Laser hair removal is a popular, and constantly evolving, treatment. Professor Paolo Bonan and colleagues provide us with a comprehensive overview and some ‘top tips’ for how to make the procedure as safe and effective as possible.
Hair removal, also known as epilation, is the deliberate removal of body hairs. Forms of hair removal have been practised in almost all human cultures since at least the Neolithic era, for various cultural, sexual, medical or religious reasons. Methods used to remove hairs have varied in different times and regions, including bleaching, plucking, shaving, waxing, threading, chemical depilatories (eflornithine) and electrolysis; these methods can no longer be considered ideal tools because of the limited and the short-term efficacy.
There has, therefore, developed a great demand for efficient long-term hair removal systems; in fact, photoepilation by light and laser-based systems is one of the fastest growing areas of cosmetic dermatology.
Only a few patients require hair removal for a purely medical purpose (these include patients affected by hirsutism, hypertrichosis, acne cheloidalis nucae, pseudofolliculitis barbae), while most undergo these procedures for purely aesthetic reasons, mainly for the removal of unwanted hair from the face, trunk, limbs and genital area.
If patients are affected by medical troubles, they are highly motivated and generally willing to undergo long and painful procedures; when the approach is purely aesthetic, discomfort levels and the session’s duration can be important factors for the choice of the device and the pathway of treatments.
In particular, the genital zone is one of the most commonly treated body areas; the so-called ‘Brazilian look’, which involves complete removal of hairs from the vulva, perineum, anus, and buttocks, is a particularly popular current trend. Hair removal in these sensitive areas may be very painful with wax or other traditional devices, so the employment of a laser or light-based technology is often preferred.
Lasers and light based hair removal: how they work
Several laser and light devices are available on the market for hair removal: ruby laser (694nm), Alexandrite laser (755nm), diode laser (800nm), intense pulsed light (IPL) (590-1200nm), neodymium-doped:yttrium aluminium garnet laser (Nd:YAG) (1064nm) and light-based devices for home use.
The purpose of these devices is the damage of stem cells in the bulge and dermal papilla of the hair follicle by targeting melanin which represents the specific chromophore [1-3]. Melanin absorbs wavelengths between 600-1100nm, the recommended optical window for hair removal with the destruction of the follicular unit.
For such devices, three main mechanisms of action have been suggested: photothermal destruction, photomechanical damage and photochemical process.
Photothermal destruction of hair follicles constitutes the fundamental concept of hair removal: melanin, the chromophore contained inside the hair shaft, absorbs the light energy converting it into heat, which spreads to the nearby bulge non-pigmented stem cells, the target. The transfer of heat from the chromophore to the target is necessary for the effectiveness of the treatment. Recently it has been demonstrated that the anagen phase is sensitive to laser and light pulses exactly as in the catagen and the telogen since in humans the hairs remain pigmented during the whole hair cycle. For this reason, targeting the hair follicles during a specific growth period, is considered to be unimportant. The previous theory about the greater sensitivity of the anagen period was due to animal studies which showed a maximum concentration of melanin within anagen hairs [2-5]. Photomechanical destruction, through the generation of shockwaves, has been used by nanosecond Q-switched lasers, employed during the early phase of laser hair removal several years ago; these lasers are no longer considered because they result in temporary hair loss.
“During the treatment, the laser / light emission should always be matched with a cooling system”
Photochemical destruction, through the creation of toxic mediators such as singlet oxygen or other free radicals, is the approach followed by photodynamic therapy (PDT); this could be a potential alternative technology since it may also work on non-pigmented hairs.
Lasers and lights
IPL
IPL technology uses a xenon broadband flashlamp to generate non-coherent light in a spectrum between visible and near infrared (500-1200nm). To reach the desired chromophore, filters cut out the light emission according to the wavelengths required by the physician; consequently, this type of light source can excite more than one chromophore (haemoglobin, melanin, water). Handpieces have a large surface of the spot, which is generally cooled, and application of gel on the skin surface is required during epilation. Clinical endpoints, frequently seen during epilation by lasers, are not commonly observed with IPL. Various studies have shown that IPL is inferior to Alexandrite and Nd:YAG lasers for long-term results [6-14].
Nd:YAG
Nd-YAG long pulse is a laser source with a longer wavelength and represents the first choice in darker skin patients in our experience. According to several comparative studies Nd:YAG laser has been found to be less effective than Alexandrite and diode lasers, and more efficacious than IPL and ruby laser as regards long-lasting hair removal results [6-14].
Diode laser
Histological studies showed significant reduction in hair density and thickness in skin treated with longer pulse 810nm diode laser. The long pulsed diode has been greatly used for hair removal due to the efficacy and safety in patients with Fitzpatrick skin phototypes I-V. Such lasers are usually employed through an in-motion manner, with several short pulses and a high frequency. Patients often consider this laser more tolerable than the long pulsed Nd:YAG [6-14].
Alexandrite laser
Since 1997 the long pulse 755nm Alexandrite laser has been utilised with efficacy in laser hair removal. It allows a deep penetration into the dermis allowing it to act on fair and black hair, however, because of its competition with melanin it is particularly indicated in patients with low phototypes (up to 3-4) for the risk of burning resulting in hyper or hypo pigmentation. In order to remedy this problem a new technology for photoepilation has recently been proposed. A new handpiece, with a cooled sapphire cylinder tip that conveys the laser beam onto the patient’s skin, has been introduced onto the market. The use of this sapphire guide dramatically reduces the system energy leaks to the skin, thus increasing effectiveness of the laser transmission as never before (Figure 1). Working at low fluences makes the treatment painless without undesirable side-effects. Repeated passages over the same area makes the treatment uniform without leaving any area untreated.
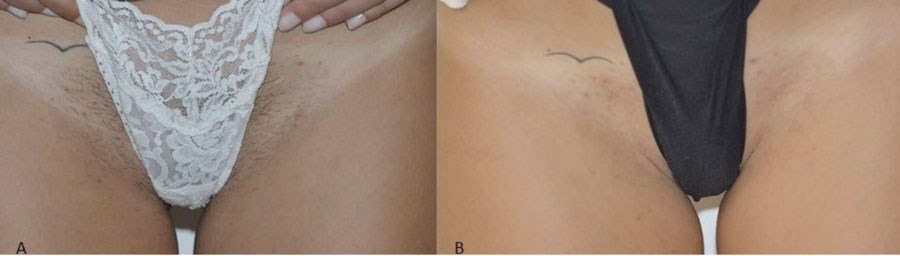
Figure 1A: Before starting laser hair removal on the inguinal areas. 1B:
The results achieved after two Alexandrite laser sessions
(Motus AX, Deka M.E.L.A. laser, Elen, Italy).
Ruby laser
This was the first laser device selectively employed for hair removal, by Grossman in 1996 [15]. Compared to newer laser and light-based modalities, the ruby laser is less effective and in fact there are no long pulsed ruby lasers commercially available in the American market. Side-effects, like hypopigmentation, have been reported after its use on dark skin.
Home devices
Home devices are characterised by lower fluence compared with medical devices; this feature limits their effectiveness, since there is evidence of the capability of hair removal systems being fluence-dependent. Conversely, the risks of adverse effects are reduced too. Nevertheless, the general public often prefer investing their money into these tools because they are cheap and pain free.
Clinical features of the patient
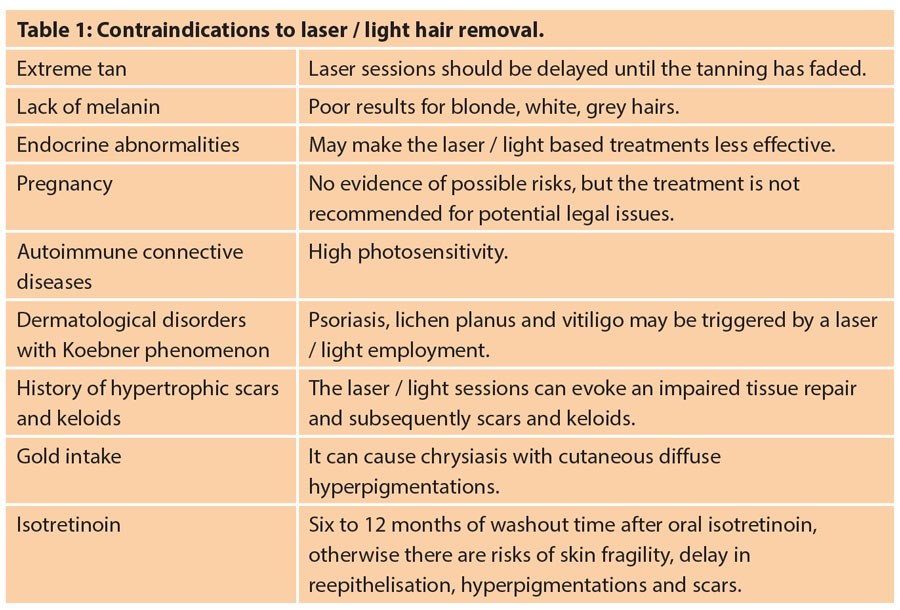
The main features to be evaluated are skin phototype and hair. Shorter wavelengths are more absorbed by melanin, so for high phototypes lasers with a low wavelength will result in a greater risk of burning and consequently other unpleasant side-effects; for these patients the selection of a diode laser or Nd:YAG laser is mandatory. If the physician has a limited choice of laser systems, it is possible to use a lower fluence, a longer pulse duration and a specific filter to make the treatment safer. Sometimes, for various reasons, patients cannot be treated with lasers or IPL devices (Table 1).
Preparation for the treatment
It is necessary to remind the patient to avoid all epilation techniques for two to four weeks before the laser / light hair removal, otherwise it will provoke elimination of the structure target of the photoepilation. Shaving the hair by the physician immediately before the beginning of the treatment, or two to three days earlier by the patient, is adequate. If the laser / light hair removal is not preceded by shaving, the pulses absorbed by the long hairs could induce burning of the skin. We usually prefer to do the shaving ourselves, since we can better evaluate the diameter and the pigmentation of the hairs cut, and these features affect the parameters to be chosen.
Selection of the parameters
The fluence (J/cm2) determines the temperature achieved within the follicular stem cells in the bulge while the pulse duration corresponds to the time length of that reached temperature. The energy level, the fluence, changes for each laser and IPL device according to their output range features, however, the physician should select the highest value without eliciting side-effects in the skin, since high fluences are correlated with greater permanent hair removal. Normally, the fluence is inversely proportional to the pigmentation of the hairs to be removed, e.g. darker hairs require lower fluence while brighter hairs need higher fluence.
“Cryogen spray, cold air, and direct contact cooling are commonly employed in combination with lasers and IPL [19]”
According to the selective phothermolysis theory the pulse duration should approximately correspond to the thermal relaxation time (TRT) of the chromophore, but for laser-based hair removal the chromophore, melanin, and the laser biological target, stem cells of the follicle bulge, do not correspond. This requires a laser pulse duration longer than if the chromophore and the target were identical; we apply the concept of thermal damage time (TDT), allowing the conduction of thermal damage to the follicular stem cells. As a result, 10-100ms laser or IPL pulses are usually needed, while shorter pulse times are indicated for thinner hairs. In the cases of dark phototypes the pulse duration should increase for achieving a sort of epidermal protection to all the possible risks.
The patient with a high phototype with thin and bright hairs presents a serious challenge for hair removal practitioners, as this type of hair would require a great fluence and a short pulse whereas the skin type would require a low fluence and a long pulse duration.
Another relevant fact to be considered is the progressive reduction of the hair diameter with the laser / light sessions, so the physician may need to change the parameters being used.
The spot size influences the penetration depth of light, since a bigger spot size penetrates deeper for a reduced scattering phenomenon. A larger spot size allows the practitioner to cover the area to be epilated rapidly, but this can lead to increased discomfort for the patient due to the possible unpleasant sensation on a larger part of the body [16-18].
Treatment protocol
During the treatment, the laser / light emission should always be matched with a cooling system; this is important for all phototypes, but vital in those persons with more epidermal melanin. Cryogen spray, cold air, and direct contact cooling are commonly employed in combination with lasers and IPL [19].
Clinical endpoints
Clinical therapeutic endpoints are immediate or early cutaneous reactions that take place during a laser session; they may guide the physician in delivering safe and effective laser / light treatment. The most relevant clinical endpoint for laser and IPL hair removal is perifollicular erythema and oedema, which corresponds to an eosinophilic inflammatory reaction due to the hair injury. This endpoint typically appears a few minutes after the laser / IPL passage and this immediate skin response gives evidence of the effectiveness of the treatment.
The pigmented hairs vaporise releasing a typical smell of smoke due to the burnt keratin. The thin hairs behave in a different manner after the laser / light emission: they can enlarge the tip or turn white at the follicular ostium.
Results
A permanent dropout of hair follicles is reached in 15-30% of laser / light treated hairs at each session, while the majority of treated hairs fall into a telogen-like state characterised by rest and absence of hair growth. This telogen-like state explains a short-lasting period of alopecia, usually lasting for a few months, until some hair follicles begin another anagen cycle.
Erythema frequently occurs and the employment of a topical steroid for two to three days is enough to eliminate this temporary side-effect. The patient must always remember to avoid sun exposure and to apply sunscreen for several days days following the session.
Possible side-effects
The most common cutaneous reactions include erythema, oedema, discomfort, pain, and occasionally more severe side-effects, such as thermal burns, blisters, hyperpigmentation, hypopigmentation and scarring, can occur. Severe side-effects manifest more frequently in darker-skinned patients but can be avoided or minimised by the selection of safer parameters and an effective cooling process during the session. ‘Paradoxical hypertrichosis’ is a rare side-effect observed in patients treated by IPL, diode and Alexandrite lasers, when the laser or light stimulates the growth of new hairs through a photoactivation of dormant hair follicles into terminal anagen hair phase. It is characterised by the appearance of new hair follicles surrounding the treated areas. This side-effect could be induced by the selection of excessively conservative parameters, and therefore it can be solved by more aggressive parameters during the subsequent sessions [20-21].
“Severe side-effects manifest more frequently in darker-skinned patients but can be avoided or minimised by the selection of safer parameters and an effective cooling process during the session.“
Conclusion
Laser hair removal is a popular treatment, and therefore its techniques are evolving. According to previous comparative studies laser and light-based systems for hair removal are shown to be generally safe and efficacious if employed by experienced practitioners. The differences between these systems include the time length of every session, the discomfort felt by the patient, the possibility of treating darker patients, and the cost of a single treatment. New hair removal systems could include promising portable home devices, photopneumatic technologies, PDT and bipolar radiofrequency. Clinical studies and long-term data will be necessary to determine the effectiveness and the safety of these modalities from the future.
References
1. Choudhary S, Elsaie ML, Nouri K. Laser assisted hair removal. G Ital Dermatol Venereol 2009;114:595-602.
2. Kolinko VG, Littler CM, Cole A. Influence on anagen:telogen ratio on Q switched Nd:YAG laser hair removal efficacy. Laser Surg Med 2000;26:33-40.
3. Seago SV, Ebling FJ. The hair cycle in human thigh and upper arm. Br J Dermatol 1985;113:9-16.
4. Randal VA, Ebling FJ. Seasonal changes in human hair growth. Br J Dermatol 1991;124:146-51.
5. Hughes CL. ‘Hirsutism’ In: Olsen EA (Ed). Disorders of hair growth: diagnosis and treatment. New York, USA: McGraw Hill; 1994:337-50.
6. Gan SD, Graber EM. Laser hair removal: a review. Dermatol Surg 2013;39:823-38.
7. Haedersal M, Haak CS. Hair removal. Curr Probl Dermatol 2011;42:111-21.
8. Kutlubay Z. Alexandrite laser hair removal results in 2359 patients: a Turkish experience. J Cosmet Laser Ther 2009;11:85-93.
9. Khoury JG, Saluja R, Goldman MP. Comparative evaluation of long-pulse Alexandrite and long-pulse Nd:Yag laser systems used individually and in combination for axillary hair removal. Dermatol Surg 2008;34:665-70.
10. Cannarozzo G, Bonan P, Campolmi P. Epilation with Nd:YAG laser: a brief analysis of the technical application methods, result and pre- and post- treatment procedures. J Cosmetic Laser Ther 2003;5:189-91.
11. Ismail SA. Long-pulsed Nd:YAG laser vs. Intense Pulsed Light for hair removal in dark skin: a randomized controlled trial. Br J Dermatol 2012;166:317-21.
12. Baugh WP, Trafeli JP, Barnette DJ Jr, Ross EV. Hair reduction using a scanning 800nm diode laser. Dermatol Surg 2001;27:358-64.
13. Finkel B, Eliezri YD, Waldman A, Slatkine M. Pulsed Alexandrite laser technology for noninvasive hair removal. J Clinic Laser Med Surg 1997;15:225-9.
14. Faurschou A, Haedersdal M. ‘Photoepilation of unwanted hair growth’ in: Raulin C, Karsai S (Eds). Laser and IPL technology in dermatology and aesthetic medicine. Berlin, Germany: Springer-Verlag; 2011:125-46.
15. Grossman MC, Dierickx C, Farinelli W, et al. Damage to hair follicles by normal-mode ruby laser pulses. J Am Acad Dermatol 1996;35:889.
16. Ibrahimi OA, Avram MM, Hanke CW, et al. Laser hair removal. Dermatol Ther 2011;24:94-107.
17. Serrano-Grau P, Campo-Voegeli A, Romero D. Fotoepilacion. Actas Dermosifiliogr 2009;100:351-61.
18. Haedersdal M, Beerwerth F, Nash JF. Laser and intense pulsed light hair removal technologies: from professional to home use. Br J Dermatol 2011;165:31-6.
19. Ram R, Rosenbach A. Effects of ambient room temperature on cold air cooling during laser hair removal. J Cosmet Dermatol 2007;6:203-6.
20. Rasheed AI. Uncommonly reported side effects of hair removal by long pulsed Alexandrite laser. J Cosmet Dermatol 2009;8:267-74.
21. Alajlan A, Shapiro J, Rivers JK, et al. Paradoxical hypertrichosis after laser epilation. J Am Acad Dermatol 2005;53:85-8.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME




