The temporomandibular joint (TMJ) articulates the mandible to the base of the skull. Temporomandibular joint disorders (TMD) are a group of musculoskeletal syndromes affecting the TMJ and the supporting musculature. The muscles, bony articular surfaces and disc may all be involved giving rise to dysfunction and painful symptoms. The most prevalent form of TMD is myofascial; relating to the musculature. Aetiology may include malocclusion, bruxism, hypermobility or harmful habits like nail-biting. Psychological factors also play an important role in this painful condition.
Functional anatomy and supporting musculature
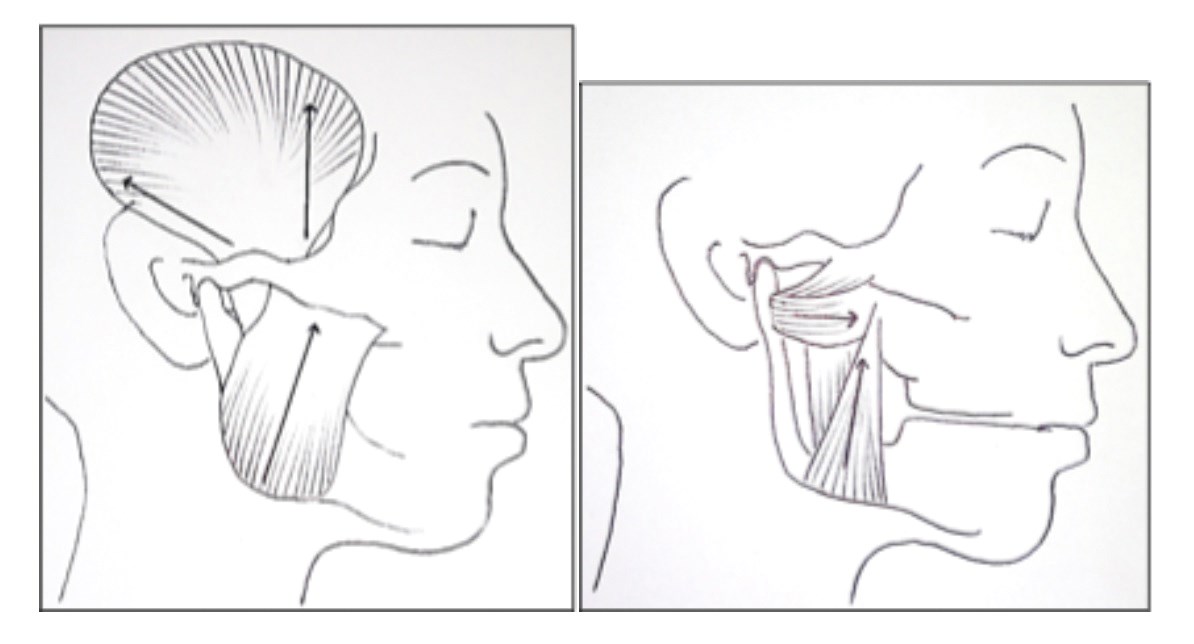
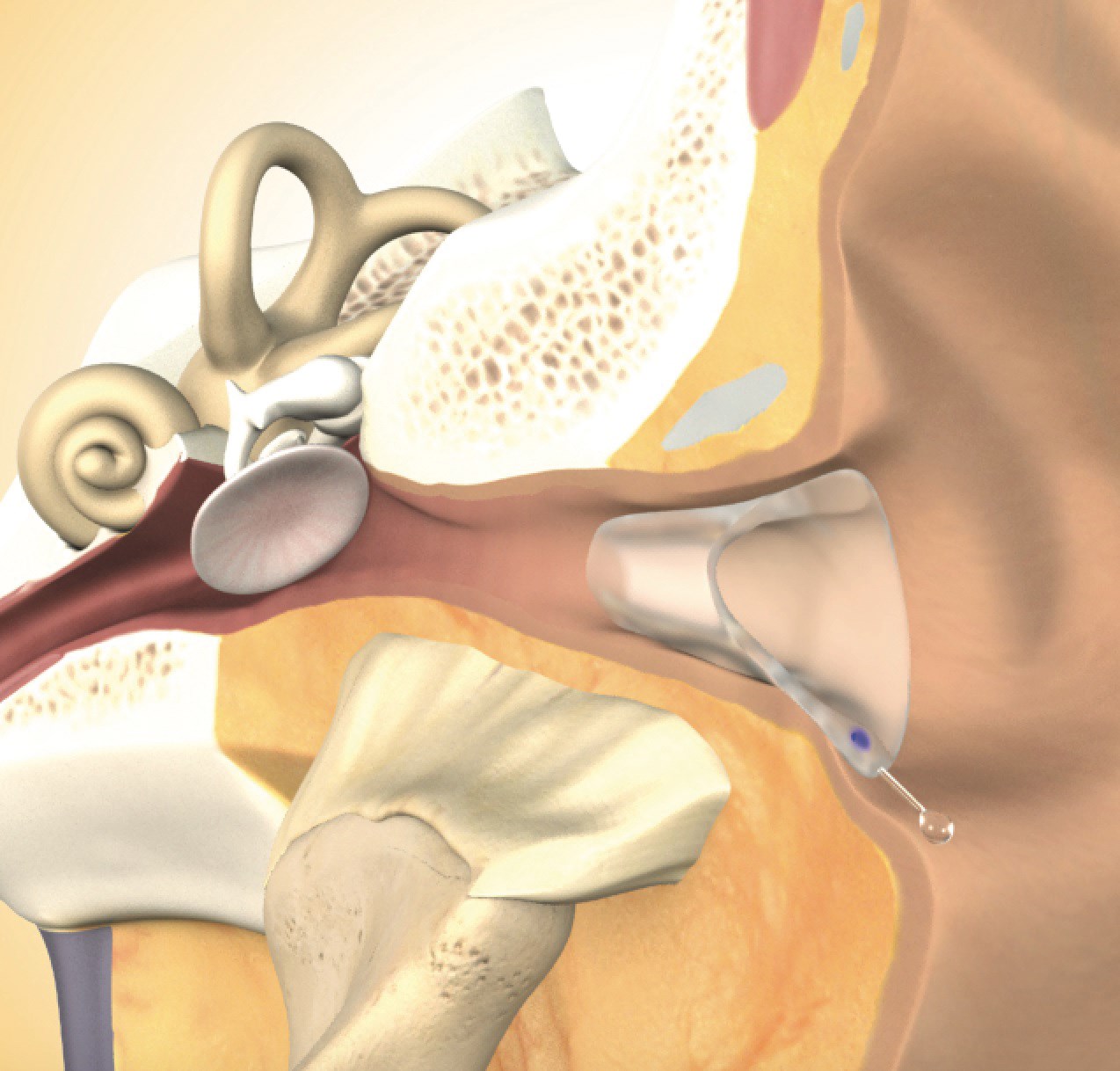
The TMJ is essentially a hinge joint divided into two by an intra-articular disc, with gliding movements. The TMJ carries out both rotation and translocation movements on opening, making this joint among the most complicated in the body (Figure 1). The articulation point at the base of the skull is the mandibular fossa. The joint is innervated by the mandibular division of the trigeminal nerve and vascular supply derived from the superficial temporal artery. The muscles of mastication are responsible for movement of the mandible and include the masseter, temporalis, medial and lateral pterygoids. The masseter elevates the mandible and attaches from the zygomatic process of the maxilla and the zygomatic arch to the lateral surface of the mandible. It is readily palpable clinically. The temporalis muscle is fanshaped and lies superficially over the temporal bone and runs deeply to the coronoid process of the mandible. It is involved in elevation of the mandible. The medial pterygoid muscle also elevates the mandible and the lateral pterygoid muscle pulls the head of the condyle out of the mandibular fossa so protruding the mandible forwards on opening (Figure 2). Due to the unique anatomy, the TMJ can be challenging to manage for the clinician and the patient.
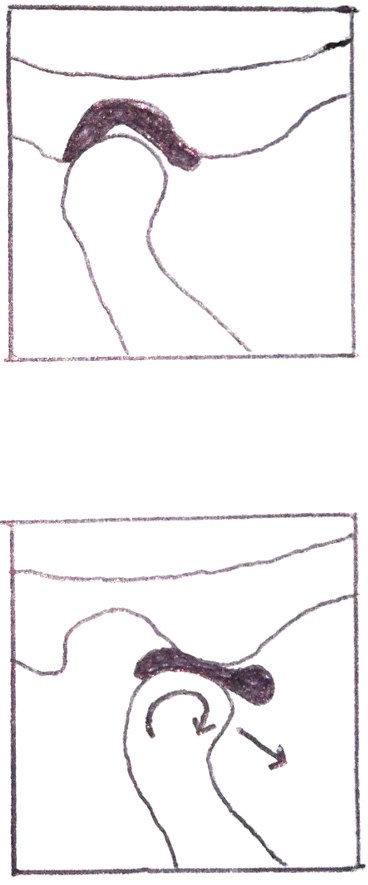
Figure 1: TMJ closed above and TMJ open below
depicting rotation and translocation of joint.
Epidemiology
TMD is the most prevalent orofacial pain of non-dental origin, with figures of up to 30% quoted in some literature [1]. It affects females more than males with peaks in middle-age. Since only a small proportion of patients seek medical help, and due to the vast diversity of symptoms, with no internationally accepted standard of diagnosis, the problem is grossly under-estimated and epidemiological data at present is inadequate [2].
Clinical diagnosis of TMD
Symptoms can be transient, modified by behaviour or persistent where an underlying psychological or somatisation disorder, such as depression, is concurrent.
Clinical symptoms are a combination of the following [3]:
- Throbbing
- Aching
- Dullness
- Mild to moderate in severity
- Localised to TMJ area
- Radiating to ear causing pain, tinnitus or fullness
- Radiating to neck
- Headaches • Unilateral or bilateral
- Usually worse in the morning
- Associated clicking, locking or trismus
- May be intermittent or continuous
- At rest or on movement
- Altered perception of occlusion.
In addition the clinical signs are:
- Crepitus
- Deviation of the jaw on opening
- Occlusal interferences
- Masseteric and temporalis hypertrophy
- Tenderness in orofacial muscles and neck muscles
- Depression or anxiety
- Poor coping skills
- Generalised pain disorders such as irritable bowel syndrome and fibromyalgia.
As there is no internationally accepted definition or standardised test for the diagnosis of TMD, at present clinicians make note of patient symptoms, clinical and dental examination, and may conduct imaging of the joint to document the presenting state. Clinical examination should include palpation of the muscles of the face and neck, trigeminal nerve testing, a detailed TMJ examination with a record of mouth opening, a pain scale and clinical photography. Dental assessment as part of differential diagnosis is pertinent as occlusal interferences or poorly fitting dentures cause imbalance on TMJs and if corrected can lead to symptom resolution. Likewise, a psychological assessment to determine comorbidities should be conducted by trained staff.
Figure 2: Left image showing position and direction of movement of temporalis and masseter muscle. Right picture (with mandible and zygomatic arch cut out) showing the two heads and direction of movement of the medial and lateral pterygoid muscles. Figure 3: Cerezen™ device in situ.
Aesthetic implications
Masseteric and temporalis hypertrophy is deemed a non-aesthetic facial shape. Acquired masseteric hypertrophy accounts for the majority of cases although a congenital form exists [4]. It occurs more frequently in Asian people [5], associated with a divergent mandible. Where bruxism leads to tooth wear, there is a significant aesthetic impact on a smile with flattened and short teeth.
Management with neuromodulators
Onabotulinum toxin A (BtxA) is a neurotoxin derived from Clostridium botulinum. It has a neuromodulatory effect on muscles predominantly by inhibiting the release of acetylcholine [6] giving atrophy [7]. It is well known that neuromuscular blocking agents are effective for the treatment of muscle hyperactivity and the associated disorders [8,9]. It can alleviate muscular pain and furthermore arthrogenic pain by reducing the functional loading of the joint. The exact mechanism of pain reduction is unclear although influencing nociceptors amongst other theories has been discussed [10].
Furthermore, injection with BtxA has been shown to cause debulking of the muscles leading to a softer curvature of the jaw line. This may be the primary reason for seeking treatment or a secondary benefit following TMD therapy. Temporalis and masseter muscles are both readily palpable and can be accessed via the transcutaneous approach. The pterygoid muscles can be approached from both intra- and extra-oral route. The latter being more technically sensitive and should only be carried out with appropriate training. Care must be taken when treating near the anterior superior margins of the masseter muscle as toxin effects on the nearby strap muscles can have adverse aesthetic effects on the smile by non-targeted zygomaticus major injection. This temporary but adverse event needs to be discussed with the patient during the consent process.
Treatment of the temporalis and the masseter muscles is sufficient for the modulation of aesthetics and relief of the articular loading forces. In some cases, treatment of the masseter alone will give the desired result. Where pain reduction is the treatment goal, it is pertinent to also inject the medial pterygoid muscle. The dose of toxin is judged by the patient stature, metabolism, level of pain and muscle size on palpation. Current literature describes a wide range of dosage used. Given the muscle atrophy caused over time, injections are performed increasingly less often. The use of BtxA is currently not Food & Drug Administration (FDA)-approved for use in TMD. But it has been effective and FDA-approved in use for disorders potentially relating to TMD such as migraine [11]. More research into the safety is required as condylar osteopenic changes have been reported in some instances post-treatment [12]. More worryingly, others have speculated a risk of bonyossification in the region of digastric muscle attachment to the mandible as it attempts to overcompensate for the atrophy in treated muscles. The combination of these events could lead to an increased risk of pathological fractures. A 2013 Cochrane review on the use of BtxA for masseteric hypertrophy highlighted the need for well-designed, high powered research [7] in order to answer these important questions.
“80% of patients with masticatory muscle hypertrophy may respond to traditional treatments, but none of these have proven sufficiently effective in managing the primary complaint of pain, which is the principle advantage in using BtxA for these cases, with the added benefit of aesthetic slimming of the face.”
Other therapies in TMD
A combination of therapies including psychological support and coping strategies, anti-anxiety medications, physiotherapy for jaw exercises, massage therapy, acupuncture and occlusal splinting have all been used. Self-care including eating soft foods, hot and cold compress and avoiding extremes of movement are recommended. For example, it would be advisable to cut an apple into smaller pieces rather than biting into it whole. General physical exercise has proven helpful in all painful conditions. Some tailored physiotherapy-guided jaw exercise to stretch and relax the muscles can provide pain relief. Psychological intervention with cognitive behavioural therapy can be effective by empowering patients to manage pain with improved coping strategies. However, a degree of mindfulness is a prerequisite for success and therefore may not suit all patients. Anti-inflammatory pain medication for short-term use may provide temporary relief. Muscle relaxants have been used rarely with limited benefit. Antidepressants at low doses have been shown to be effective in the management of chronic pain conditions. Oral appliances (occlusal splint or bite guard) are widely used in the treatment of TMD although studies have been inconclusive in their effectiveness in controlling symptoms. They are more widely regarded as being protective of teeth to reduce stress fracturing and incidence of dental filling replacement. They shouldn’t be used on a long-term basis to avoid permanent changes in occlusion. Up to 80% of patients may respond to one or a combination of these therapies [10]. Surgical reduction, arthrocentesis and arthroscopy have been used previously but patients now prefer a less invasive option [5]. None of these therapies effectively treat the primary complaint of patients which is pain and tension in the jaw muscles.
Figure 3: Cerezen™ device in situ.
New therapies
New hope for TMD sufferers is offered by a new device called Cerezen™ which comprises an inconspicuous set of custom-fitted, removable inserts worn within the auditory canal [13]. The ear inserts support the TMJ and associated secondary musculature to reduce strain and also provide ‘cognitive awareness’ (consciously or subconsciously) to the wearer (Figure 3). This encourages them to alter their para-functional habits (e.g. jaw clenching) which contributes to TMD pain, relieving strain in the area and alleviating associated symptoms. This patented device was launched in the UK in 2015 after a successful pilot clinical trial conducted in the USA where FDA approval is granted.
References
1. Schwarts M, Freund B. Treatment of temporomandibular disorders with botulinum toxin. Clin J Pain 2002;18(6):198-203.
2. Carlsson GE. Epidemiology and treatment need for temporomandibular disorders. J Orofac Pain 1999;13:232-7.
3. Zakrzewska JM. Orofacial Pain. Oxford University Press: Oxford; 2009:105-18.
4. Bas B, Muglali M, Celebi N. Treatment of masseteric hypertrophy with botulinum toxin: a report of two cases. Med Oral Patol Oral Cir Buccal 2010;15(4):e649-52.
5. Ahn J, Horn C, Blitzer A. Botulinum toxin for masseter reduction in Asian patients. Arch Facial Plastic Surg 2004;6(3):188-91.
6. Park SY, Park YW, Ji YJ, et al. Effects of botulinum toxin type A injection on the masseter muscle: An animal model study. Maxillofac Plast Reconstr Surg 2015;37:10.
7. Fedorowicz Z, van Zuuren EJ, Schoones J. Botulinum toxin for masseter hypertrophy. Cochrane Database of Systematic Reviews 2013.
8. Lee CJ, Kim SG, Kim YJ, et al. Electrophysiologic change and facial contour following botulinum toxin A. Plast Recon Surg 2007;120(3):769-78.
9. Lew MF, Brashear A, Factor S. The safety and efficacy of botulinum toxin type B in the treatment of patients with cervical dystonia: summary of three controlled clinical trials. Neurology 2000;55(12 suppl 5):29-35.
10. Bentsianov B, Francis A, Blitzer A. Botulinum toxin treatment of temporomandibular disorders, masseteric hypertrophy, and cosmetic masseter reduction. Oper Tech Otolaryngol Head Neck Surg 2004;15(2):110-3.
11. Smith HS, Audette J, Royal MA. Botulinum toxin in pain management of soft tissue syndromes. Clin J Pain 2002;18:S125-32.
12. Raphael KG, Tadinada A, Bradshaw JM, et al. Osteopenic consequences of botulinum toxin injections in the masticatory muscles: a pilot study. J Oral Rehabil 2014;41(8):555-63.
13. Jaw-dropping new treatment for TMJ disorders. Br Dent J 2015;218:364.
Declaration of competing interests: None declared.
TAKE HOME MESSAGE
-
The TMJ is a complex joint anatomically and functionally.
-
Due to the varied symptoms associated with TMD, the diagnosis of TMD is poorly defined and as such the scale of the problem is underestimated.
-
Medical, dental, facial and psychological aspects all play a role in the aetiology and presentation of TMD.
-
Neuromodulators have been used successfully in painful symptom control and aesthetic de-bulking of the masseter muscle.
-
Other therapies used to date include self-care techniques, physiotherapy, dental occlusal adjustment, anti-inflammatory pain medications, muscle relaxants, anti-depressants, occlusal splints and TMJ surgery. More recently, Cerezen has shown benefit in some patients.
-
Further research is required for the safe and effective use of neuromodulators in this common disorder.
Case report


Figure 4: Top image showing prominent masseteric enlargement before treatment.
And after treatment on the bottom, a softer angle is observable.
Figure 4 shows photographs of a 37-year-old Caucasian woman, with a tender bilateral masseteric enlargement. She was medically well with no dental or psychological implications in her presenting features. Aetiology of the hypertrophy was considered to be stress-related clenching giving myofascial TMD. Firm, well-defined masseters were palpable on clenching with focal tenderness at the centre. There was no associated temporalis or pterygoid involvement. An injection of 30 units of BtxA was made to each muscle. The patient reported reduction in pain symptoms and drastic slimming of the face as demonstrated in the clinical photographs. Clinical palpation post-treatment revealed reduction in muscle strength with high patient satisfaction levels.
COMMENTS ARE WELCOME