination cream in mild-to-moderate facial seborrheic dermatitis: an intra-subject controlled trial examining treated vs. untreated skin utilizing clinical features and erythema-directed digital photography. J Clin Aesthet Dermatol 2015;8(9):33-8.
13. Dall’Oglio F, Tedeschi A, Fusto C, et al. A novel cosmetic antifungal/anti-inflammatory topical gel for the treatment of mild to moderate seborrheic dermatitis of the face: an open-label trial utilizing clinical evaluation and erythema directed digital photography. G Ital Dermatol Venereol 2017;152(5):436-40.
14. Dall’Oglio F, Lacarrubba F, Luca M, et al. Clinical and instrumental evaluation of a new topical non-corticosteroid antifungal/anti-inflammatory/antiseborrheic combination cream for the treatment of mild-to-moderate facial seborrheic dermatitis. Clin Cosmet Investig Dermatol 2019;12:103-8.
15. Dall’Oglio F, Lacarrubba F, Luca M, et al. Clinical and erythema-directed imaging evaluation of papulo-pustular rosacea with topical ivermectin: a 32 weeks duration study. J Dermatol Treat 2019;20:1-5.
16. Sattler EC, Hoffmann VS, Ruzicka T, et al. Reflectance confocal microscopy for monitoring the density of Demodex mites in patients with rosacea before and after treatment. Br J Dermatol 2015;173(1):69‑75.
17. Urban J, Siripunvarapon AH, Meekings A, et al. Optical coherence tomography imaging of erythematotelangiectatic rosacea during treatment with brimonidine topical gel 0.33%: a potential method for treatment outcomeassessment. J Drugs Dermatol 2014;13(7):821-6.
TAKE HOME MESSAGE
-
Rosacea is a chronic, inflammatory and vascular condition of the face classically characterised by four broad clinical subtypes and different cutaneous symptoms. In clinical practice, a combination of different clinical subtypes / cutaneous symptoms (phenotypes) may frequently be seen.
-
The diagnosis of rosacea is mostly clinical and generally easy. However, sometimes it may be difficult to assess clinical features or severity grade for a correct diagnosis and optimal treatment.
-
New therapeutic options for rosacea include brimonidine 0.33% gel and ivermectin 1% cream, which control background erythema in ETR and inflammatory lesions in PPR, respectively.
-
Erythema digital photography provides additional clinical information in many facial disorders, including rosacea.
-
In ETR patients, erythema digital photography allows at baseline to better identify vascular alterations (background erythema and telangiectasias) so as to select a targeted therapeutic strategy, which includes brimonidine 0.33% gel or vascular laser or a combination thereof.
-
In PPR patients, erythema digital photography represents a promising tool for a more accurate severity grading evaluation of erythema related to inflammation during treatment with IVM 1% cream, especially at an early stage in which clinical assessment only may be limited.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME





