Can BHRT offer hope to women suffering from debilitating menopausal symptoms? Ruth Crofford, ‘the menopause nurse’, explores the evidence, safety issues and misconceptions around the therapy.
Life expectancy for women in the UK is currently 80.96 years [1]. Females in their mid forties are said to be at the average age of peri-menopause as oestrogen levels rise and fall irregularly [2]. ‘Most’ women will experience menopausal symptoms with 51 being the average age of onset.
These figures show that women can spend around a third of their lives in or around peri-menopause [1]. Although peri-menopause is not a disease state, it is of paramount importance to treat symptoms in these women due to their impact on the quality of life.
With the cultural liberation in feminine health, recent generations of menopausal women seek optimum wellness and fulfilment in both lifestyle and relationships. There is new-found freedom in openly discussing the individual menopause journey and entitlement to symptom relief [3]. In the 1980s and 90s, a significant proportion of women were on hormone replacement therapy (HRT) [4]. As the data on the risk of breast cancer emerged in the late 1990s and the publication of the Women’s Health Initiative (WHI) study [5] prescriptions for HRT decreased by 66%. Since then, women were frequently told to suffer through their symptoms [6]. Women are reporting a lack of support from their general practitioners (GPs) where their hormone health is concerned, particularly around the peri-menopause / menopause.
Consultation time in GP surgeries is limited [7] and patients are often required to make multiple attempts at persuading their prescriber that their symptoms merit hormone therapy. Alternatives to conventional care, which allow women to feel their menopausal experience is solicited, their treatment goals are heard, and they are engaged as agents in managing their own menopause are becoming popular. As a result, bioidentical hormone replacement therapy (BHRT) is presently gaining momentum in the private medical sector and being targeted as an additional service to patients within aesthetic settings.
What is HRT?
Relayed as one of the ‘government-approved’ [2] treatments for the relief of menopausal symptoms, such as hot flushes, night sweats, difficulty sleeping and reduced libido [6], there are two types of HRT in existence. Oestrogen-only therapy and combined oestrogen and progesterone therapies.
Oestrogen-only replacement therapy is appropriate for women who have had their uterus removed for non-cancerous conditions. Women who have their uterus intact will need oestrogen and progesterone replacement therapy and the latter for protection of the uterus against endometrial cancer. Traditional HRT is normally prescribed as an oral tablet or a transdermal patch. Oestrogen gels and vaginal progesterone are also available but are less commonly used.
“Consultation time in GP surgeries is limited [7] and patients are often required to make multiple attempts at persuading their prescriber that their symptoms merit hormone therapy”
How are they made?
BHRT
Bioidentical hormones are described as hormone products that are identical in molecular structure to those in the human body. They are described as ‘precise duplicates’ of hormones such as oestrone E1, oestradiol E2, oestriol E3, progesterone, dehydroepiandrosterone (DHEA), testosterone and levothyroxine, as produced by the human ovary, adrenal and thyroid [8]. They are synthesised by chemically extracting diosgenin from plants such as yams or soy. Diosgenin is chemically modified in the lab to yield the precursor progesterone, which is then used to synthesise bioidentical oestrogens and androgens [8]. Bioidentical progesterone is a natural progesterone that is micronised and hence better absorbed by the body. These chemically modified plant extracts are structurally indistinguishable from human endogenous hormones. The drugs are often compounded in a pharmacy and hence are not subject to good manufacturing process regulation. These drugs are not Food & Drug Administration (FDA) approved.
Conventional HRT
The currently available HRT products are synthetic oestrogens that mimic the hormone produced in the body. They have an identical structure to the one produced in the body. Progesterone products are of various types in conventional HRT but natural progesterone is also available as Utrogestan® or Cyclogest®.
How do the drugs / doses compare with each other?
BHRT mimics naturally produced oestrogens and is thought to be less synthetic than conventional HRT. BHRT consists of ‘compounded’ prescriptions that are specifically made up to a patient’s prescribed dose. There is also the option to make up a lot of BHRT at standard or commonly used doses and dispense them as the prescription arrives. The main advantage of BHRT is the ability to tweak a prescription to the patient’s required dose based on symptoms. Theoretically, there are fewer options with BHRT in terms of the availability of the type of progesterone as synthetic progesterone is not used in BHRT.
Conventional HRT comes in standard doses which are prepacked and dispensed by the pharmacy. They come in various permutations and combinations with an option of changing the progesterone if necessary though the oestrogen component in all of them is the same. The biggest downside is that the oestrogen and progesterone only come in standard combinations. It might take a bit of trial and error to find the most suitable drug with the least side-effects.
The prescription process
BHRT prescriptions are sent off to the compounding pharmacy and the medications are constituted based on the prescription. The compounding pharmacy has the capability to combine different drugs into one gel or lozenges though most practitioners would prefer to keep them separate so they can be individually stopped if necessary. This has been the most controversial aspect of BHRT, as they use commercially available drugs to compound the prescriptions. The safety of these drugs in themselves have been tested but not necessarily the mixture of these drugs, especially as gels and lozenges. There are also concerns over standards of manufacturing as some of these ‘specialised pharmacies’ remain unregulated or monitored by the Medicines and Healthcare products Regulatory Agency (MHRA). Much apprehension has been voiced by internationally recognised bodies including the British Menopause Society, who continue to petition for their regulation.
HRT, available on the National Health Service (NHS) and a recognised part of mainstream medicine, is dispensed like any other prescription in a pharmacy.
Is BHRT available on the NHS?
There is a strong misconception that BHRT is only available in private medical settings within the UK. However, all oestrogens that are available on the medicines formulary are bioidentical or body identical hormones. They are often mixed with synthetic progesterone but micronised natural progesterone is also available on the formulary. A natural oestrogen tablet, gel or patch can be combined with micronised progesterone to get BHRT. It is a false belief that HRT is synthetic and bioidentical hormones are not; although BHRT is derived from plant oestrogens they then undergo a process in the lab to convert them into oestrogens.
There is a difference in the availability of hormones on the NHS. DHEA is determined as an essential pre-cursor hormone, with an alleged potential to increase bone density, improve sexual function and decrease body fat. The local application of DHEA has been clinically trialled and there is evidence to suggest it improves vaginal atrophy, a classical problem during menopause [9]. To date, no serious adverse events have ever been reported (worldwide) from the use of DHEA.
Private hormone care also gives patients an opportunity to have a wider choice of routes of administration and to explicably share their preferences for medication. A combination of four hormones can be blended in a transdermal ‘carrier’ cream for topical administration. This enables compliance and simplifies a regimen.
These prescriptions are made to order in private compounding pharmacies. They are tailor-made to fulfil the individual’s prescription. This is in direct contrast to the standardised dosing of traditional HRT.
Is there any difference in the consultation process and prescription?
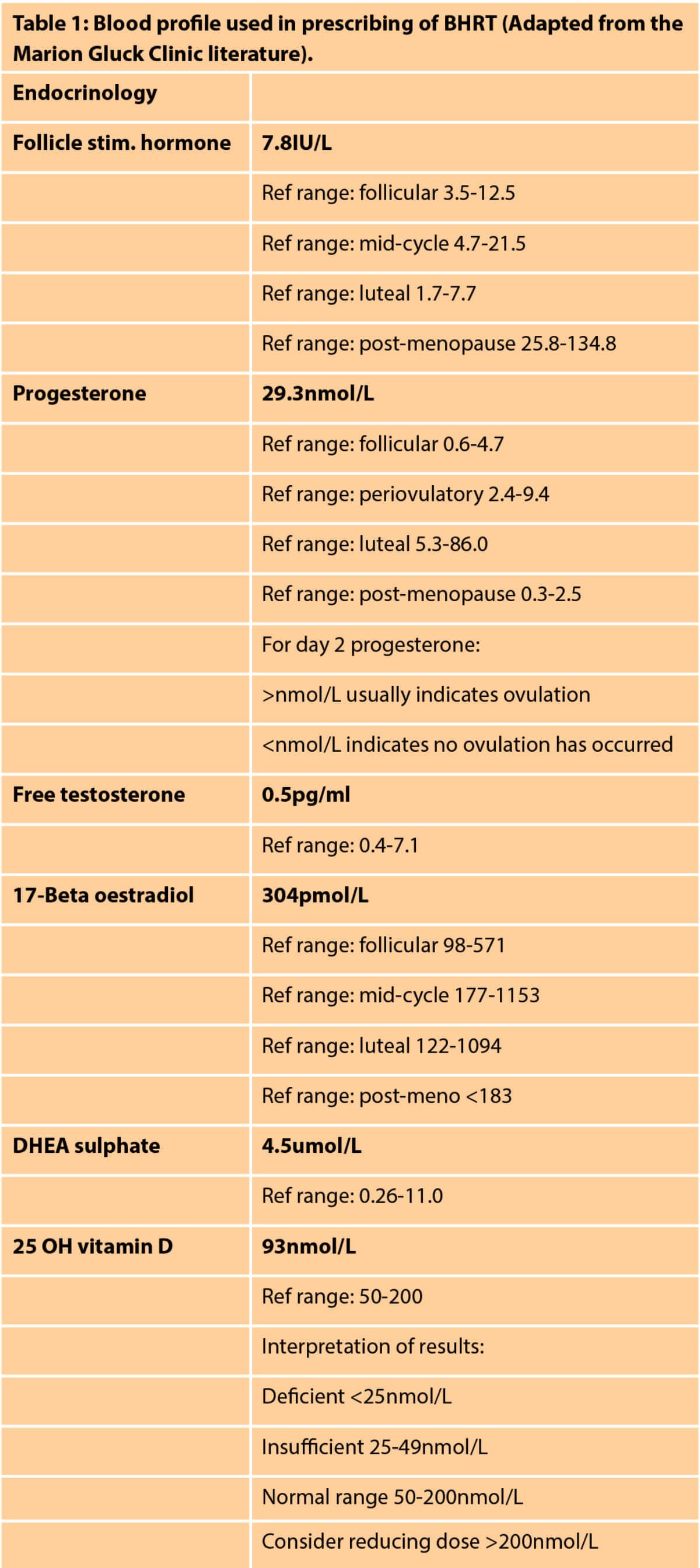
With BHRT, in the first instance, a consultation is offered to give a comprehensive symptom-checker [10]. This symptom checker will help to determine an individual’s therapy. Blood tests are then performed to understand the hormonal profile (Table 1).
It should be noted that premises wishing to take blood samples must be Care Quality Commision (CQC) registered. The approach in BHRT is to restore hormone balance and to actualise a feeling of wellbeing. It aims to provide freedom from the vasomotor symptoms of oestrogen depletion with the addition of endometrial protection (where required), as well as examining the psychological, sexual and social aspects of symptoms. Since BHRT of this type is available in the private sector only, patients feel that their problems are heard and solutions are provided to target the problems.
Consultations for conventional HRT emphasise the risks and contraindications for HRT. There is generally very little guidance or awareness on the type of progesterone that is necessary to address the symptoms of menopause or side-effects of HRT.
“BHRT consists of ‘compounded’ prescriptions that are specifically made up to a patient’s prescribed dose”
How are hormone levels tested in BHRT?
Blood tests can be used to measure the total amount of oestradiol, oestriol and 17-ß oestradiol from all sources in the body. Patients on BHRT have regular blood tests and the oestrogen dose is regulated to control symptoms, while progesterone is often administered to achieve 1/10th of the levels of oestradiol. DHEA and testosterone levels are measured to ensure that the normal levels in women are not exceeded, however, there is considerable uncertainty surrounding what the normal levels of testosterone in women actually are. Saliva testing has not been recommended as there is not rigorous data to substantiate the use of such expensive tests [11].
In conventional HRT, patients would not routinely be offered blood testing as the dosage and treatments are based on symptoms rather than blood tests.
What are the advantages of BHRT over conventional HRT?
With BHRT lower doses of natural progesterone are available compared to conventional HRT. DHEA and testosterone are also available at doses pertinent to the symptoms. With conventional HRT testosterone gel is not FDA approved for use in women. Hence many practitioners are not keen on prescribing the gel despite women suffering from lack of energy and libido even after starting oestrogen and progesterone replacement therapy. DHEA gel is not available in the market for systemic use; vaginal DHEA has just been approved for vulvovaginal atrophy and hopefully will be available soon.
What are the advantages of conventional HRT over BHRT?
Conventional HRT comes in standard doses. It is not possible to reduce the dose of progesterone below a certain level. However, there are alternatives available which might suit some patients better. The production, sale and prescription of conventional HRT are highly regulated and its safety is well established.
What do the experts think of BHRT?
The American Menopause Society and the British Menopause Society have raised concerns about BHRT, not due to the medications used or prescription of drugs, but due to the lack of control over the production process [11,12].
Why do women want BHRT?
Though some patients are on BHRT the overall market share for BHRT is currently a lot smaller than conventional HRT. Many studies have looked at the reasons for women requesting BHRT. It is clear that there is a false notion that hormones which are natural are a lot safer compared to conventional HRT. This has led to the impression among women that there is a reduction in breast and endometrial cancer or a reduction in the incidence of stroke and deep vein thrombosis with BHRT.
Most women who have BHRT consultations want to feel that they are heard and their symptoms are acknowledged. They don’t want merely to be dismissed as menopausal symptoms, these can have a serious impact quality of life. Often BHRT prescribers are there to give the time and education that is necessary to manage these patients. Unfortunately, the NHS struggles to provide such care, especially in primary care.
Conclusion
RD Langer urges us to learn pertinent lessons from the WHI, that HRT affects organ systems widely according to age, treatment regimens, and time since last physiologic exposure to hormones [13]. The Advertising Standards Agency (ASA) counsels’ patients to be cautious of claims over safety, or ‘natural alternatives’ marketed to women by purveyors of BHRT. They condemn advertising which gives unfounded securities and does not condone the purchase of preparations such as progesterone cream on the internet.
We need investment from a major pharmaceutical company to do the necessary research into the efficacy and potential side-effects of BHRT before it becomes seen as a panacea for all menopausal symptoms.
If GPs were to become more familiar with the wording of hormones as ‘body identical’ and make patients aware of their availability in the licensed HRT form, then the demand for bioidentical hormones in private care setting would probably reduce. Patients are currently viewing the private hormone market as more trustworthy and effective with a lower risk profile. Greater investment in patient time is needed in primary care, along with a more holistic approach, for example, to include more liberal prescribing of off-label testosterone for sexual dysfunction during the menopause.
References
1. The King’s Fund. What is happening to life expectancy in the UK? 2018.
www.kingsfund.org.uk/publications/
whats-happening-life-expectancy-uk
[Accessed 25 June 2019].
2. The North American Menopause Society. How Do I Know I’m in Menopause?
www.menopause.org/for-women/
menopauseflashes/menopause
-symptoms-and-treatments/
how-do-i-know-i’m-in-menopause
[Accessed 25 June 2019].
3. Holtorf K. The bioidentical hormone debate: are bioidentical hormones (estradiol, estriol, and progesterone) safer or more efficacious than commonly used synthetic versions in hormone replacement therapy? Postgrad Med 2009;121(1):73-85.
4. Fishman JR, Flatt MA, Settersten RA. Bioidentical hormones, menopausal women, and the lure of the “natural” in U.S. anti-aging medicine. Soc Sci Med 2015;132:79-87.
5. Silverman BG, Kokia ES. Use of hormone replacement therapy, 1998-2007: sustained impact of the Women’s Health Initiative findings. Ann Pharmacother 2009;43(2):251-8.
6. Gluck M, Edgson V. It Must Be My Hormones. Michael Joseph; 2017.
7. Connolly A, Britton A. Women’s Health in Primary Care. Cambridge University Press; 2017.
8. Cirigliano M. Bioidentical hormone therapy: a review of the evidence. J Womens Health 2007;16(5):600-31.
9. Labrie F. DHEA, important source of sex steroids in men and even more in women. Prog Brain Res 2010;182:97-148.
10. Dilks A, Soos E. Bioidentical hormone replacement therapy: implications for practice. J Aesthetic Nurs 2019;8(4):166-71.
11. British Menopause Society. BMS council issues a consensus statement on bioidentical hormones. 2017.
https://thebms.org.uk/2017/03/
bms-council-issues-consensus
-statement-bioidentical-hormones/
[Accessed 25 June 2019].
12. de Villiers TJ, Hall JE, Pinkerton JV, et al. Revised global consensus statement on menopausal hormone therapy. Maturitas 2016;91:153-5.
13. Langer RD. The evidence base for HRT: what can we believe? Climacteric 2017;20(2):91-6.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME






