The use of ultrasound in hospital settings is widespread, however, while the use in aesthetic clinics is in its infancy, it’s steadily increasing [1]. This rise in popularity is a result of an increased desire for safety and accuracy of filler placements, a desire for detailed anatomical knowledge and decreasing costs of handheld ultrasound devices, such as the Clarius HD. Improved access to adequate ultrasound training has further promoted the use of ultrasound in aesthetic medicine [2].
Although most practitioners perceive the benefit to be mostly safety related, severe complications such as vascular occlusions are rare, occurring in 0.05–0.01% of treatments [3]. My use of ultrasound is mainly to plan patients’ treatments, by imaging the individual anatomy, injecting under ultrasound guidance, confirming correct filler placement, ensuring normal blood flow post treatment and observing filler changes over time.
Ultrasound can help improve anatomical knowledge and treatment planning; scanning tissue layers helps ascertain the thickness of tissue layers such as the subcutaneous layer over the parotid. Visualising these areas results in improved treatment modality selection and decreased risk for incorrect tissue targeting. Fascial planes can also be avoided, which in turn limits filler migration, dislocation and longer-term swelling. Tactile feedback can be confirmed with ultrasound, improving injectors’ skills with precise filler placement [2].
"Ultrasound can help improve anatomical knowledge and treatment planning; scanning tissue layers helps ascertain the thickness of tissue layers such as the subcutaneous layer over the parotid"
The hydrophilic nature of hyaluronic acid-based dermal fillers makes ultrasound use possible when injecting and monitoring these treatments. The hyaluronic acid is usually visible as anechoic (black) or hypoechoic (dark grey) areas in the tissue immediately after injection. With time, the hyaluronic acid’s appearance changes until it becomes difficult to discern amongst normal tissue [4]. Other fillers such as calcium hydroxylapetite (CaHA) and polymethylmethacrylate (PMMA) also have distinctive appearances within the tissues. Threads can also be visualised in the tissues as straight, hyperechoic (white) lines.
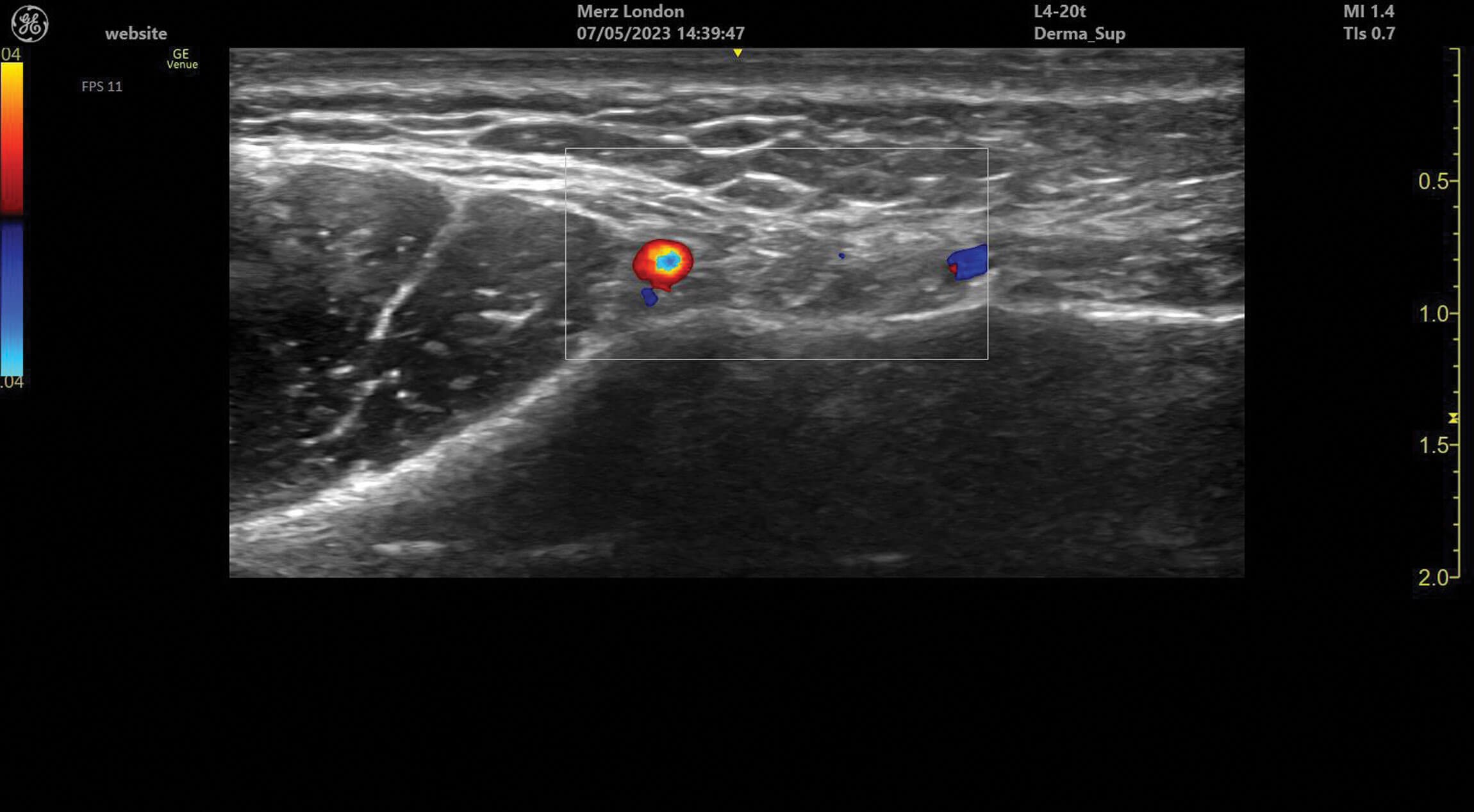
Figure 1: The facial vein and facial artery identified medial to the masseter in the facial plane of the lower face.

Figure 2: The superior labial artery running under the orbicularis oris muscle in the upper lip.
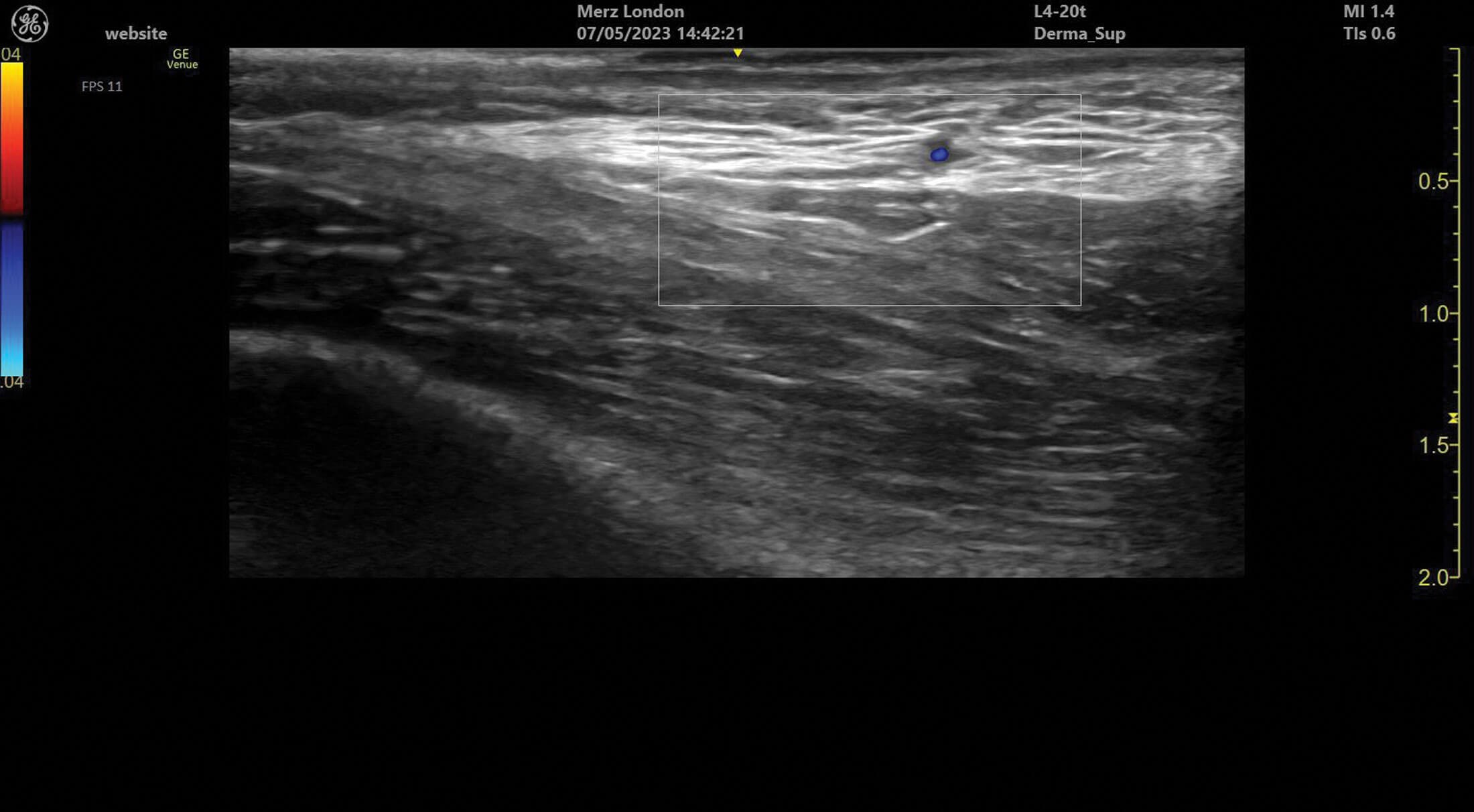
Figure 3: A branch of the superficial temporal artery in superficial tissues of the temple.

Figure 4: Scanning a patient with the Clarius handheld ultrasound device.
The visibility of dermal fillers and devices also allows for identification of prior treatments. This can be useful when consulting a new patient who has had previous filler treatments, reviewing patients who request additional filler over older filler of known or unknown composition and diagnosing long-term filler complications. Diagnosing the presence of existing fillers can assist in treatment planning and complication diagnosis and management. [1,2].
Ultrasound doppler can be used to assess blood vessel flow prior to treatments but can also help identify abnormalities in blood supply after filler treatment. Vessels can be identified and tracked in the tissue allowing for the observation of any anatomical variation. Blood vessels always appear as anechoic structures on ultrasound but, when using a colour doppler, flow can be detected either towards (red) or away (blue) from the ultrasound probe [1].
Ultrasound has been shown to help improve occlusion resolution as affected vessels can be identified and filler localised with ultrasound, allowing for improved targeting with reversal agents. This facilitates less use of reversal agents, which carry side-effects such as swelling and allergic reactions. Occlusions can also be confirmed immediately after injection without waiting for occlusion sequelae, such as mottling and crusting, to appear hours to days later. Faster resolution of occlusions benefits the patient as well as the practitioner dealing with the complication [4].
Ultrasound competence can take time to master but previous modality experience results in quicker ease of use [1]. Practice with scanning facial structures and differentiating between soft tissue layers is essential, along with formal training. I would caution against social media education as I find that self-proclaimed experts can misidentify structures on public forums, leading to misdiagnosis and mistreatment. Visualisation training is unfortunately not included with devices and can lead to treatment decisions being taken on poor quality images by unqualified practitioners. Identifying filler and even anatomical structures requires patience and hours of dedicated practice. Vascular mapping is difficult, and the lack of vessel visualisation does not exclude the presence of vascular structures, which can lead to a false sense of reassurance to inexperienced users and should always be used in conjunction with current safety advice, such as minimal bolus volumes and capillary refill assessment before and after treatment [2].
I believe the benefits far outweigh the pitfalls and ultrasound in aesthetics will only increase, and soon become the gold standard in aesthetic clinics.
References
1. Schelke LW, Decates TS, Velthuis PJ. Ultrasound to improve the safety of hyaluronic acid filler treatments. J Cosmet Dermatol 2018;17(6):1019-24.
2. Schelke L, Farber N, Swift A. Ultrasound as an Educational Tool in Facial Aesthetic Injections. Plast Reconstr Surg Glob Open 2022;10(12):e4639.
3. Schelke L, Decates T, Kadouch J, Velthuis P. Incidence of Vascular Obstruction After Filler Injections. Aesthet Surg J 2020;40(8):NP457-NP460.
4. Schelke LW, Velthuis P, Kadouch J, Swift A. Early ultrasound for diagnosis and treatment of vascular adverse events with hyaluronic acid fillers. J Am Acad Dermatol 2023;88(1):79-85.
Declaration of competing interests: Kim Booysen has been paid by Merz UK for running educational programmes and participating in research projects and, as a consultant for Merz UK, been reimbursed for attending some conferences. Kim Booysen has also been paid by Wigmore Medical and Church Pharmacy for running educational programmes.
COMMENTS ARE WELCOME









