The medical school curriculum is increasingly focusing on the role of a general practitioner, which has resulted in medical students having reduced exposure to surgical specialties. There has been a longstanding concern that plastic surgery teaching and exposure in the medical school curriculum is on a decline over the past few decades [1-5,8]. It is known that future career choices are influenced by the medical school curriculum. In addition, medical students and young trainees misunderstand the range of diseases and procedures performed by plastic surgeons and commonly misconceive their work to be predominantly cosmetic.
This is further compounded by the lack of placements at medical school in this specialty, which may potentially have an impact on the future of the specialty [1,4]. Research has shown that preconceived ideas and positive exposure to a specialty, the length of experience and the presence of role models or mentors influences the choice of career made [3,6-13]. However, due the limited involvement of plastic surgeons in the medical school curriculum, role models are not available during the crucial periods when students are making career choices or seeking advice [8].
Research in the United States has shown that undergraduate exposure introduced before the third year of medical school is the strongest factor in attracting applicants to plastic surgery [3]. Interestingly, the competition for a plastic surgery training post remains high at seven applicants to one vacancy, which is comparatively higher than other specialties such as urology, 1.4:1, and cardiothoracic surgery, 0.45:1. It has been shown that most plastic surgeons chose to pursue this specialty during postgraduate training, however in modern times, due to the structure of training programmes introduced by Modernising Medical Careers and the introduction of the European Working Time Directive, this career choice is made earlier than ever before with relatively little clinical experience [1-5].
Plastic surgery is not confined to age, pathology or anatomy, which makes it unique compared to other surgical specialties. It is well known that career decisions can be changed several times throughout a student’s time at medical school and early stages of training and early clinical exposure can aid this process [11].
Swansea University is unique in offering early clinical exposure to plastic surgery and formal teaching within the curriculum that is delivered by local plastic surgeons. Therefore, a cross-sectional survey was performed to investigate the influence of this early clinical exposure and teaching and to determine the factors medical students felt were most influential in considering a career in plastic surgery with a view to addressing the growing concern of marginalisation of plastic surgery from undergraduate training [2-4].
Objectives
The aims of this study were to assess:
- The influence of early plastic surgery exposure and teaching in the medical school curriculum.
- Factors that influence medical students to pursue a career in plastic surgery.
- Medical student perception of plastic surgery and the role of extracurricular activities and external influences, such as the media.
This review would serve to enrich and update the debate surrounding whether teaching and exposure to plastic surgery must increase at an undergraduate and early postgraduate level.
Setting
Swansea University runs a four-year, fast tracked, Graduate Entry Medical Programme. It is unique in offering early clinical exposure to first and second year students via an innovative system of Learning Opportunities in the Clinical Setting (LOCS) [6]. Students must complete a minimum of 10 LOCS and can choose from 31 different specialties, including plastic surgery. Each LOCS lasts half a day and it is compulsory to complete at least one in surgery. LOCS encourage experiential learning, early clinical exposure to self selected specialties and learning opportunities that may be excluded from a standard curriculum, which can assist in making future career choices. Some students are randomly allocated to a five-week plastic surgery placement in year one or two. This approach is supported by evidence that early clinical exposure improves students’ understanding of a specialty, increases clinical confidence, allows accelerated personal development and improved academic and career progression [6,11].
Methods
The purpose of this study was to determine medical student career choices and factors centered around choosing plastic surgery as a future career. Therefore, a cross sectional survey was carried out in December 2013, which is the end of the first academic term. Institutional ethic committee approval was sought and a preliminary survey was conducted via a focus group of 10 medical students and one plastic surgery consultant and registrar, respectively, to ascertain appropriate questions and practical conditions and minimise extraneous variables.
A paper copy of the survey was handed out via a current third year medical student to all medical students attending Swansea University Medical School. Information regarding medical students was obtained from the medical school’s curriculum staff. Incentives for completing the survey were not offered and neither were non-responders followed up. Survey responses were collected on the same day via an easily accessible designated drop-in box and multiple submissions were prevented by assigning each student and survey a unique identification number. Students were advised that this study was being carried out by the local plastic surgery team at Morriston Hospital, Swansea, Wales. The exact aim of the study was only elucidated upon completion of the survey to avoid biasing the results. A cover sheet served as a waiver of documentation of informed consent [14]. All students were informed that all data would be anonymous and kept confidential. They were also reassured that there was not a right answer to any of the questions.
The data was extracted into a spreadsheet and analysed using a grounded theory approach to identify any themes to the answers given [6]. Data from incomplete surveys was included whenever possible.
The survey was designed to be as personally non-intrusive as possible and centered around previously published work examining a similar topic [14].
The survey involved 52 questions and investigated the following categories:
- Student profiling: year of study, age, gender and ethnic origin [14-21].
- Career aspirations: preference for a particular specialty, when this choice was made, factors influencing this choice, whether being a graduate medical student influenced this.
- Teaching and clinical exposure: the quality of anatomy teaching, participation in any surgical skills, teaching from plastic surgeons, plastic surgery elective, special study module or project in plastic surgery, the availability of plastic surgery placements, the influence of a plastic surgery placement and pursuing this as a specialty, plastic surgery LOCS.
- Extracurricular activities: any extracurricular interests in plastic surgery, member of the medical school’s surgical society, any plastic surgery components offered by the surgical society, attended any plastic surgery conferences.
- Perception of plastic surgery: the influence of exposure to plastic surgeons, a role model or mentor in plastic surgery, the role of a plastic surgeon, the influence of media and its effect on pursuing a career in plastic surgery, training pathway, competition ratio.
- Influencing factors (ranking scale): personality of plastic surgeons, gender distribution in the specialty, length of training, lifestyle during training, lifestyle after training, work hours during training, work hours after training, ability to obtain a training number, patient interaction, future patient demographics, income potential, prestige, intellectual challenge, television programme exposure, concern about debts, on call schedule, pressure from family, pressure from peers, research possibilities.
The first five categories consisted of open-ended questions and the last category involved ranking the importance of 19 characteristics or factors that might influence the student’s decision to apply for plastic surgery training. The ranking was based on a scale of 0 to 7 with 0 bearing no influence and 7 being very influential.
Results
1) Student profiling
A total of 153 British medical students (53% combined response rate) from all four years at Swansea University completed our survey. The overall mean age of students was 25-years-old and 45% of respondents were male and 55% female. The individual response rate was 65%, 51%, 51% and 47% for year one, two, three and four, respectively.
2) Career aspirations
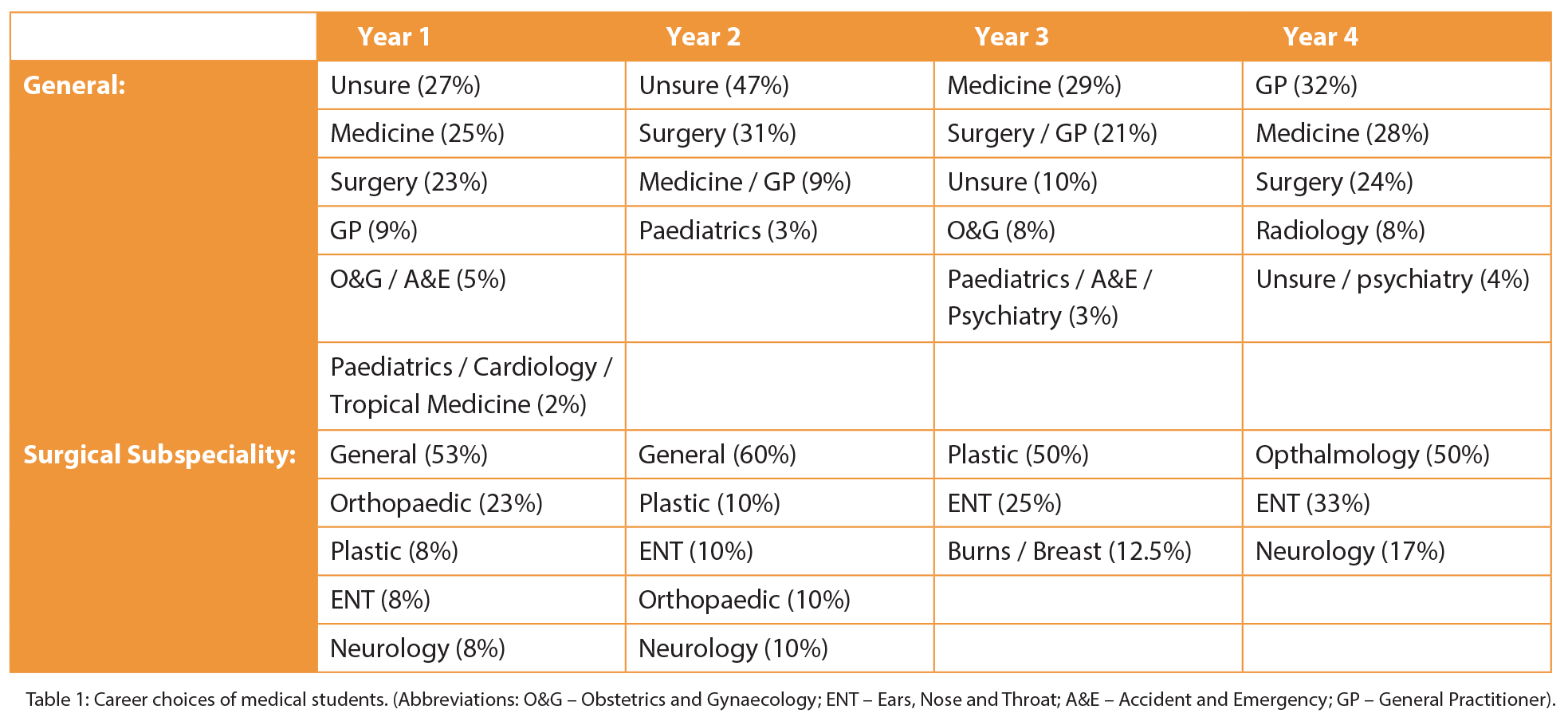
(Table 1) Year one and two students largely reported making this career decision before starting medical school (68% and 54%) or in their first year (27% and 38%). The majority of year three students made this decision in the first (35%) or second year (28%). Finally, the majority of year four students decided in second (36%) and third year (32%). When asked what influenced their career choice, years one (53%), two (69%) and three (29%) reported “experience in the field” as being the main influencing factor, whereas year four students favoured a career offering a better lifestyle (33%). Being a graduate medical student was not considered to be a major factor, with all four years reporting this to be “not influential” (29%) or “slightly influential” (22%).
3) Teaching and clinical exposure
The majority of students (40%) reported anatomy teaching to be good, and a remarkable 82% of first year students reported being involved with surgical skills such as suturing. Least involvement in surgical skills activities was in year four (61%). The majority of students (92%) were aware that they had received formal teaching from a plastic surgeon very early on in the curriculum. Overall, the majority of students (82%) would not consider a plastic surgery elective. Year one students were most keen, with 45% of the respondents expressing an interest in a plastic surgery based elective, with the remainder having no interest, but by year four only three people were considering an elective in plastic surgery, two of whom had said they want to pursue a career in surgery, more specifically ENT, and the third student had chosen medicine as a career choice. Of all students, 87% were aware that plastic surgery LOCS exist. On average, in each year, four to five students had completed at least one plastic surgery LOCS. The most plastic surgery LOCS were completed by a second year student (six LOCS) and had expressed an interest in pursuing a career in plastic or breast surgery. All students who had completed a plastic surgery LOCS stated that they assisted in career making decisions and “gave a taster of the specialty.” The majority of fourth years (43%) felt placements only slightly influenced their career choice. First and second year students’ (28% and 33%) felt it was moderately influential. Third years mostly thought it was very influential (38%) and this coincides with it being the year with most plastic surgery LOCS completed and the highest interest in this specialty as a career.
4) Extracurricular activities
An average of four students from each year carry out extracurricular activities in plastic surgery, which range from reading around the subject to organising a LOCS. The majority of students (76%) were members of Swansea surgical society, which is student led. The least surgical society members were in year four (69%) and the most in second year (84%). All years knew (60%) that the surgical society offered plastic surgery exposure by way of surgeons coming in to talk or through organised surgical skill evenings, which introduced procedures performed by plastic surgeons, such as suturing, grafts, skin harvesting and vessel anastomosis. Interestingly, 60% of third year students had expressed an interest in specialising in plastic surgery. Of this group, 80% had also attended a plastic surgery conference.
5) Perception of plastic surgery
(Table 2) Year one and year three (41% and 45%) felt exposure to surgeons did affect career choice. Whereas the majority of year four (63%) believed exposure did not make any difference to career choice. One student in year one had a hand surgeon as her mentor and was interested in orthopaedics, Also, one student in year three had a plastic surgery mentor and was interested in this as a career. A year four student interested in ophthalmology and another in general surgery also had a mentor. Overwhelmingly, the majority of students felt the media projected plastic surgery in a negative light, year one (80%); year two (84%); year three (74%); year four (91%). Collectively, 12% (60% of them were year one) of the students stated that there was too much focus on breast surgery, cosmetic surgery and television shows tainted the profession and perception of plastic surgeons. However, the majority (88%) of all years said that the media influence would not affect their career choice. The majority of students were unaware of the plastic surgery training pathway, year one (90%), year two (86%), year four (81%), however only 50% were unaware in year three. When asked about the competition ratio of applicants applying to plastic surgery training, the majority of students were unaware (year one 90%, year two 60%, year three 57% and year four 72%) and 19% overall commented that it was very competitive, with 8% estimating the ratio to be 16-19:1 and 8% estimating it to be 5:1.
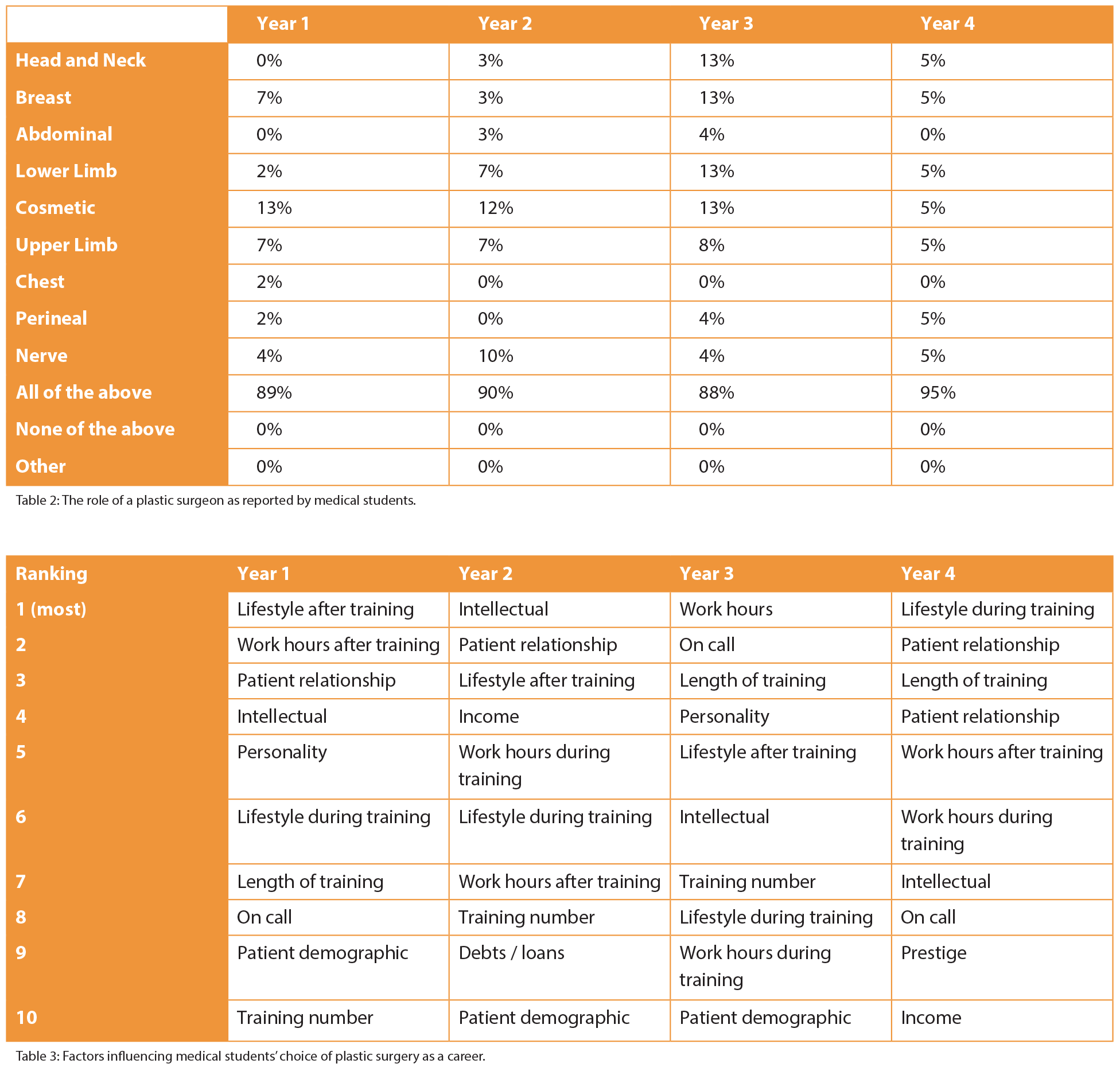
6) Influencing factors (Table 3)
Factors that would influence the students’ decision to apply for plastic surgery training are detailed in Table 3.
Discussion
Plastic surgery training is highly competitive when compared to other surgical specialties. Our study supports emerging evidence that the increased interest in plastic surgery is multifactorial, but early clinical exposure and interaction between plastic surgeons and students is the biggest predictor of a student selecting this as a career.
Encouragingly, the majority of students had become members of the university’s student led Surgical Society and reported that exposure to plastic surgeons does influence their career choice, which supports the role of mentors and early clinical contact. LOCS were implemented to allow for students to independently seek out clinical experience or extracurricular activities, but even the most eager student will face barriers, which was demonstrated by the low uptake of plastic surgery LOCS and few students with mentors. Furthermore, a currently unpublished study by the author, examining whether early surgical exposure via LOCS benefitted medical students found that it served a beneficial way of exploring career options, but negative feedback was also noted in three areas, 1) an obstructed view in theatre, 2) minimal teaching and 3) feeling unwelcome. Therefore, it is not a simple case of providing students with early clinical exposure to plastic surgery. Student uptake of clinical opportunities needs to be improved by ensuring consistent surgeon involvement, teaching and practical experience.
In addition, research has shown career choices are made as a result of positive exposure and preconceived ideas relating to a specialty [5,8-12]. This was supported by our study, which showed that junior students expressed more of a general interest in surgery, however with increased clinical exposure, the career choices of senior years were more specific towards a surgical subspecialty. This career decision was reported to be made largely in the first or second years of medical school, which was further supported by final year students stating that clinical placements were now only “slightly influential.” The findings of our study agree with previous research that plastic surgeon engagement should ideally occur before the third year of medical school [15]. Therefore, the need for early clinical exposure and a mentor is vital in shaping the future of surgery and has been found to correlate with future uptake of the specialty. Again, this was supported by our study, which found that the medical school year with students most interested in plastic surgery reported that this was due to “very influential” clinical placements. This is further supported by research demonstrating specialty choices are a ‘‘socially constructed process of trying on possible selves (i.e. projecting oneself into hypothetical career and personal roles) [14].’’
Despite the high level of plastic surgeon involvement throughout early years of the curriculum, students in this study were still unaware of the role of a plastic surgeon and focused on cosmetic and breast surgery. This may be influenced by media representation, as the majority of students, especially from year one, stated that plastic surgeons were portrayed negatively due to the main emphasis on cosmetic surgery and financial incentives. Encouragingly, the majority of students reported they would not allow the media to influence their career choice. Furthermore, in times of growing surgical subspecialisation, plastic surgeons should be encouraged to mentor medical students at an early stage and maintain this relationship, especially as the majority of students, even those that expressed an interest in plastic surgery, were unaware of the training pathway, but believed it to be a competitive process. This lack of knowledge, coupled with the fact it is seen to be competitive, may deter outstanding applicants from applying.
With regards to the future of plastic surgery, Calnan in 1970 stated that “undoubtedly the best way to encourage trainees to any specialty is to include, in the general undergraduate programme, lectures on the subject [18].” This has been heavily debated, with the general consensus being that the breadth of the subject, coupled with the interest it generated in students, would determine the inclusion of plastic surgery teaching in the medical school curriculum [9]. A single study has shown the majority of students to be interested in plastic surgery teaching and felt its absence would negatively impact the competency of, not just surgeons, but physicians and GPs too [7]. However, student interest and relevance may not always coincide, as previous research has shown that students perceive a subject’s importance based on what will be examined [6]. Plastic surgery is not confined to age, pathology or anatomy, which makes it unique compared to other surgical specialties and therefore, teaching can be tailored according to the needs of the curriculum and examination.
Research has found that students and doctors are increasingly placing greater emphasis on lifestyle and shorter training when choosing a specialty. This was supported by our survey, which showed a decline in response rate from the senior medical students and the shift from career choices being based on clinical experience in the junior years to favouring lifestyle and a career in general practice as a final year. Therefore, for plastic surgery to remain competitive as a specialty, strategies need to be employed to maintain a high level of interest in students, especially as it has been predicted that there will be a shortage of general surgeons by 2020 owing to the change in demographics of students, the increased emphasis on primary care in the undergraduate curriculum, unavailability of mentors, reduced early exposure to surgery and the demanding training. These findings can also help towards understanding how to advertise and recruit students to plastic surgery and allow surgical educators to recognise the changing demographics, needs and perceptions of current students.
Worryingly, the majority of students ranked research opportunities as being least influential in choosing a career in plastic surgery. Research is essential in improving surgical techniques, enriching the clinical evidence base and maintaining high quality care and standards in plastic surgery. A study found that an eight-week surgical programme in cardiothoracic surgery with a compulsory research project inspired students into this specialty and improved academic productivity throughout medical school with the help of an ongoing mentor. Therefore, early interventions at medical school, especially in the earlier years need to be employed to maintain or, better still, increase student interest in plastic surgery, such as extracurricular programmes, which allow mentor-led clinical and research experience.
It is encouraging to see that the majority of medical students who took part in this survey viewed their anatomy teaching as being “good.’’ It has been shown that anatomy taught by surgeons can increase student interest in surgery; therefore, plastic surgeons should be encouraged to participate. Previous studies have shown that even if the encounter between a surgeon and student is brief, providing it is positive, students can still be influenced towards a career in plastic surgery and it can improve the, sometimes negative, image of a plastic surgeon.
Conclusion
The results of this study support previous research [7,19-20] and encourage a continual review of the undergraduate and postgraduate teaching of plastic surgery to maintain the specialty’s high standards, minimise misrepresentation and attract outstanding candidates. Due to the inclusion of only one medical school in this study, national based conclusions cannot be drawn. We appreciate that financial and time constraints do not allow for all specialties to be taught by the medical school curriculum, however, specific extracurricular programmes can be developed to encourage the best medical students into plastic surgery.
Acknowledgement
The study was presented at the The Association for the Study of Medical Education (ASME) Scientific Meeting, July 2014.
References
1. Polk HC, Zeppa R. Elective programs in undergraduate surgical education: An early evaluation. Surgery 1968;64(1):295-301.
2. Berggren RB. Role of the plastic surgeon in undergraduate medical education. Plast Reconstr Surg 1972;50(1):75-6.
3. Prater MA, Smith DJ. Determining undergraduate curriculum content in plastic surgery. Plast Reconstr Surg 1989;84(3):529-33.
4. Rees-Lee JE, Lee S. Reaching our successors: the trend for early specialisation and the potential effect on recruitment to our speciality. J Plast Reconstr Aesthet Surg 2008;61(10):1135-8.
5. Ek WW, Ek ET, Mackay SD. Undergraduate experience of surgical teaching and its influence on career choice. ANZ J Surg 2005;75:713-8.
6. Burd A, Chiu T, McNaught C. Plastic surgery in the undergraduate curriculum: the importance of considering the students’ perception. Br J Plast Surg 2004;57:773-9.
7. Wade RG, Clarke EL, Leinster S, Figus A. Plastic surgery in the undergraduate curriculum: a nationwide survey of students, senior lecturers and consultant plastic surgeons in the UK. J Plast Reconstr Aesthet Surg 2013;66(6):878-80.
8. Dunkin CS, Pleat JM, Jones SA, Goodacre TE. Perception and reality - a study of public and professional perceptions of plastic surgery. Br J Plast Surg 2003;56:437-43.
9. Parikh AR, Clarke A, Butler PEM. Plastic surgery and the undergraduate medical school curriculum. Med educ 2006;40:476-7.
10. Wright V, Hopkins R, Burton KE. What shall we teach undergraduates? BMJ 1979;1(6166):805-7.
11. Chen H, Hardacre JM, Martin C, Lillemoe KD. Do medical school surgical rotations influence subspeciality choice? J Surg Res 2001;97:172-8.
12. Taylor I, Reed MF, Kingsworth AN, et al. Surgery in the undergraduate curriculum report by the educational and professional committee of SARS. Ann R Coll Surg Engl 2005; 87:139.
13. Cote L, Leclere H. How clinical teachers perceive the doctor-patient relationship and themselves as role models. Acad Med 2000;75:1117-24.
14. Burack JH, Irby DM, Carline JD, et al. A study of medical students’ speciaility-choice pathways: trying on possible selves. Acad Med 1997;72:534-41.
15. Greene AL, May JW. Applying to plastic surgery residency: factors associated with medical student career choice. Plast Reconstr Surg 2008;121:1049-53.
16. Granick MS, Blair PG, Sachdeva AK. A new educational role for plastic surgery in the fourth year of medical school. Plast Reconstr Surg 1999;103(5):1523-8.
17. Davis CR, O’Donoghue JM, McPhail J, Green AR. How to improve plastic surgery, knowledge, skills and career interest in undergraduates in one day. J Plast Reconstr Aesthet Surg 2010;63:1677-81.
18. Whither CJ. Plastic surgery? Trends for the future. Br J Plast Surg. 1970; 23:100-7.
19. Jalali M, Davies PS, Jalali M, et al. The UK plastic surgery trainee. J Plast Reconstr Aesthet Surg 2011; 64(12):1716-7.
20. Jalali M, Abood A, Flint LA, et al. Skills courses in plastic surgery: impact of enhancing confidence, skills and understanding amongst junior doctors. J Plast Reconstr Aesthet Surg 2011;64(7):976-8.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME