Umbilical cord lining (UCL) mesenchymal stem cells (MSC) produce proteins and growth factors that, when packaged into exosomes in fixed proportions, can stimulate repair and regeneration in recipient cells. The pleiotropic properties of UCL-MSC have been shown to be effective in treating several medical conditions, including hair loss. In vitro analyses of hair follicles exposed to red deer UCL-MSC exosomal proteins demonstrated increased cellular proliferation and decreased inflammation markers of the dermal papilla.
In human studies, topical application of red deer UCL-MSC exosomal proteins to the scalp of a patient suffering post COVID-19 telogen effluvium was shown to result in hair regrowth. Similar positive results were demonstrated when using red deer UCL-MSC exosomal proteins after microneedling in males and females suffering from androgenetic alopecia as well as alopecia areata. A small pilot study in 10 patients treated with red deer UCL-MSC exosomal proteins after microneedling demonstrated an increase in total hair count and hair calibre, with a decrease in interfollicular distance after 12 weeks. Overall, red deer UCL-MSC exosomal proteins may promote hair growth by reducing inflammation and restoring a healthy hair cycle, as well as by stimulating regeneration processes in the dermal papilla cells.
Introduction
Exosomes are small, vesicles produced by all cell types [1]. Originally thought to be the cell’s ‘rubbish bin’ [2], these membrane-bound particles, containing a variety of molecules such as cytokines, growth factors, peptides, lipids, and nucleic acids, are now known to be important mediators of intercellular communications [2]. In vitro, exosomes can be released from cultured cells in the culture media. This ‘conditioned media’ containing exosomes can then be collected and evaluated for various therapeutic applications.
The proportion of cytokines and growth factors contained in exosomes is specific to the cell type from which they are produced [3]. The UCL is a rich source of both mesenchymal and epithelial stem cells that secrete exosomes promoting cellular repair, regeneration and renewal [4]. Stem cell-derived exosomes offer important advantages over stem cells, e.g., less immunogenicity, less potential oncologic complications and stability for long-term storage and transportation [5]. Early studies demonstrated that stem-cell derived exosomes accelerated healing in a variety of wounds, and in the US, human UCL-MSC exosomes are now entering phase two trials [6] with the Food and Drug Administration (FDA) for treatment of chronic diabetic foot ulcers.
A study comparing conditioned media from red-deer UCL-MSC with that from cultured human UCL-MSC, showed that both could significantly and equally stimulate human dermal fibroblast growth and cell proliferation in-vitro (Figure 1). This suggested that mammalian cytokines and growth factors work across different mammalian species.
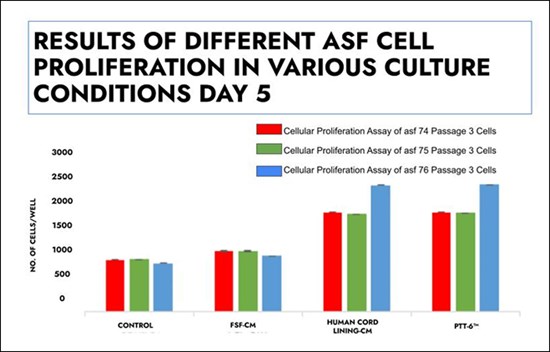
Figure 1: Cell proliferation assay of adult skin fibroblasts 74, 75 and 76 Passage 3 cells in different culture conditions on day five, demonstrating similar levels of proliferation in fibroblasts exposed to human and red deer (PTT-6) UCL-MSC exosomal proteins in conditioned media.
Using the European Commission Cosmetic Ingredients (CosIng) reference database [7], a formulation containing red deer UCL-MSC conditioned media with released exosomal proteins was developed for cosmeceutical purposes, both as a serum and combined with a transepidermal excipient. Exposure of dermal fibroblasts from individuals of different ages to red deer UCL-MSC exosomal proteins in vitro demonstrated increased fibroblast production of elastin and hyaluronic acid [8]. Clinical trials further showed red deer UCL-MSC exosomal proteins in a transepidermal excipient cream to be effective in skin rejuvenation as evaluated by investigator and subject assessments [9]. Finally, application of red deer UCL-MSC exosomal proteins to the face after ablative laser facial resurfacing also resulted in decreased post-procedural facial erythema, accelerated healing and improvement in facial wrinkling [10].
Here we present evidence of the applicability, safety and efficacy of red deer UCL-MSC exosomes for the treatment of hair loss.
Alopecia case reports and case series
Telogen effluvium
A 30-year-old patient who recovered from COVID-19 infection developed acute telogen effluvium hair loss. He was unresponsive to topical minoxidil and daily LED treatments. Red deer UCL-MSC exosomal proteins applied to the scalp at monthly intervals resulted in hair regrowth and hair density improvement [11] (Figure 2).

Figure 2: Before (left) and three months after (right) treatment using red deer UCL-MSC exosomal
proteins at monthly intervals on a patient suffering from telogen effluvium in Singapore.
Androgenetic alopecia
In a case series of 60 patients on medical alopecia therapy it was noted that a majority of patients showed signs of erythema indicative of scalp inflammation. To suppress inflammation, red deer UCL-MSC exosomal proteins were applied topically to the scalp following microneedling. Hair regrowth and improved hair calibre and density occurred in over 95% of the patients with no adverse effects reported [12] (Figure 3).

Figure 3: Treatment of androgenetic alopecia using red deer UCL-MSC exosomal proteins
with a microneedling device. Courtesy of Dr Michelle Ng, Hong Kong.
A London-based trichologist treated male and female androgenetic alopecia with weekly applications of red deer UCL-MSC exosomal proteins following microneedling. She found hair regrowth and improvements in hair density and calibre up to six months after treatment. Notably she also observed re-pigmentation in areas of greying. Similar results were observed using similar treatment protocols in Singapore and Australia [13] (Figure 4).
Figure 4a-c: Results on the treatment of androgenetic alopecia using red deer UCL-MSC exosomal
proteins after six weeks from doctors in London, Australia and Singapore, respectively.
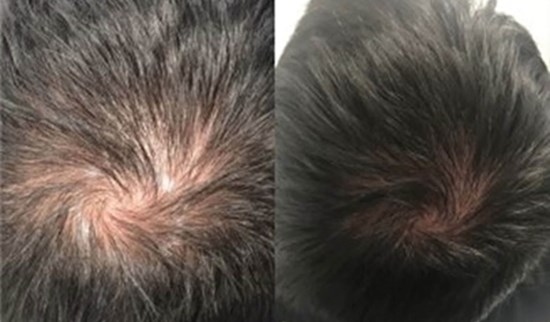
Figure 4a: Courtesy of Ms Kelly Morrell, London.

Figure 4b: Courtesy of Dr Mathew Jafarzadeh, Australia.
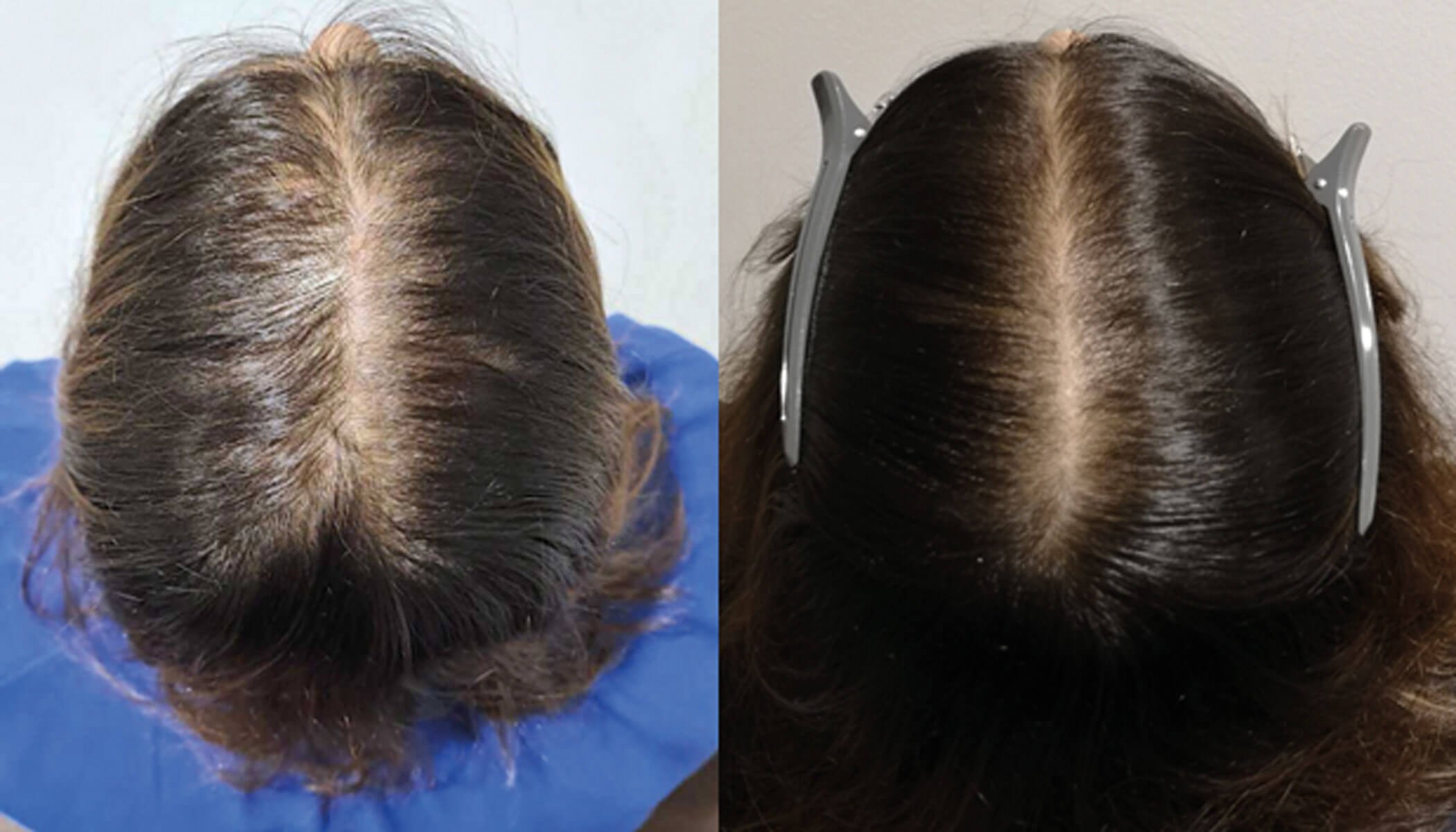
Figure 4c: Courtesy of Ms Fazilah Iqbal, Singapore.
A study in 10 patients with androgenetic alopecia treated weekly with application of red deer UCL-MSC exosomal proteins following microneedling of the scalp demonstrated significant amplification of the follicular units per cm [2] (P <.05), with decreased inter-follicular distance (P <.05) as documented in phototrichograms after 12 weeks. Density and total hair count per cm [2] increased (P <.05), as did the sum of hair width per cm [2] (P <.05) [14].
Alopecia areata
A patient with alopecia areata treated with red deer UCL-MSC exosomal proteins following microneedling experienced complete hair regrowth after six weekly treatments [15] (Figure 5).

Figure 5: Alopecia areata treated with weekly micro needling sessions and application of red deer UCL-MSC exosomal proteins for six weeks. Images were taken pre-treatment, six sessions and four months later, and eight sessions and eight months later. Courtesy of Ms Kelly Morrell, London.
In vitro analyses
In vitro, dermal papilla cells incubated with red deer UCL-MSC exosomal proteins showed a 24% increase in cell proliferation, similar to that observed with minoxidil at 2µg/ml [16].
Moreover, proinflammatory cytokine tumour necrosis factor alpha (TNF-α) levels were reduced by 30-fold when dermal papilla cells were exposed to red deer UCL-MSC exosomal proteins, an effect which was similar to suppression of inflammation with Vitamin D [16].
Discussion
Stem cells exert effects on cell regeneration and repair by stimulating cell proliferation and accelerating apoptotic programs in senescent cells [17]. In the classic example of wound re-epithelisation, stem cells at the follicular bulge area stimulate keratinocyte outgrowth, and peri-wound stem cells stimulate skin cells to depolarise and migrate to cover the wound [18]. In the hair follicle, similar mechanisms might be at play to activate dermal papilla cells thereby stimulating proliferation and lengthening of the hair shaft [19].
Many anti-inflammatory cytokine mediators, such as IL-10 and TGF-β [20], have been detected in the stem cell secretome. UCL-MSC themselves express HLA-E and HLA-G with immunosuppressive functions [21]. HLA-E inhibits natural killer cell cytotoxicity [22], and HLA-G has a key role in fetal-maternal tolerance [23]. Originally found only in the placenta, it has also been detected in UCL-MSC [24,25].
Anti-inflammatory effects of UCL-MSC were examined in Faslpr mice who spontaneously develop systemic lupus erythematosus (SLE).Intraperitoneal implantation of UCL-MSC increased survival and decreased the severity of lupus nephritis by modulating both innate and adaptive immune systems [26].
Wounds become indolent in the face of toxic inflammation [27]. Suppression of toxic inflammation promulgated by M2 macrophages [28] which have a key role in controlling the immune system [29] may reverse a wound from an indolent to closable [30].
The finding that red deer UCL-MSC exosomal proteins could suppress inflammation as effectively as vitamin D with resultant increase in hair growth from reactivation of dormant hair follicles in the telogen phase suggests that (1) active inflammation at the dermal papilla suppresses hair growth [31] and (2) suppression of inflammation allows hair regrowth [32].
Overall, the mechanism of action of UCL-MSC exosomal proteins on hair regrowth appear to be similar to wound healing, namely suppression of inflammation and stimulation of cell proliferation. Further study is required to elucidate this potentially two-prong mechanism of action of UCL-MSC exosomal proteins where there is simultaneous stimulation of cell proliferation and suppression of toxic inflammation. Larger controlled trials are also required to assess the effects of red deer UCL-MSC on hair regrowth.
References
1. Ludwig A, Giebel B. Exosomes: small vesicles participating in intercellular communication. Int J Biochem Cell Biol 2012;44(1):11-5.
2. Shrivastava S, Morris K. The Multifunctionality of Exosomes; from the Garbage Bin of the Cell to a Next Generation Gene and Cellular Therapy. Genes (Basel) 2021;12(2):173.
3. Yin K, Wang S, Zhao R. Exosomes from mesenchymal stem/stromal cells: a new therapeutic paradigm. Biomark Res 2019;7:8.
4. Lim I, Phan TT. Epithelial and Mesenchymal Stem Cells From the Umbilical Cord Lining Membrane. Cell Transplant 2014;23(4-5):497-503.
5. Zhang K, Cheng K. Stem cell-derived exosome versus stem cell therapy. Nat Rev Bioeng 2023;1:608-9.
6. Phase 1, Open-Label Safety Study of Umbilical Cord Lining Mesenchymal Stem Cells (Corlicyte®) To Heal Chronic Diabetic Foot Ulcers (2022). ClinicalTrials.gov.
https://classic.clinicaltrials.gov/
ct2/show/NCT04104451
7. Cosmetic Ingredient Database. European Commission.
https://single-market-economy.ec
.europa.eu/sectors/cosmetics/
cosmetic-ingredient-database_en
8. Ong C, Lim I, Goldman M, et al. Improvement in Skin Elasticity Using Red Deer Umbilical Cord Lining Mesenchymal Stem Cell Conditioned Media. J Drugs Dermatol 2023;22(1):82-9.
9. Alhaddad M, Boen M, Wu D, et al. Red Deer Umbilical Cord Lining Mesenchymal Stem Cell Extract Cream for Rejuvenation of the Face. J Drugs Dermatol 2019;18(4):363-6.
10. Hoss E, Kollipara R, Alhaddad M, et al. Red Deer Umbilical Cord-Derived Stem Cell Conditioned Media Combined With Ablative Resurfacing of the Face. J Drugs Dermatol 2020;19(11):1044-8.
11. Ong S, Ong K, Lee S. COVID-19-induced Scalp Alopecia Treated Effectively with Stem Cell Serum. Plast Reconstr Surg Glob Open 2022;10(6):4423e
12. Ng M. Umbilical Cord Lining Mesenchymal Exosomes with Microneedling for Scalp Rejuvenation [presentation]. World Congress of Dermatology, Singapore 2023.
https://www.wcd2023singapore-abs.org/
abstract_details.php?aid=3159
13. Jafardazeh M. World Congress for Hair Research, Australia, 2022.
14. Duschek N, Prinz V, Cajkovsky M. PTT-6, a novel topical hair serum with stem cell growth factors significantly increases hair growth in patients with hair loss – a 12-week prospective, open-label Case series (2023). The Private Clinic.
https://www.theprivateclinic.co.uk/
wp-content/uploads/2023/05/PTT-6
-novel-topical-hair-serum-with-stem-cell
-growth-factors-significantly-increases-hair
-growth-in-patients-with-hair-loss-12-week
-prospective-open-label-case-series.pdf
15. Morrell K. Unpublished Information (2023).
16. CellResearch Corporation Internal Data (2022).
17. Murphy M, Moncivais K, Caplan AI. Mesenchymal stem cells: environmentally responsive therapeutics for regenerative medicine. Exp Mol Med 2013;45(11):54.
18. Baraniak P, McDevitt T. Stem cell paracrine actions and tissue regeneration. Regen Med 2010;5(1):121-43.
19. Kwack M, Seo C, Gangadaran P, et al. Exosomes derived from human dermal papilla cells promote hair growth in cultured human hair follicles and augment the hair-inductive capacity of cultured dermal papilla spheres. Exp Dermatol 2019;28(7):854-7.
20. Sanjabi S, Zenewicz L, Kamanaka M, et al. Anti-inflammatory and pro-inflammatory roles of TGF-beta, IL-10, and IL-22 in immunity and autoimmunity. Curr Opin Pharmacol 2009;9(4):447-53.
21. Shang Y, Guan H, Zhou F. Biological Characteristics of Umbilical Cord Mesenchymal Stem Cells and Its Therapeutic Potential for Hematological Disorders. Front Cell Dev Biol 2021;9:570179.
22. Kamiya T, Seow S, Wong D, et al. Blocking expression of inhibitory receptor NKG2A overcomes tumor resistance to NK cells. J Clin Invest 2019;129(5):2094-106.
23. Dudek N, Purcell A. Repertoire of Nonclassical MHC 1 (HLA-E, HLA-F, HLA-G, and Orthologues). Encyclopedia of Immunobiology 2016;2:215-9.
24. Zhou Y, Gan S, Lin G, et al. Characterization of Human Umbilical Cord Lining-Derived Epithelial Cells and Transplantation Potential. Cell Transplant 2011;20(11-12):1827-41.
25. Abbasi B, Shamsasenjan K, Ahmadi M, et al. Mesenchymal stem cells and natural killer cells interaction mechanisms and potential clinical applications. Stem Cell Res Ther 2022;13(1):97.
26. Chua A, Guo D, Tan J, et al. Intraperitoneally Delivered Umbilical Cord Lining Mesenchymal Stromal Cells Improve Survival and Kidney Function in Murine Lupus via Myeloid Pathway Targeting. Int J Mol Sci 2023;24(1):365.
27. Zhao R, Liang H, Clarke E, et al. Inflammation in Chronic Wounds. Int J Mol Sci 2016;17(12):2085.
28. Arabpour M, Saghazadeh A, Rezaei N. Anti-inflammatory and M2 macrophage polarization-promoting effect of mesenchymal stem cell-derived exosomes. Int Immunopharmacol 2021;97:107823.
29. Roszer T. Understanding the Mysterious M2 Macrophage through Activation Markers and Effector Mechanisms. Mediators Inflamm 2015;2015:816460.
30. Kim S, Nair M. Macrophages in wound healing: activation and plasticity. Immuno Cell Biol 2019;97(3):258-67.
31. Olayinka J, Richmond J. Immunopathogenesis of alopecia areata. Curr Res Immunol 2021;2:7-11.
32. Peyravian N, Deo S, Daunert S, et al. The Inflammatory Aspect of Male and Female Pattern Hair Loss. J Inflamm Res 2020;13:879-81.
Declaration of competing interests: Dr Ivor Lim is co-founder and medical director of CellResearch Consumer Health Pte. Ltd. and CellResearch Corporation (parent company of CellResearch Consumer Health Pte. Ltd.); Laura Thompson is an employee of CellResearch Corporation.
COMMENTS ARE WELCOME