Introduction
Male to female transgender patients often undergo reduction thyroplasty – a procedure to reduce the external appearance of the thyroid cartilage of the larynx, and feminisation of the voice. Reduction thyroplasty, often erroneously called ‘tracheal shave’, is one of the earliest procedures requested by transgender patients, as it is a procedure classed under facial feminisation. Around the world, reduction thyroplasty is carried out in conjunction with procedures aimed at raising the pitch of the voice.
These surgeries are varied and include:
- Cricothyroid approximation suturing of the cricoid cartilage to the thyroid cartilage thus creating a cricothyroid muscle-like action; elongating and tensing the vocal cords.
- De-epithelialisation of the anterior commissure; induces laryngeal webbing and resulting in a ‘breathier voice’ as well as shortening the vibrating section of vocal cords.
There is no long-term evidence for these procedures, and presently speech and language therapy is the safest, most effective option for feminising the voice and communication behaviours [1].
Reduction thyroplasty is a cosmetic procedure to reduce the prominence of the thyroid notch. It is technically a straightforward procedure, so long that care is taken not to damage the endolarygael structures.
Preparation
Preoperatively patients should have a detailed discussion of surgery to ensure their expectations are realistic. Some patients will have an idea of someone they would like to look like as opposed to what can realistically be achieved in their circumstances. Medical photography for documentation is essential and can be used to guide discussion. It is common for there to be anxiety about admission to hospital and being placed in a male communal room. For this reason, we admit all patients to a single room. Many patients will be on hormonal therapy and we stop oestrogen products four weeks prior to surgery and use compression stockings for the perioperative period.
Procedure
It is helpful to extend the neck with a shoulder bag and stabilise the head in a head ring. The incision is made in a skin crease overlying the thyroid lamina. It is advantageous to mark this with a sterile marker and inspect it from the head of the table to ensure symmetry. Flaps are raised in the subplatysmal plane accepting that the platysma is deficient in the midline. The infrahyoid strap muscles are then separated to skeletonise the larynx (Figure 1). Minimal dissection is performed superior to the thyroid lamina to avoid damage to the superior thyroid nerve and artery as they pierce the thyrohyoid membrane. The thyroid lamina is marked halfway between the thyroid notch and the inferior edge of the thyroid cartilage. Here, the vocal cords insert on to its posterior surface. All planned incisions are now placed superior to this point (Figure 1).
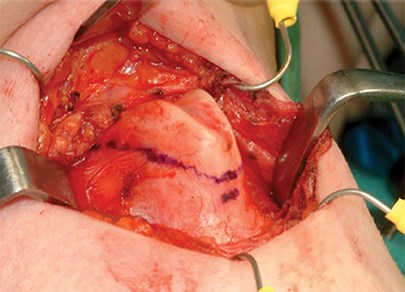
Figure 1: Skeletonisation of the anterior larynx.
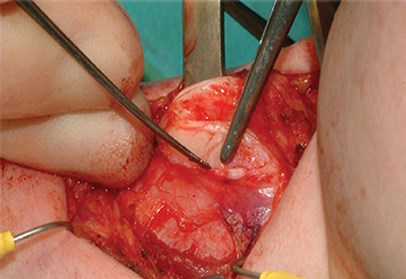
Figure 2: Elevation of the perichondrium.
The perichondrium is carefully elevated by incising it over the superior edge of the thyroid lamina, then raising it using a Lempert elevator (Figure 2). This is carried out on the lateral and medial surface of the thyroid lamina. Great care is taken medially to avoid any damage to the laryngeal contents. The handle of the elevator is now placed medial to the cartilage and scalpel is used to cut on to the elevator. This can be difficult if differential ossification of the cartilage has taken place and it is helpful to use mayo scissors or a cutting drill burr to complete the incisions. The cartilage is now hinged anteriorly (Figure 3) and it too, after careful inspection medially to ensure no damage to the glottis, can be removed also using the scissors. The resultant reduced thyroid cartilage can now be smoothed and contoured using a large diamond burr drill (Figure 4). It is important to use irrigation.
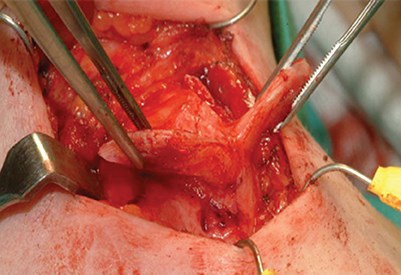
Figure 3: Cartilage about to be removed now hinged anteriorly.
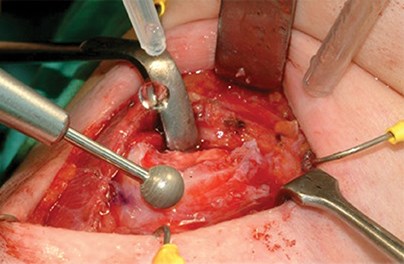
Figure 4: Smoothing and contouring of cartilage using diamond burr.
The perichondrium is then replaced and sutured. The strap muscles are re-approximated and the skin is closed. Our preference for closure is skin clips for four days. The patient is reviewed at six weeks and then, three months. Postoperative photographs are obtained. Patients do need to understand they will be left with an anterior neck scar, but many find this is preferable to, and easier to camouflage than, a prominent thyroid cartilage.

Figure 5: Pre and postoperative result three months later.
Complications
These include wound problems – infection or skin tethering; and laryngeal problems – damage to the endolaryngeal structures – this can produce temporary or permanent hoarseness. This is avoided by not placing cartilaginous incisions too inferiorly. A systemic complication, deep venous thrombosis in patients on oestrogen supplementation is a recognised problem. Finally, as with all cosmetic procedures, there is a risk that the patient may not be satisfied with their appearance postoperatively. In these situations, we would recommend careful consideration before offering revision surgery.
Postoperative care
We monitor all patients overnight following their procedure and discharge them home the following day. This is to ensure no problems with the voice, neck or surgical emphysema and the wound is satisfactory prior to discharge.
Conclusion
Reduction thyroplasty is a key procedure in facial feminisation. It is important to treat these patients sensitively from the outset and acknowledge any concerns they have about hospitalisation. The procedure is straightforward; however, it is important to avoid damaging the anterior attachments of the vocal cords.
References
1. Spiegel JH. Phonosurgery for pitch alteration: Feminisation and masculisation of the voice. Otolaryngol Clin N Am 2006;39(1):77-86.
Declaration of competing interests: None declared.
COMMENTS ARE WELCOME





