From liposuction to adipose stem cells; from regenerative medicine to tissue engineering; and a vision of the future.
Part 1
The history of attempts to sculpture fat dates back to the beginning of the 20th century, but Professor Yves-Gerard Illouz was the first to introduce a new, safe and widespread method of liposuction. This involved the preoperative injection of local anaesthesia, saline, distilled water, adrenaline and hyaluronidase. This was widely called the wet technique, and established a safe and effective adjunct to lipoaspiration.
This procedure was initially based on an automatic pump system; subsequently the efficacy of syringe aspiration was popularised in the 1980s. Liposuction in the subcutaneous tissue, just 3-4mm deep to dermis, also called superficial liposuction, is a modern and effective evolution of the technique, but requires significant experience in order to avoid disfiguring outcomes. Ultrasound and laser lipoplasty methods have provided further choices in the range of technical weapons offered to the plastic surgeon.
Liposuction is a purely surgical procedure, and as such, carries risks of minor and major complications. Since the 1980s there has been a steady increase in the interplay between surgical recontouring procedures and liposuction performed simultaneously such as alipoabdominoplasty, lipoinerthighplasties and facial rejuvenation. Reinjection of harvested fat with the purpose of liposculpture for both reconstructive and cosmetic indications is a relatively recent development which has been established as a successful, globally accepted procedure. Adipose derived stem cells, extracted from the unlimited source represented by human adipose tissue, have great promise for future tissue-engineering.
Liposuction has nowadays become a safe, effective, popular procedure for contouring adipose tissue and the human body in general, in many reconstructive and cosmetic indications. PMFA News is delighted to be publishing a series of three articles from Prof Illouz describing the evolution of liposuction and adjunct techniques. In the first article he discusses the development the classical technique.
Introduction
The first reported attempt at surgical sculpting of fat for cosmetic purposes is most commonly attributed to Dr Charles Dujarrier in 1921. He was a widely respected French general surgeon and the Chief of the Department of Surgery at Saint Antoine Hospital. He had a patient who was a professional dancer who wanted to improve the shape of her ankles and knees. Dujarier performed an excision of excess skin and subcutaneous tissue from her calf but the result was catastrophic.
He had removed too much tissue and there was excessive tension in the closure. This caused necrosis and amputation and resulted in the first lawsuit in the history of plastic surgery [1] (Editor’s note: it is ironic indeed that the procedure was not performed by a plastic surgery specialist but the specialty takes the blame!) Dujarrier was condemned in the first instance, but absolved in appeal because the procedure was done without charge. (Editor’s note: another irony in that incompetent surgeons can too often avoid accountability for spurious reasons.)

Figure 1: The first patient was a lipoma of the back.
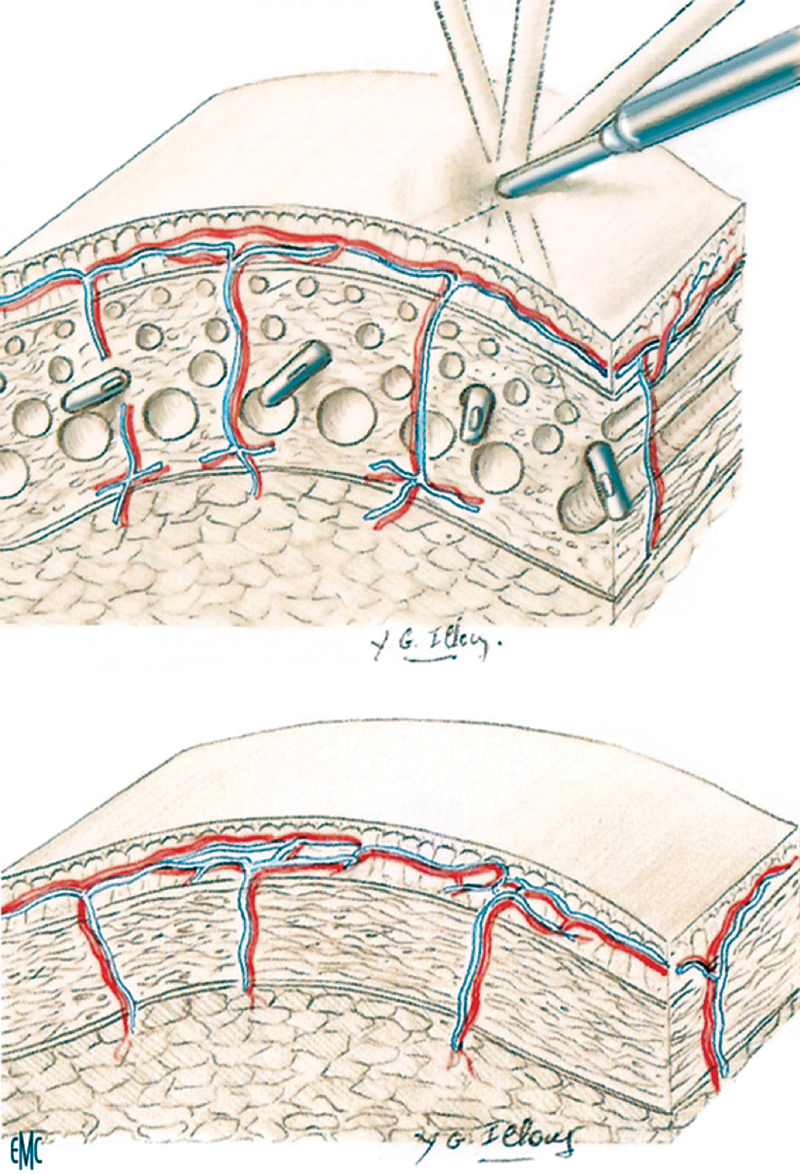
Modern fat extraction began approximately 40 years ago, initially as a closed technique, when the German physician Schrudde first published his technique using a uterine curette to remove subcutaneous fat. Several other surgeons, including Kesselring and Meyer, used this technique in the mid-1970s, and combined this with aspiration to remove more fat. However, frequent complications including persistent lymphorrhea, haematoma, skin necrosis and localised skin excess, brought the procedure into disrepute [2,3]. In 1977 one of the author’s patients made the request for a large lipoma to be removed without leaving a scar (Figure 1). In order to meet this challenge the author developed a blunt cannula technique with the aim of avoiding the serious complications previously associated with lipoaspiration. An important adjunct to the surgical procedure was the preoperative preparation subsequently referred to as the ‘wet’ technique which resulted in minimal blood loss and preservation of the neurovascular septi (Figure 2). This novel and pioneering technique was disseminated to physicians of different specialties throughout the world [4] and the blunt cannula liposuction technique became the global standard of care for liposuction [5, 6].
Figure 2: The round tipped blunt cannula avoids destruction of vessels
and nerves and only removes fat. It is a ‘Swiss cheese technique’.
Patients and methods
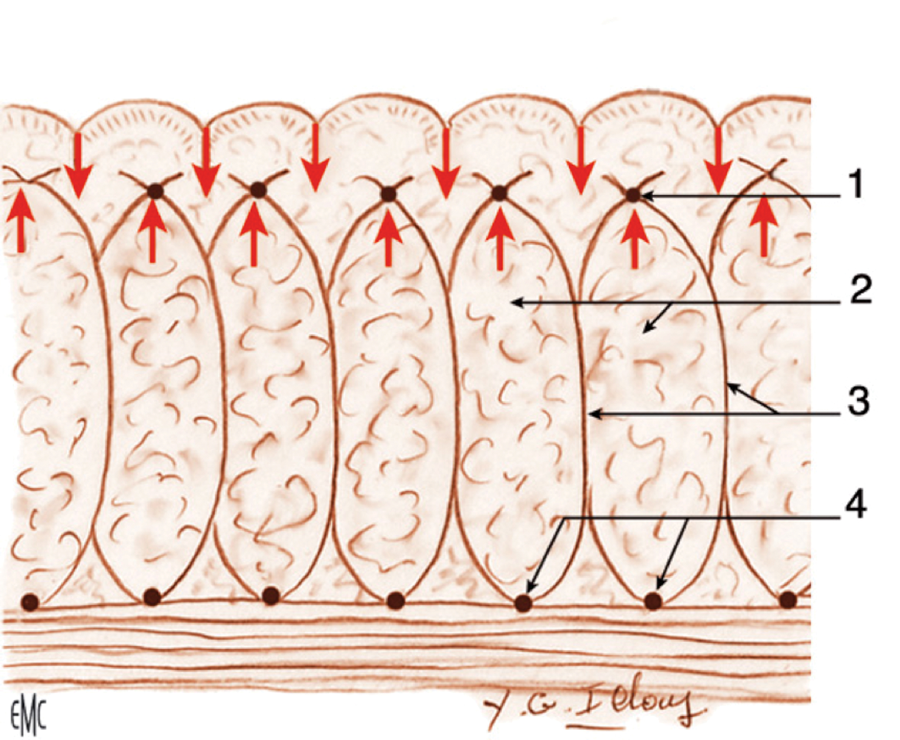
Patient selection is of major importance and is perhaps the most critical factor for a safe and aesthetically satisfying result in body contouring [3]. Not all patients who request liposuction are good candidates. Liposuction is a technique of body contouring rather than weight loss, and potential surgical candidates must be advised and counselled carefully on what results they can realistically expect. It has been proven that liposuction is not a treatment modality for cellulite (Figure 3) and these patients should be warned that only the contour will improve but not the quality of the skin [7,8].
Figure 3: Explanation of cellulite hormone dependant. Only females have cellulite. The female subcutaneous tissue has ‘septi’ which go from the dermis to the fascia superficialis. These septi are extensible laterally but not vertically. As soon as there is a hypertrophy of the subcutaneous fat, bulges appear and that is ‘cellulite’. As soon as androgen hormone appears (as in men) these septi disappear. But a liposuction of the deep plane will not change this phenomenon.
1975-1995: the evolution of suction lipectomy
Initially the author used three different sizes of blunt-tipped cannulas (Figure 4) depending on the area to be aspirated. A 10mm cannula was used for the flanks, buttocks and hip areas; an 8mm cannula was used for the knees, ankles, abdomen and arms; and lastly a 5mm cannula was used for the face.
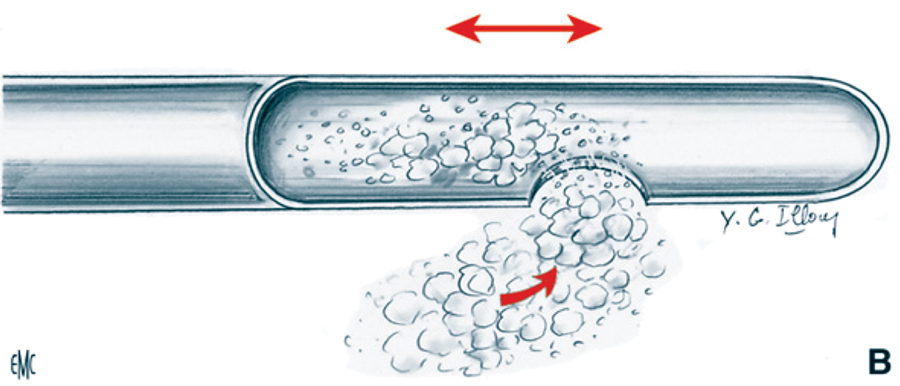
Figure 4: Blunt-tipped cannula designed by Illouz. The back and forth movements combined
with suction, suck out the fat and the round tip avoids damage to vessels or nerves.
The wet technique, or ‘dissecting hydrotomy’, was another aspect of controversy and evolution. The initially described hypotonic formula comprised of normal saline, distilled water and hyaluronidase. Fifteen years later the formula was still: 1000ml normal saline, 200ml distilled water, but with the addition of 1mg epinephrine, and 60mg of lidocaine [9]. Over time plastic surgeons argued in favour of hydrotomy. The ‘wet technique meant dry surgeon’, meaning that hydrotomy makes the procedure significantly less exhausting. The greatest advantage of hydrotomy, however, is the magnification of the deep fat layer that needs to be aspirated. This enables the surgeon to remain in the proper deep layer while preserving the superficial fat. In addition, there was significantly less bleeding with the wetting approach especially after the addition of epinephrine to the wetting solution [10]. As recently reported in a large series, surgeons have been using the Ilouz wet technique (1:1 ratio between volume aspirated and volume injected) as they find it superior to ‘superwet’ and tumescent technique in terms of complications [11].
Liposuction was was originally described as a mechanised procedure in which suction was achieved by aspiration through a vacuum pump [12]. Since 1988 [13], Pierre Fournier (France) and Luiz Toledo (Brazil) have proposed the use of an automatic pump with disposable syringes of various sizes and gauges. With syringe liposuction, an exact knowledge of the aspirated volume in each body area is possible and also allows for more mobility for the operator who is no longer restrained by the aspirating tube and this facilitates the procedure. In addition, at the completion of the operation the precise quantities of local anaesthesia infiltrated, the total aspirated and the percentage of pure fat harvested in each region can be recorded. This essential data cannot be calculated with precision when using the lipoaspirator. Utilised syringes have a volume of 60ml and the model is ‘toomey-tip’, with lumen of 8mm [14,15].
Modern cannulas are made of zirconium, internally and externally. This reduces friction both in fat aspiration and fat injection. Suction lipectomy was also used for lipoaspiration of the submental and nasolabial sulcus areas. Obesity, formally a clear exclusion, was no longer considered as such. Serial procedures were performed with a minimum interval of six months to achieve a satisfactory result [16]. There is no doubt that excessive aspiration of fat can result in severe complications including death, and any volume above five litres was still considered dangerous.
One major breakthrough was the introduction of ‘suction abdominoplasty’. Patients with a combination of excess infraumbilical skin and large fat volume in the supraumbilical area could benefit from this procedure [8,17-21]. Advancement in instrumentation, techniques and devices has moved suction lipectomy forward.
1995-2010: the modern era
Since there are no absolute dogmas in medicine the evolution and further refinement of liposuction was inevitable. Advancement in instrumentation, techniques and devices has taken liposuction to a new era.
Taboo zones (Figure 5) were no longer considered ‘out of bounds’ and hence all of the body could be reshaped with very satisfying results.
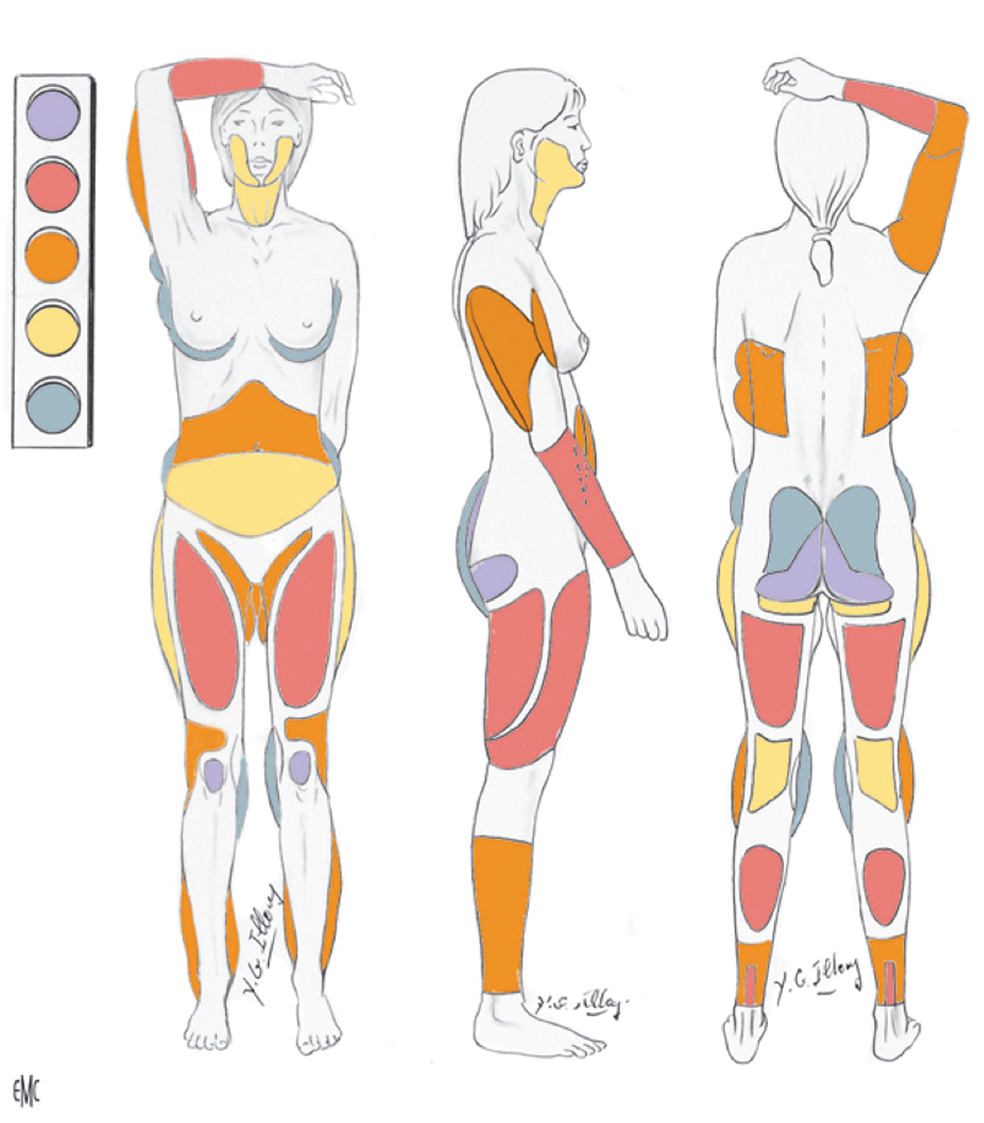
Figure 5: Scheme drawn by Illouz to explain the different level of difficulty: from green
(forgiving areas) to orange (difficult areas) to red (forbidden areas) and dark (absolutely taboo).
The author designed a multi-hole tetrafluoroethylene coated cannula with one lower and two lateral openings on each side (Figure 6) improving the geometry of tunnels by avoiding leaving excess fat tissue in between them. In addition, the incorporation of Teflon made the surgeon’s task significantly easier as the cannula could traverse the tissues with minimal effort [8].

Figure 6: The new designed Illouz cannula with one ventral hole and two lateral holes
in each side to suck in the same time a deep plane and a more superficial plane.
The development of more advanced, narrower cannulas led to the trend of superficial lipoplasty, where the surgeon could aspirate the superficial fat just 3-4mm subdermal. The author had used this approach from the very beginning but always insisted that sufficient thickness should be left under the skin to avoid injuries that would later lead to inappropriate healing and dimpling of the skin. As a result he recommended that the opening of the cannula should be directed downwards to avoid the aforementioned sequelae.
“Advancement in instrumentation, techniques and devices has taken liposuction to a new era.”
Along with the new instruments and the ‘wet technique’, superficial liposuction and ways to improve and facilitate liposuction were developed as well.
Ultrasound assisted liposuction (UAL) was first introduced by Kloehn [22] and popularised even more in the late 1990s when Zocchi introduced perforated cannulas [22,23]. Ultrasound is the process which turns electricity into mechanical vibrations and results in both thermal effects and mechanical effects to the surrounding adipocytes.
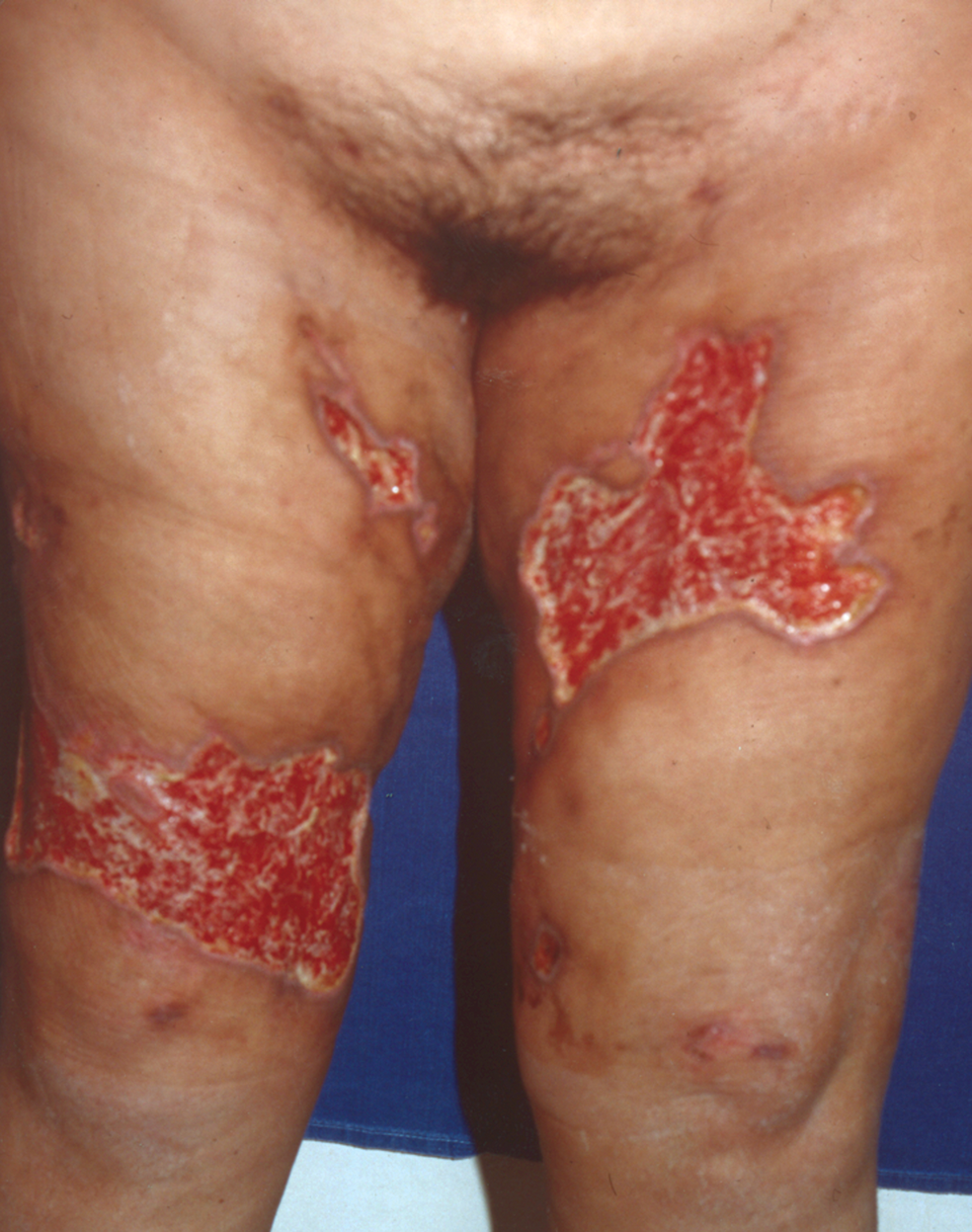
These mechanical oscillations pass through the cannula that emits the waves from its tip [24-26]. The thermal effects play a role in fat dissolution and must be dissipated by tissue infiltration [27]. Graf et al. conducted a study of 348 patients who underwent UAL in Brazil. The use of UAL leads to preservation of vessels and better haemostasis [28]. Factors that may discourage the use of UAL are the thermal effects on the skin and nerves, with huge burns leading to unacceptable results [Figure 7]. These catastrophic complications made this technique obsolete but some are now using a ‘cold’ ultrasonic technique called ‘vaser’.
Figure 7: Huge burns after a UAL liposuction.
Laser assisted liposuction
The laser beam is directly propagated to adipose tissue with which it keeps direct contact. The action of the laser causes the rupture of the adipocyte membrane and consequent release of oily content into the extracellular fluid. In addition, coagulation of collagen is found and microtunnels are created in the track of the laser beam, along with coagulation of microvessels in the adipose tissue. Complications and final results of laser-assisted liposuction are similar to those obtained with the majority of liposuction techniques. In addition to the cytolitic effects on adipocytes, the laser can induce remodelling of the collagen and reorganisation of the reticular dermis. It is particularly indicated as an office-based procedure for localised areas of lipodystrophy in the body or face. The interaction between laser and adipose tissue was initially described by Apfelberg [29] and Apfelberg et al. [30,31] in 1992. Low-level laser therapy externally applied through skin and preceding liposuction has also been proposed as a method to cause fat liquefaction before aspiration, but the utility of this treatment was subsequently disproved. [32-41]
Complications
Ecchymosis is inherent in liposuction and varies according to the individual patient, the volume of the treated area, and the extent of the treatment. Oedema usually subsides within several weeks, but in distal areas, such as the calf or ankle, it may persist from six months to a year. Induration will subside in a similar fashion. Hyperesthesia or dysesthesia are common sequelae of the procedure, which will gradually improve in three to six months after surgery. A minor degree of irregularity in the overlying skin also improves within a period of months.
Localised infections are not frequent after lipoaspiration, but can sometimes occur, especially in the case of early return to normal activities. Local infections are easily treated, whereas toxic shock syndrome, a systemic disease caused by the toxin of Staphylococcus aureus, is a life-threatening event. It presents with fever, diarrhoea, nausea and vomiting, and can be associated with a specific rash and oliguria. This syndrome can even progress to necrotising fascitis, requiring urgent debridement and intensive care.
Further complications include contour defects, permanent skin colour changes, infection, emboli, haematomas or seromas, but mainly sequelae induced by an insufficient or too aggressive technique (Figure 8).
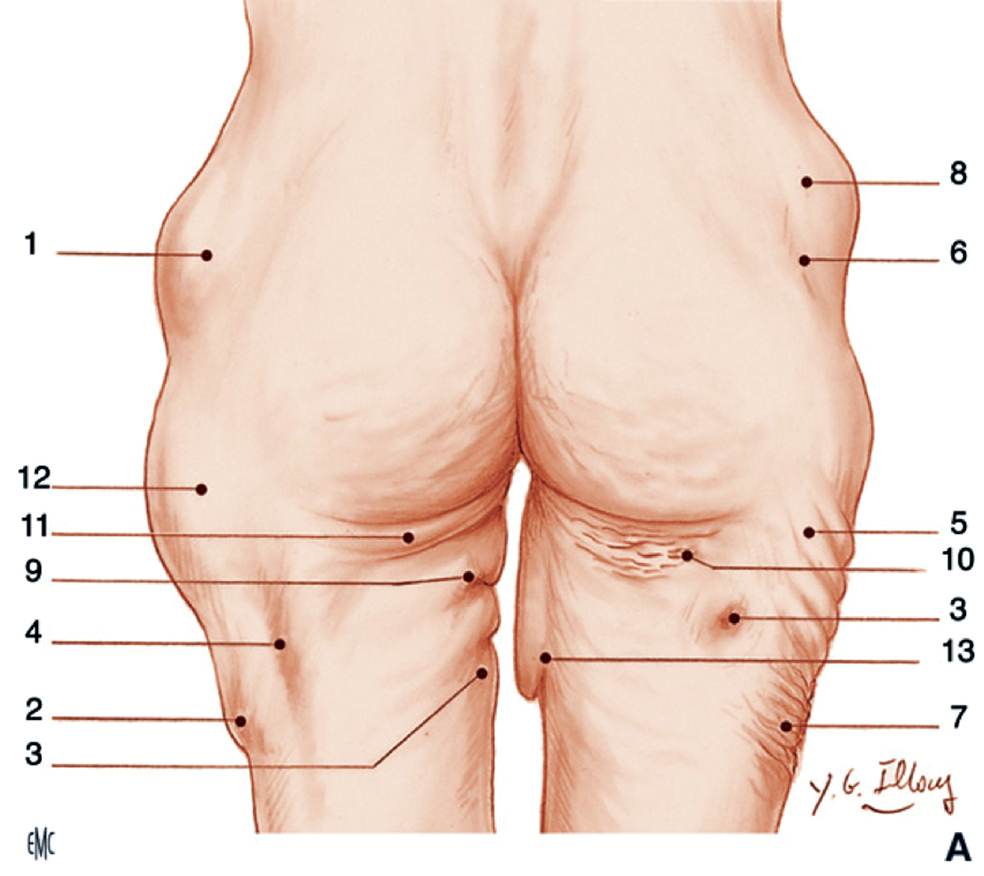
Figure 8: All types of possible sequelae: 1 & 8) Residual bumps; 2) Step deformity; 3 & 4) Grooves;
5) Waviness; 6) Depression; 7) Wrinkles; 9) Internal waviness; 10) Bunch of little bananas;
11) Postoperative banana; 12) Insufficient suction; 13) Ptosis.
Major complications, with a lethal effect, are reported in 1:5000 cases from plastic surgeons according to Grazer and De Jong [42] in 2000. Higher rates are described when liposuction is performed by doctors without specialist training in plastic surgery. The most frequent cause of death was deep venous thrombosis (DVT) associated with pulmonary embolism (23.1%). Abdominal and bowel perforations are reported as the second commonest lethal event (14.6%). In 10% of cases the death was caused by the use of local anaesthesia, sedation and other medications. This last percentage is probably underestimated because in some cases the death occurred after discharge from hospital, due to the late peak concentration of lidocaine. Bleeding, formerly the most relevant cause of death due to lipoaspiration, represents just 4.6% of lethal events according to this study, which was conducted after the introduction of the tumescent and superwet techniques of infiltration.
With the new methods of injections, the new identified risk factors are office-based or multiple procedures, excessive infiltration and intoxication from lidocaine or adrenaline (usually with some hour-delayed onset), excessive removal of adipose tissue with volume depletion in the third space, postoperative respiratory depression, early discharge. The risk of DVT is associated with blood flow stasis, trauma and possible hypercoagulation status. Intermittent compression devices for legs, early mobilisation and the use of low molecular weight heparins can reduce the risk. The event of perforation is extremely rare, but represents a severe complication.
All these ‘surgical’ complications are now exceptional because the technique is better understood and performed by qualified surgeons.
References
1. Flynn TC, Coleman WP 2nd, Field LM, et al. History of liposuction. Dermatol Surg 2000;26:515-20.
2. Kesselring U. Regional fat aspiration for body contouring. Plast Reconstr Surg 1983;72:610-19.
3. Hetter G (Ed.). Lipoplasty: the Theory and Practice of Blunt Suction Lipectomy. Boston,USA; Little, Brown & Co; 1984.
4. Illouz YG. Body contouring by lipolysis: a 5-year experience with over 3000 cases. Plast Reconstr Surg 1983;72:591-7.
5. Newman J. Lipo-suction surgery: Past-present-future. Am J Cosmet Surg 1984;1:19-20.
6. Illouz Y. Remodelage de la silhouette par lipolyseaspiration ou lipectomie selective. Ann Chir Plast Esthet 1984;29:162-79.
7. Illouz YG. Refinements in the lipoplasty technique. Clin Plast Surg 1989;16:217-33.
8. Khan MH, Victor F, Rao B, Sadick NS. Treatment of cellulite: Part II. Advances and controversies. J Am Acad Dermatol 2010;62(3):373-84; quiz 385-76.
9. Lllouz YG. History and current concepts of lipoplasty. Clin Plast Surg 1996;23:721-30.
10. Hetter GP. The effect of low-dose epinephrine on the hematocrit drop following lipolysis. Aesthetic Plast Surg 1984;8:19-21.
11. Triana L, Triana C, Barbato C, Zambrano M. Liposuction: 25 years of experience in 26,259 patients using different devices. Aesthet Surg J 2009;29:509-12.
12. Illouz YG. Une novelle technique pour les lipodystrophies localisees. Rev Chir Esthet Langue Franc 1980;19:3-10.
13. Toledo LS. ‘Syringe liposculpture for face and body’. In: Annals of the International Symposium ‘Recent Advances in Plastic Surgery’. Sao Paulo, Brazil, Estadao, 3-5 March, 1989.
14. Toledo LS. Syringe liposculpture. Clin Plast Surg 1996;23:683-93.
15. Lewis CM. Comparison of the syringe and pump aspiration methods of lipoplasty. Aesth Plast Surg 1991;15:203-8.
16. Illouz Y. Body sculpturing by lipoplasty. London, UK; Churchill Livingstone; 1988.
17. Elbaz JS. Esthetic abdominoplasty with preliminary liposuction. Ann Chir Plast Esthet 1987;32:148-51.
18. Matarasso A. Liposuction as an adjunct to a full abdominoplasty. Plast Reconstr Surg 1995;95:829-36.
19. Matarasso A. Abdominolipoplasty: a system of classification and treatment for combined abdominoplasty and suction-assisted lipectomy. Aesthetic Plast Surg 1991;15:111-21.
20. Ousterhout DK. Combined suction-assisted lipectomy, surgical lipectomy, and surgical abdominoplasty. Ann Plast Surg 1990;24:126-32; discussion 132-3.
21. Illouz YG. En bloc abdominoplasty: a new, safer and more esthetic technique. Ann Chir Plast Esthet 1990;35:233-42.
22. Kloehn R. Liposuction with “Sonic Sculpture”: six years’ experience with more than 600 patients. Aesthet Surg J 1996;16:123-8.
23. Zocchi ML. Basic physics for ultrasound-assisted lipoplasty. Clin Plast Surg 1999;26:209-20.
24. Igra H, Satur NM. Tumescent liposuction versus internal ultrasonic-assisted tumescent liposuction. A side-to-side comparison. Dermatol Surg 1997;23:1213-18.
25. Lawrence N, Cox SE. The efficacy of external ultrasound-assisted liposuction: a randomized controlled trial. Dermatol Surg 2000;26:329-32.
26. Thornton LK, Nahai F. Equipment and instrumentation for ultrasound-assisted lipoplasty. Clin Plast Surg 1999;26:299-304.
27. Zocchi ML. Ultrasonic assisted lipoplasty. Technical refinements and clinical evaluations. Clin Plast Surg 1996;23:575-98.
28. Graf R, Auersvald A, Damasio RC, et al. Ultrasound-assisted liposuction: an analysis of 348 cases. Aesthetic Plast Surg 2003;27:146-53.
29. Apfelberg D. Laser-assisted liposuction may benefit surgeons and patients. Clin Laser Mon 1992;10:259-64.
30. Apfelberg D, Rosenthal S, Hunstad J. Progress report on multicenter study of laser-assisted liposuction. Aesth Plast Surg 1994;18:259-64.
31. Apfelberg D, et al. Results of multicentric study of laser-assisted liposuction. Clin Plast Surg 1996;23:713-19.
32. Blugerman G. Laserlipolysis for the treatment of localized adiposity and “cellulite”. Abstr World Congress Liposuction Surgery; Dearborn, MI, USA; 2000.
33. Schavelzon D, Blugerman G, Goldman A. Laser lipolysis. Abstracts of the 10th International Symposium on Cosmetic Laser Surgery; Las Vegas, USA; 27-29 April, 2001.
34. Goldman A, Schavelzon D, Blugerman G. Laser lipolysis: liposuction using ND:YAG laser. Rev Soc Brasil Cirugia Plast 2002;17:17-26.
35. Goldman A, Schavelzon D, Blugerman G. Laserlipolysis-Liposuction with Nd:YAG laser. Translation of Laserlipolise-lipoaspiracao com Nd:YAG laser. Rev Soc Bra Laser 2003;2:1-3.
36. Goldman A. Lipoaspiracao a laser-laserlipolise no contorno corporal. Rev Brasil Cirugia 2002;3:92-3.
37. Badin A, Moraes L, Gondek L, et al. Laser lipolysis: flaccidity under control. Aesth Plast Surg 2002;26:335-9.
38. Neira R, Arroyave J, Ramirez H, et al. Effect of low-level laser therapy on abdominal adipocytes before lipoplasty procedures. Plast Reconstr Surg 2002;110:912-22.
39. Brow S, Rohrich R, Kenkel J, et al. Effect of low-level laser therapy on abdominal adipocytes before lipoplasty procedures. Plast Reconstr Surg 2004;113:1796-804.
40. Ichikawa K, Miyasaca M, Tanaka R, et al. Histologic evaluation of the pulsed Nd:YAG laser for laser lipolysis. Laser Surg Med 2005;36:43-6.
41. Kim KH, Geronemus RG. Nonablative Laser And Light Therapies For Skin Rejuvenation. Arch Facial Plast Surg 2004;6:398-409.
42. Grazer FM, De Jong RH. Fatal outcomes from liposuction: census survey of cosmetic surgeons. Plast Reconstr Surg 2000;105:436-47.
Declaration of competing interests: None declared.